
What are the four stages of pressure ulcers?
· How Should You Treat a Stage 1 Pressure Ulcer? If you believe that you have a stage 1 pressure ulcer, you should remove all pressure from the area. Keep the area as dry and clean as possible to prevent bacterial infections. To speed up the healing process, you should eat adequate calories and have a diet high in minerals, proteins, and vitamins. Zinc, iron, vitamin …
How to treat a stage 3 pressure ulcer?
The treatment for the pressure ulcer depends on the stage and condition of your ulcer. It includes: Try to move and regularly change your position to remove the pressure from the sore. You can use foam pads or pillows or dynamic mattresses and …
What is the best treatment for a pressure ulcer?
TREATMENT Cleaning and debridement. Cleaning of the wound and meticulous skin care are the most essential part of the treatment. Wound dressings. The dressing used for various stages of wound healing is specialised for every stage; in fact …
What are the stages of a pressure ulcer?
· Wound cleansing, preferably with normal saline and appropriate dressings, is a mainstay of treatment for clean ulcers and after debridement. Bacterial load can be managed with cleansing. Topical...

What type of dressing is used on a Stage 1 pressure ulcer?
Thin hydrocolloid dressings (eg DuoDERM® SignalTM and DuoDERM® Extra Thin) are increasingly used in the management of Category/Stage I pressure ulcers. The slippery outer surface assists in reducing friction or shear to the underlying skin to protect it against further damage7.
What is the best treatment of pressure ulcers?
Clean open sores with water or a saltwater (saline) solution each time the dressing is changed. Putting on a bandage. A bandage speeds healing by keeping the wound moist. It also creates a barrier against infection and keeps skin around it dry.
How can Stage 1 pressure ulcers be prevented?
Avoid massaging bony prominences. Provide adequate intake of protein and calories. Maintain current levels of activity, mobility and range of motion. Use positioning devices to prevent prolonged pressure bony prominences.
What does a Stage 1 pressure sore look like?
STAGE 1. Signs: Skin is not broken but is red or discolored or may show changes in hardness or temperature compared to surrounding areas. When you press on it, it stays red and does not lighten or turn white (blanch).
What antibiotics treat bed sores?
Amoxicillin-potassium clavulanate is a naturally occurring beta-lactam structurally similar to the penicillin nucleus. This antibiotic group of beta-lactam/beta-lactamase combination has demonstrated a broad-spectrum activity; therefore, it is frequently used for the treatment of infected pressure ulcers.
What is the initial treatment for Stage 1 pressure ulcer?
If you believe that you have a stage 1 pressure ulcer, you should remove all pressure from the area. Keep the area as dry and clean as possible to prevent bacterial infections. To speed up the healing process, you should eat adequate calories and have a diet high in minerals, proteins, and vitamins.
How long does it take for a Stage 1 pressure ulcer to heal?
These are all good for your skin. Also, drink plenty of water. Recovery time: A Stage 1 pressure sore may go away in as little as 2 or 3 days.
What is a Category 1 pressure ulcer?
Classification of Pressure Ulcers. Page 1. Category I: Non-blanchable Erythema. Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its colour may differ from the surrounding area.
How to speed up the healing process of a pressure ulcer?
To speed up the healing process, you should eat adequate calories and have a diet high in minerals, proteins, and vitamins. Zinc, iron, vitamin A, and vitamin C will play the biggest role in the healing process. Drink water frequently to remain hydrated. Inspect the stage 1 pressure ulcer at least twice a day.
How long does it take for a pressure ulcer to go away?
Usually, you can reverse a pressure ulcer in this stage in about two to three days as long as pressure is removed. If the pressure ulcer hasn’t gone away after three days, you should call your physician.
How do you know if you have a stage 1 pressure ulcer?
Here is some information about the symptoms and signs that may indicate that you have a stage 1 pressure ulcer. Discolored, reddened, or darkened skin is one of the first signs of a pressure ulcer. For individuals with darker skin, purple, bluish, and shiny areas are one of the first signs. The area may feel warm or hard.
How to tell if you have a pressure ulcer?
How Can You Tell If You Have a Pressure Sore? 1 Discolored, reddened, or darkened skin is one of the first signs of a pressure ulcer. For individuals with darker skin, purple, bluish, and shiny areas are one of the first signs. The area may feel warm or hard. 2 If you remove pressure from the afflicted area for 30 minutes and the skin does not go back to normal, a pressure ulcer has begun to form. 3 Press on the afflicted area with your finger to do the blanching test. Once the area goes white, you should remove the pressure. If the area remains white, this means blood flow has been impaired. The blanching test may not be as effective when it comes to dark skin.
How to treat pressure ulcers?
Treating pressure ulcers involves reducing pressure on the affected skin, caring for wounds, controlling pain, preventing infection and maintaining good nutrition.
What can a social worker do for a child with pressure ulcers?
Parents or caregivers of children with pressure ulcers can talk with a child life specialist for help in coping with stressful health situations.
What to do if a bedsore doesn't heal?
One method of surgical repair is to use a pad of your muscle, skin or other tissue to cover the wound and cushion the affected bone (flap surgery).
What is the best medication for a wound?
Drugs to control pain. Nonsteroidal anti-inflammatory drugs — such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) — might reduce pain. These can be very helpful before or after repositioning and wound care. Topical pain medications also can be helpful during wound care.
How to heal a wound?
To heal properly, wounds need to be free of damaged, dead or infected tissue. The doctor or nurse may remove damaged tissue (debride) by gently flushing the wound with water or cutting out damaged tissue.
What is the best way to heal a wound?
A bandage speeds healing by keeping the wound moist. It also creates a barrier against infection and keeps skin around it dry. Bandage choices include films, gauzes, gels, foams and treated coverings. You might need a combination of dressings.
How to clean a wound that is not broken?
Generally, cleaning and dressing a wound includes the following: Cleaning. If the affected skin isn't broken, wash it with a gentle cleanser and pat dry. Clean open sores with water or a saltwater (saline) solution each time the dressing is changed. Putting on a bandage.
How to prevent pressure ulcers?
An individual can prevent the development of pressure ulcers by frequently repositioning and avoiding stress on the skin. Apart from this, taking good care of skin, good nutrition, and fluid intake, avoiding smoking & stress and daily exercises can help a lot.
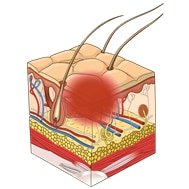
What is a pressure ulcer?
Also known as Bedsore , Pressure Sore , or Decubitus Ulcer , a Pressure Ulcer is an area of damaged skin & underlying tissue caused by prolonged pressure on the skin that cuts-off blood flow to the parts of the body and results in injuries to the skin and tissues. A Pressure Ulcer is an open wound on the skin that often occurs on ...
How does negative pressure wound therapy work?
Negative pressure wound therapy. The healing process depends on the stage of your ulcer. The sooner it is diagnosed, the sooner treatment can be started and recovery can also be quick. Wound Care Surgeons may suggest you make some small lifestyle changes in your diet while later stages require more aggressive treatment.
Why is it important to have proper nutrition for ulcers?
Proper nutrition is crucial to ensure effective and proper wound healing.
What happens if you have dementia and you can't understand pressure ulcers?
They may also be unable to sense discomfort as a necessary signal to change position.
Can pressure ulcers be treated?
In other words, people who are not in a condition to make small movements are at risk of Pressure Ulcers . The condition can be treated but chronic deep ulcers are difficult to treat. It depend s on several factors such as under lying medical conditions and the stage of the ulcer.
Can pressure ulcers happen to anyone?
In simple language, Pressure Ulcers can happen to anyone but the people who spend a long time in one position or those confined to a bed or sit in a chair or wheelchair for long periods due to several reasons such as paralysis , illness , old age , or frailty , etc are usually prone to this .
What happens if you have a pressure ulcer?
Infection is the most common major complication of pressure ulcers/injuries. If the ulcer progresses far enough, it can lead to osteomyelitis (infection of the underlying bone) or sinus tracts, which themselves can be either superficial or connect to deeper structures.
What are the factors to consider when treating a stage 1 pressure injury?
The key factors to consider in a treating a stage 1 pressure injury are identifying the cause of the wound and determining how best to prevent it from worsening, including an evaluation of the nutritional status of the patient. The presence of a stage 1 pressure injury should be a signal to take preventive action.
What is pressure injury?
Pressure injuries are localized areas of tissue necrosis that typically develop when soft tissue is compressed between a bony prominence and an external surface for a long period of time. Stage 1 pressure injuries are characterized by superficial reddening of the skin (or red, blue or purple hues in darkly pigmented skin) ...
How to prevent bony prominences?
Provide adequate intake of protein and calories. Maintain current levels of activity, mobility and range of motion. Use positioning devices to prevent prolonged pressure bony prominences.
What is the most common grading system for pressure ulcers?
Healthcare professionals use several grading systems to describe the severity of pressure ulcers; most common is the EPUAP grading system. Pressure sores are categorised into four stages [Table 2] corresponding to the depth of damage.[22,23,24] It must however be emphasised that when an eschar is present, accurate staging is not possible.
What is the most accurate description of a pressure ulcer?
Pressure ulcers are a type of injury that breaks down the skin and underlying tissue when an area of skin is placed under constant pressure for certain period causing tissue ischaemia, cessation of nutrition and oxygen supply to the tissues and eventually tissue necrosis. Constant pressure resulting in ‘distortion or deformation damage’ is probably the most accurate description of a pressure ulcer.[1] There is a localised, acute ischaemic damage to any tissue caused by the application of external force (either shear, compression or a combination of the two).
What does a grade 2 pressure ulcer look like?
Grade 2. In Grade 2 pressure ulcers, some of the outer surface of the skin (the epidermis) or the deeper layer of skin (the dermis) is damaged, leading to skin loss [Figure 1b]. The ulcer looks like an open wound or a blister.
Why do ulcers have oxygen?
Oxygen is required for all stages of wound healing thus any condition that is associated with a low tissue oxygen tension is a major cause of pressure ulcers. These include: Heart failure, atrial fibrillation, myocardial infarction, and chronic obstructive pulmonary disease.
Can friction cause pressure ulcers?
Friction, along with pressure and shear, is also frequently cited as a cause of pressure ulcers.[14] . Friction can cause pressure ulcers both indirectly and directly. In the indirect sense, friction is necessary to generate the shearing forces.
Can pressure sores develop in the soles of feet?
The height of the available tissue cover over the bony prominence is not the only determining factor for developing pressure sores. Although the soles of the feet have a thin covering of soft tissue, they have a vasculature that is particularly well-adapted to withstand considerable distorting forces. On the sacrum and ischial tuberosity on the other hand, although there is a relatively thick covering of soft tissue and a wide supporting surface, the blood vessels are not adapted for weight-bearing, which means that even with fairly light compression, pressure ischaemia can develop rapidly. Hence, soles of feet do not develop pressure sores even after prolong weight bearing in ambulatory patients unless there are underlying causes making them insensate and more prone to pressure damage.
What age group is most likely to have pressure ulcers?
Age is also a factor that the majority (approximately two-third) of pressure ulcers occur in old age people (60-80 years of age).[7] .
What is pressure ulcer?
A pressure ulcer is a localized injury to the skin or underlying tissue, usually over a bony prominence, as a result of unrelieved pressure. Predisposing factors are classified as intrinsic (e.g., limited mobility, poor nutrition, comorbidities, aging skin) or extrinsic (e.g., pressure, friction, shear, moisture).
What is the assessment of pressure ulcers?
Assessment of an established pressure ulcer involves a complete medical evaluation of the patient. A comprehensive history includes the onset and duration of ulcers, previous wound care, risk factors, and a list of health problems and medications. Other factors such as psychological health, behavioral and cognitive status, social and financial resources, and access to caregivers are critical in the initial assessment and may influence treatment plans. The presence of a pressure ulcer may indicate that the patient does not have access to adequate services or support. The patient may need more intensive support services, or care-givers may need more training, respite, or assistance with lifting and turning the patient. Patients with communication or sensory disorders are particularly vulnerable to pressure ulcers because they may not feel discomfort or may express discomfort in atypical ways.
What should a physician note about ulcers?
The physician should note the number, location, and size (length, width, and depth) of ulcers and assess for the presence of exudate, odor, sinus tracts, necrosis or eschar formation, tunneling, undermining, infection, healing (granulation and epithelialization), and wound margins. Most importantly, the physician should determine the stage of each ulcer ( Figures 1 through 4).
What are pressure reducing devices?
Pressure-reducing devices can reduce pressure or relieve pressure (i.e., lower tissue pressure to less than the capillary closing pressure of 32 mm Hg) and are classified as static (stationary) or dynamic. 9 Static devices include foam, water, gel, and air mattresses or mattress overlays. Dynamic devices, such as alternating pressure devices and low–air-loss and air-fluidized surfaces, use a power source to redistribute localized pressure. Dynamic devices are generally noisy and more expensive than static devices. Pressure-reducing surfaces lower ulcer incidence by 60 percent compared with standard hospital mattresses, although there is no clear difference among pressure-reducing devices. 10, 11 The benefit of dynamic versus static surfaces is unclear. Dynamic surfaces should be considered if a patient cannot reposition him- or herself independently or if the patient has a poorly healing ulcer. 7 If there is less than 1 inch of material between the bed and pressure ulcer when feeling beneath the static surface, the device may not be effective and an alternative should be considered. 7 Other pressure-reducing devices include chair cushions and pillows, foam wedges, and materials that are placed between the knees or used to relieve heel pressure. Ring cushions can cause pressure points and should not be used.
What is the most common site for pressure ulcers?
The most common sites for pressure ulcers are the sacrum, heels, ischial tuberosities, greater trochanters, and lateral malleoli.
Does a pressure reducing mattress help with ulcers?
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers. There is no evidence to support the routine use of nutritional supplementation (vitamin C, zinc) and a high-protein diet to promote the healing of pressure ulcers.
What percentage of pressure ulcers occur in older people?
Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years, 1 younger patients with neurologic impairment or severe illness are also susceptible.
What is stage IV pressure ulcer?
Stage IV: The pressure ulcer has become so deep that there is damage to the muscle and bone, and sometimes to tendons and joints. There are two other types of pressure sores that don't fit into the stages. Sores covered in dead skin that is yellow, tan, green, or brown.
How to clean a stage 2 pressure sore?
Ask your provider what type of moisturizer to use. Stage II pressure sores should be cleaned with a salt water (saline) rinse to remove loose, dead tissue.
What is stage 2 of a sore?
Stage II: The skin blisters or forms an open sore. The area around the sore may be red and irritated.
How to check for pressure sores?
Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can't see. If the pressure sore changes or a new one forms, tell your provider. Take care of your health.
How to get rid of pressure sores on skin?
Avoid further injury or friction. Powder your sheets lightly so your skin doesn't rub on them in bed. Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore. Care for healthy skin by keeping it clean and moisturized. Check your skin for pressure sores every day.
How to treat a pressure sore at home?
Here's how to care for a pressure sore at home. Relieve the pressure on the area. Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area.
Where do pressure sores form?
Pressure sores tend to form where skin covers bony areas, such as your:
What is the cornerstone of pressure ulcer prevention?
The cornerstone of pressure ulcer prevention is identifying and minimizing risk factors with the use of a validated risk assessment tool. 10
What is pressure ulcer?
A pressure ulcer is the result of a degenerative change caused by biological tissue (skin and underlying tissue) being exposed to pressure and shear forces. The increased pressure prevents the blood from circulating properly, and causes cell death, tissue necrosis and the development of pressure ulcers. The effect of pressure and shear forces on tissue and blood supply Heel, Unstageable
What is the best dressing for pressure ulcers?
An antimicrobial moist wound healing dressing, e.g.a silver foam (Biatain® Ag), or a silver alginate dressing (SeaSorb®Soft Ag) in combination with an adhesive secondary dressing(Biatain Silicone) may help prevent or resolve wound infection.
What is wound dressing?
Wound dressings are a central component of pressure ulcer care.Dressing selection should be based on the type of tissue in thewound bed, the depth of the wound, the amount of wound exudateand the condition of the periwound skin. Suitable wound dressingsfor pressure ulcers are moist wound healing dressings with goodabsorption and exudate management properties.
What is the depth of a stage IV pressure ulcer?
Further description: The depth of a Category/ Stage IV pressure ulcer varie s by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Category/ Stage IV ulcers can extend into muscle and/or supporting structures (for example, fascia, tendon or joint capsule) making osteomyelitis or osteitis likely to occur. Exposed bone/muscle is visible or directly palpable.
What is the prevalence of pressure ulcers?
Prevalence studies, among patients in acute care hospitals, indicated a pressure ulcer prevalence ranging from 10.1% to 17% .3Recently, 5947 patients were surveyed in 25 hospitals in five European countries. The pressure ulcer prevalence (Stage 1–4) was 18.1%. If Stage 1 pressure ulcers were excluded, the prevalence was 10.5%. The sacrum and heels were the most affected sites. Only 9.7% of the patients in need of prevention received fully adequate preventative care.3
Can an alginate filler be used on a deep pressure ulcer?
Infected deep pressure ulcers or deep wounds at-risk of infection can be filled with antimicrobial dressing materials, such as an alginate filler, and covered with an adhesive dressing. If the infection spreadsbeyond the wound, antibiotics should be used at the discretion of aphysician.
What is the purpose of the pressure ulcer study?
To assess the effects of dressings and topical agents for healing pressure ulcers in any care setting. We aimed to examine this evidence base as a whole, determining probabilities that each treatment is the best, with full assessment of uncertainty and evidence quality.
What is pressure ulcer dressing?
Background. Pressure ulcers, also known as bedsores, decubitus ulcers and pressure injuries, are localised areas of injury to the skin or the underlying tissue, or both. Dressings are widely used to treat pressure ulcers and promote healing, and there are many options to choose from including alginate, hydrocolloid and protease‐modulating dressings.
What is topical agent?
Topical agents are defined as hydrogels. ointments and creams that are placed in contact with the wound and left in situ; they may be covered with a secondary dressing.The following types of topical agents are considered as interventions in this review:
What is the best dressing for wounds?
Honey‐impregnated dressings contain medical‐grade honey that is purported to have antimicrobial and anti‐inflammatory properties and can be used for acute or chronic wounds. Examples include: Medihoney (Medihoney) and Activon Tulle (Advancis).
How much did pressure ulcers cost in 2006?
Figures from the USA suggest that for half a million hospital stays in 2006, 'pressure ulcer' was noted as a diagnosis; for adults, the total hospital cost for these stays was USD 11 billion ( Russo 2008 ).
How long does it take for pressure ulcers to heal?
Pressure ulcers are normally expected to show signs of healing within two weeks, but this may not occur and there can be deterioration ( EPUAP‐NPUAP‐PPPIA 2014 ).
What is the NMA for pressure ulcers?
A network meta‐analysis (NMA) of data from 39 studies (evaluating 21 dressings and topical agents for pressure ulcers) is sparse and the evidence is of low or very low certainty (due mainly to risk of bias and imprecision). Consequently we are unable to determine which dressings or topical agents are the most likely to heal pressure ulcers, and it is generally unclear whether the treatments examined are more effective than saline gauze.
Symptoms of Stage 1 Pressure Injuries
Risk Factors
- Treating pressure ulcers involves reducing pressure on the affected skin, caring for wounds, controlling pain, preventing infection and maintaining good nutrition.
Complications
Treatment of Stage 1 Pressure Injuries
References
- In addition to the aforementioned non-blanchable erythema, stage 1 pressure injuries may also differ in temperature (warmer or cooler), consistency (firmer or softer) or may be more tenderthan adjacent tissue.