Procedures
What is the definitive therapy for cardiac tamponade? Removal of pericardial fluid is the definitive therapy for tamponade and can be done using the following three methods: Emergency subxiphoid percutaneous drainage Pericardiocentesis (with or without echocardiographic guidance)
Self-care
- Chest X-rays
- Electrocardiogram (ECG or EKG) to look for changes in your heart rhythm
- Echocardiogram (echo) to check for fluid or pericardial effusion
- Cardiac MRI to check for pericardial inflammation
- CT scan to check for abnormalities around the heart
- Cardiac catheterization to determine if the heart is constricted
What is the definitive therapy for cardiac tamponade?
What are the three symptoms of cardiac tamponade?
- Chest pain or discomfort.
- Shortness of breath.
- Fast breathing.
- Increased heart rate.
- Enlargement of the veins of the neck.
- Fainting.
- Swelling in the arms and legs.
- Pain in the right upper abdomen.
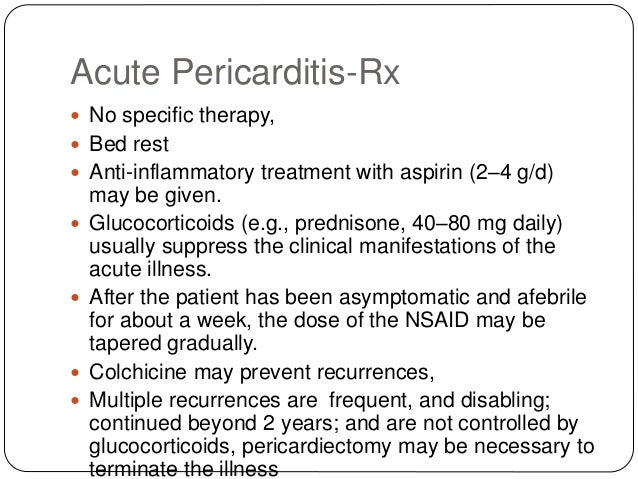
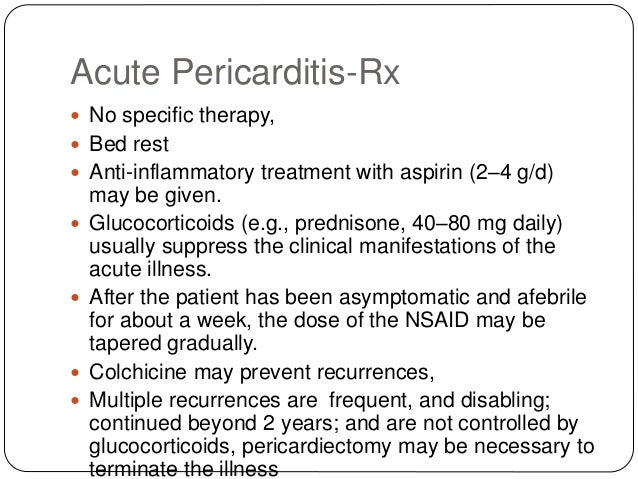
What is best treatment for pericarditis?
The patients were masked for the treatment but not the physicians ... gastrointestinal tract, liver hilum, pericardium, diaphragm, and major vessels (larger than 3 mm) 31. Three radiologists (AR, AZ and JS) with 5–10 years of experience in ...
What are the three signs of cardiac tamponade?
Is there a cure for pericarditis?
What is the definitive treatment for pericardial tamponade?
Removal of pericardial fluid is the definitive therapy for tamponade and can be done using the following three methods: Emergency subxiphoid percutaneous drainage. Pericardiocentesis (with or without echocardiographic guidance) Percutaneous balloon pericardiotomy.
What is the priority intervention for a client with cardiac tamponade?
Penetrating traumatic pericardial tamponade require prompt surgical intervention: pericardial window if the patient has vital signs, or emergency department thoracotomy if the patient has no pulse.
What are the current treatment options available for pericardial effusion?
Surgeries or other procedures to treat pericarditis include: Pericardiocentesis. In this procedure, a sterile needle or a small tube (catheter) is used to remove and drain the excess fluid from the pericardial cavity. Removal of the pericardium (pericardiectomy).
What is cardiac tamponade what are known causes and treatments?
Cardiac tamponade happens when the space around your heart fills with blood or other fluid, putting pressure on your heart. Because of the pressure, your heart can't beat correctly, causing a drop in blood pressure. Trauma and certain diseases can cause cardiac tamponade. If not treated, it is always fatal.
What is the nursing management of cardiac tamponade?
Administering intravenous fluids such as 0.9% sodium chloride solution or lactated Ringer's solution to increase filling pressures if the patient has acute tamponade. Preparing to administer inotropes, as prescribed, to increase cardiac output, improve myocardial contractility, and optimize preload.
Do you give fluids for cardiac tamponade?
Treatment for Cardiac Tamponade Inotropic drugs, such as dobutamine: To improve heart function and lower blood pressure. Volume expansion with IV fluids: To help maintain the heart's volume. Oxygen: To reduce the heart's workload. Pericardiocentesis: To drain the fluid from the pericardium using a needle.
Can fluid around the heart be treated with medication?
The treatment for fluid around the heart depends on what is causing the buildup, but it may involve medications and various procedures. These include: ibuprofen, aspirin, and other nonsteroidal anti-inflammatory drugs, which can help control inflammation. diuretics, which can treat fluid buildup due to heart failure.
Does fluid around the heart go away on its own?
How is it treated? If there is only a small amount of extra fluid in your pericardium, you may not need treatment. The extra fluid may go away on its own. Treatment depends on the cause of the extra fluid, the amount of fluid, and your symptoms.
Can a pericardial effusion resolve on its own?
Treatment of pericardial effusion depends on the cause and severity of the condition. In some cases where the effusion is small and uncomplicated, it may resolve on its own, with anti-inflammatory medication recommended to help the healing process.
How do paramedics treat cardiac tamponade?
Treatment is directed at decreasing intrapericardial pressure by withdrawing fluid from the pericardial sac. Typically, a needle is inserted into the pericardial space and enough fluid withdrawn to normalize vital signs. This process, called a pericardiocentesis, is dangerous.
What is the prognosis of cardiac tamponade?
Cardiac tamponade is a medical emergency. The prognosis depends on prompt recognition and management of the condition and the underlying cause of the tamponade. Untreated, cardiac tamponade is rapidly and universally fatal.
What are the three signs of cardiac tamponade?
The classic signs of cardiac tamponade are known as Beck's triad, which includes low blood pressure, distension of the jugular veins, and muffled heart sounds.
What is pericardial tamponade?
Pericardial tamponade, also known as cardiac tamponade, is a medical condition caused by the compression of the heart due to a build-up of fluid, b...
What causes pericardial tamponade?
Pericardial tamponade can develop suddenly as a result of chest trauma like a stab wound or blunt trauma, rupture of the aorta, rupture of the vent...
What is the difference between pericardial effusion and cardiac tamponade?
Pericardial effusion happens when pericardial fluid builds up slowly over time, which allows the pericardium to stretch out to accommodate bigger a...
What are the three signs of cardiac tamponade?
The classic signs of cardiac tamponade are known as Beck’s triad, which includes low blood pressure, distension of the jugular veins, and muffled h...
How do you diagnose pericardial tamponade?
Diagnosis of a pericardial tamponade is suspected in individuals with low blood pressure and jugular vein distention in the presence of a pericardi...
How do you treat pericardial tamponade?
People with cardiac tamponade need to receive treatment urgently after the diagnosis is made. Treatment for cardiac tamponade consists of removing...
What are the most important facts to know about pericardial tamponade?
A pericardial tamponade is a life-threatening compression of the heart due to the build-up of fluid, blood, or air in the pericardial sac. It can o...
What is a pericardial tamponade?
What are the most important facts to know about pericardial tamponade? A pericardial tamponade is a life-threatening compression of the heart due to the build-up of fluid, blood, or air in the pericardial sac. It can occur as a result of trauma, inflammation, infection, or rupture of the heart or the aorta.
Why does a tamponade occur?
In rare cases, a cardiac tamponade can occur due to the presence of air in the pericardial sac, known as pneumopericardium.
What are the signs of tamponade?
The classic signs of cardiac tamponade are known as Beck’s triad, which includes low blood pressure, distension of the jugular veins, and muffled heart sounds. The low blood pressure is a consequence of the decreased volume of blood being pumped by the heart and is typically accompanied by other signs, such as increased heart rate, ...
What is the pericardium filled with?
Normally, the pericardium is filled with a small amount of fluid that prevents the two layers of the pericardium from rubbing together as the heart beats. Pericardial tamponade occurs when there’s an increased amount of fluid, blood, or air inside the pericardial sac.
What happens when fluid accumulates in the pericardium?
On the other hand, when there’s a sudden fluid accumulation, the pericardium has no time to adjust, so even small amounts can cause a dramatic increase of pressure inside the pericardial sac, resulting in acute pericardial tamponade.
Is pericardial tamponade a medical emergency?
Pericardial tamponade can rapidly progress to circulatory shock and even cardiac arrest. Thus, it is considered a medical emergency that requires prompt treatment.
What is the surgical option for a tamponade?
Surgical options include creating a pericardial window or removing the pericardium. Emergency department resuscitative thoracotomy and the opening of the pericardial sac is a therapy that can be used in traumatic arrests with suspected or confirmed cardiac tamponade.
What is a cardiac tamponade?
Cardiac tamponade is a medical emergency that takes place when abnormal amounts of fluid accumulate in the pericardial sac compressing the heart and leading to a decrease in cardiac output and shock. This activity describes the evaluation and management of cardiac tamponade and reviews the role of the interprofessional team in improving care ...
What causes tamponade in the heart?
Cardiac tamponade is caused by the buildup of pericardial fluid (exudate, transudate, or blood) that can accumulate for several reasons. Hemorrhage, such as from a penetrating wound to the heart or ventricular wall rupture after an MI, can lead to a rapid increase in pericardial volume.
What is a tamponade?
Cardiac tamponade is a medical or traumatic emergency that happens when enough fluid accumulates in the pericardial sac compressing the heart and leading to a decrease in cardiac output and shock.
What is the underlying pathology behind cardiac tamponade?
The underlying pathology behind cardiac tamponade is a decreased in diastolic filling, which leads to a decreased cardiac output. One of the first compensatory signs is tachycardia to overcome the reduced output.
How long does it take for a tamponade to die?
The key is the timing of intervention; the longer the delay, the worse the outcomes. Patients with tamponade caused by malignant disease have death rates exceeding 75% within 12 months.
How long does it take to die from pericardial effusion?
In all cases, the underlying cause must be treated. When the cause of the pericardial effusion is a malignancy, it carries an 80% mortality within 12 months, whereas patients with a non-malignant cause have a mortality rate of less than 15%. [2][15](Level V) Continuing Education / Review Questions.
What to do if you have tamponade?
If anti-inflammatory treatments don't correct the problem or you have or are likely to have tamponade, your cardiologist may recommend one of the following procedures to drain fluids or prevent fluids from accumulating again. Drain the fluid .
What to do if you have pericardial effusion?
If your pericardial effusion is discovered as a result of a heart attack or other emergency, you won't have time to prepare for your appointment. Otherwise, you'll likely start by seeing your primary care provider. Or you might be referred immediately to a cardiologist.
What test is done to determine if you have pericardial effusion?
If you have signs or symptoms of pericardial effusion, a series of blood and imaging tests will be done to confirm the diagnosis, identify possible causes and determine treatment.
What is the procedure called when a doctor uses a small tube to drain fluid?
Your doctor can enter the pericardial space with a needle and then use a small tube (catheter) to drain fluid — a procedure called pericardiocentesis. The doctor uses echocardiography or a type of X-ray imaging called fluoroscopy to guide the catheter to the right position.
Where is the transducer placed on a heart?
A tiny transducer on a tube is put down the part of your digestive tract that runs from your throat to your stomach (esophagus). Because the esophagus lies close to the heart, having the transducer placed there often provides a more detailed image of the heart.
What is the purpose of echocardiogram?
Echocardiogram. An echocardiogram uses sound waves to create real-time images of your heart. This test allows your doctor to see how much fluid has collected in the space between the two layers of the pericardium. An echocardiogram can also show how well your heart is pumping blood and help diagnosis tamponade or a collapse in one ...
What factors influence the management strategy of tamponade?
Factors that influence the management strategy include evaluating the cause, providing haemodynamic support, and choosing the technique. Fluid resuscitation to maintain venous pressure and circulation may be beneficial up to a point, after which, tamponade may be aggravated.
Is tamponade a definitive therapy?
Cardiac tamponade is an emergency, and definitive therapy is fluid removal by pericardiocentesis. In certain conditions, fluid removal is still the optimal choice, but a conservative approach using haemodialysis may be employed.
Is fluid removal surgery or percutaneous?
While inotropes have theoretical benefit, studies involving humans are few. Fluid removal strategies are broadly grouped into percutaneous and surgical methods. In most cases, the percutaneous approach is favoured. However, surgery is typically the first choice in blunt trauma or in proximal aortic dissection.
