
Treatment of an MI is time-critical. Aspirin is an appropriate immediate treatment for a suspected MI. Nitroglycerin
Nitroglycerin
Nitroglycerin extended-release capsules are used to prevent chest pain in people with a certain heart condition.
Full Answer
What medicine is used in an emergency for myocardial infarction?
Some questions to ask your doctor about heart attack prevention include:
- What tests do I need to determine my current heart health?
- What foods should I eat or avoid?
- What's an appropriate level of physical activity?
- How often should I be screened for heart disease?
- I have other health conditions. How can I best manage these conditions together?
- Are there brochures or other printed material that I can have? ...
Why are STEMI heart attacks so deadly?
Why a ‘Widowmaker’ Heart Attack Is So Dangerous
- Different kinds of heart attacks. There are three main arteries in the heart — one on the right side and two on the left side. ...
- Action plan: Call 911. Every minute matters when someone’s having a heart attack. ...
- Keeping your risk in check. When it comes to any kind of heart attack, “the best thing is prevention,” Dr. ...
How does nitroglycerine help with a myocardial infarction?
Proper Use
- Dosing. The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label.
- Missed Dose. If you miss a dose of this medicine, take it as soon as possible. ...
- Storage. Keep out of the reach of children. Do not keep outdated medicine or medicine no longer needed. ...
What tests confirm a diagnosis of myocardial infarction?
You may also undergo:
- Chest X-ray. An X-ray image of your chest allows your doctor to check the size of your heart and its blood vessels and to look for fluid in your lungs.
- Echocardiogram. ...
- Coronary catheterization (angiogram). ...
- Exercise stress test. ...
- Cardiac computerized tomography (CT) or magnetic resonance imaging (MRI). ...
What causes a myocardial infarction?
The most frequent cause of myocardial infarction (MI) is rupture of an atherosclerotic plaque within a coronary artery with subsequent arterial spasm and thrombus formation. Other causes include the following: Coronary artery vasospasm. Ventricular hypertrophy.
What happens to the heart after an infarction?
Inflammation of the lining of the heart occurs after infarction. This is painful and is reduced by the drugs.
Why is support important in hospitals?
It is important in these patients because support plays a important role in these patients who have less chances of survival during the administration to hospital .
What is the name of the artery that causes the heart to die?
This is most commonly due to occlusion (blockage) of a coronary artery following the rupture of a vulnerable atherosclerotic plaque, which is an unstable collection of lipids (fatty acids) and white blood cells in the wall of an artery. The resulting ischemia (restriction in blood supply) and oxygen shortage, if left untreated for a sufficient period of time, can cause damage or death of heart muscle tissue.
What is the cause of acute myocardial inferior infarction?
An acute myocardial inferior infarction has been attributed to the formation of acetaldehyde in a 22-year-old chronic alcoholic man who took oral disulfiram and alcohol together [54A ]. Coronary angiography showed normal coronary arteries.
What causes inferior MI?
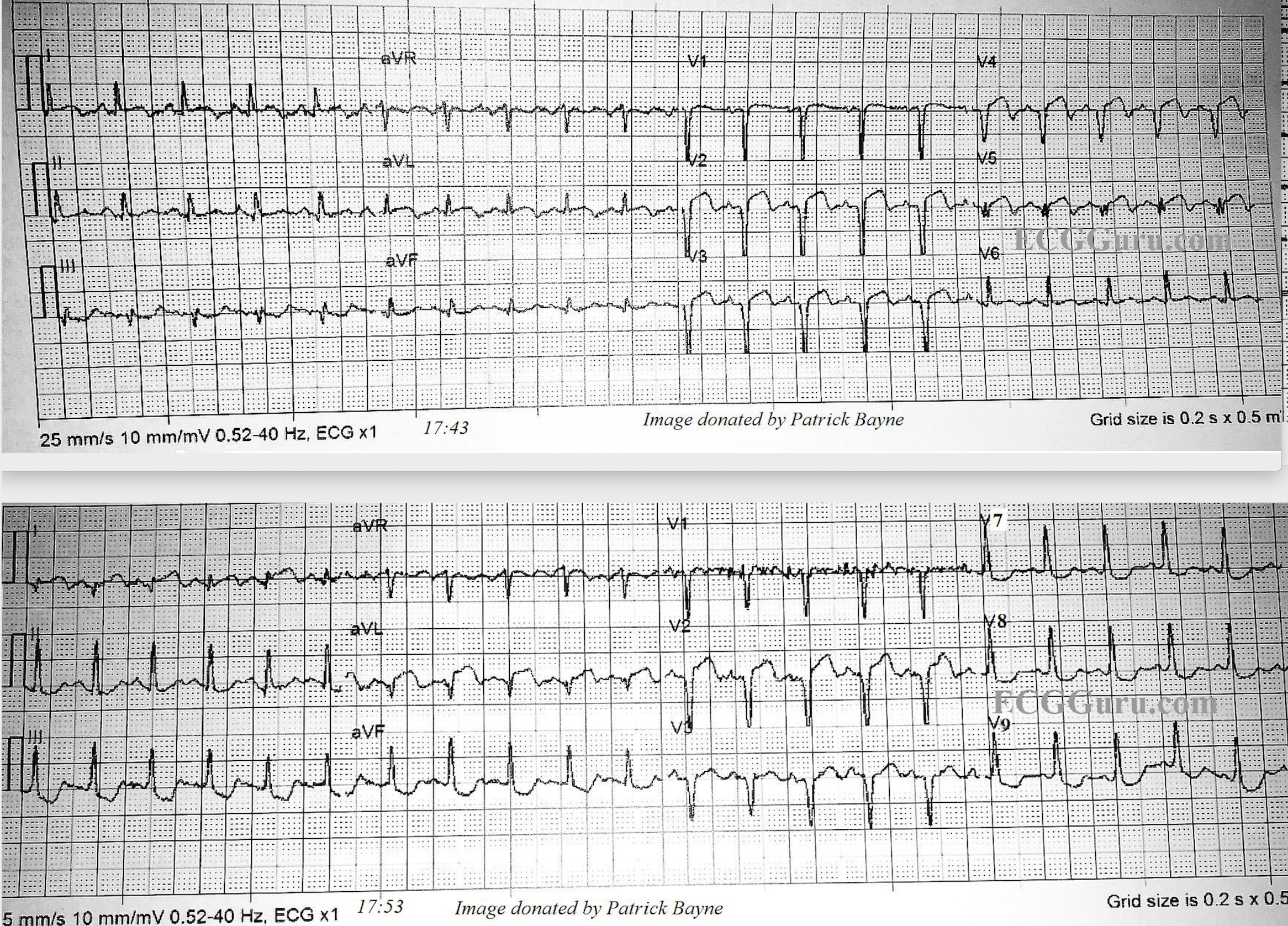
Inferior MI is caused by the occlusion of the dominant left circumflex artery in about 18% of cases. 40 Myocardial infarction caused by the dominant right coronary artery and the dominant left circumflex artery tends to produce similar Q wave changes (Figures 7-8, 7-9, and 7-16 to 7-21 ), but the pattern of ST segment elevation may be helpful for the differential diagnosis. This is shown in Figure 17-22, reproduced from the study of Wellens et al. 23 Although both vessels perfuse the inferior wall, the RCA territory covers the medial part including the inferior septum, whereas the circumflex territory covers the left posterobasal and lateral area. Thus in the case of RCA occlusion, the ST vector is directed inferiorly and rightward, whereas in the case of left circumflex occlusion, the ST vector points inferiorly and leftward. Accordingly, in RCA occlusion, the ST elevation is greater in lead III than in lead II with ST depression in lead I, whereas in the case of circumflex occlusion, ST segment in lead I is either elevated or isoelectric. In the experience of these investigators, 23 ST depression in lead I was predictive of RCA occlusion in 86 percent of cases and an isoelectric or elevated ST segment in lead I was predictive of circumflex occlusion in 77 percent of cases.
What is the mitral isthmus?
The mitral isthmus (between the mitral annulus and inferior infarct scar) contains a critical region of slow conduction in some patients with VT following inferior MI , providing a vulnerable and anatomically localized target for catheter ablation. This critical zone of slow conduction is activated parallel to the mitral annulus in either direction, resulting in two distinct QRS configurations not seen in VTs arising from other sites: LBBB pattern (rS in lead V 1, R in lead V 6) with left superior axis, and RBBB pattern (R in lead V 1, QS in lead V 6) and right superior axis. 3,32
What is a large inferoposterior infarction?
A large inferoposterior infarction combines abnormalities of the posterolateral and inferior MIs.
How to tell if you have transmural ischemia?
Ordinarily, the earliest sign of transmural ischemia is ST segment elevations (with reciprocal ST depressions). The ST elevations (current of injury pattern) usually persist for hours to days. During this same period, Q waves often begin to appear in the leads that show ST elevations. Once these changes have occurred, the ST segments start to return to the isoelectric baseline and the T waves become inverted during the evolving phase.
Does RVMI cause pulmonary embolism?
As in LVMI, RVMI may predispose to thrombus formation in the infarcted ventricle with possible pulmonary embolism. In the presence of a PFO, paradoxical embolization may lead to systemic emboli. Thrombus has been identified in the RV of patients with RVMI (3 of 33; 9%) and in patients without RV infarction with posterior wall MI (4 of 106; 4%). 96
How long do Q waves last after an infarct?
In the weeks or months after an infarct, what should you expect to happen to the Q waves and the ST-T changes just described? The answer is that you cannot make any certain predictions. In most cases, the abnormal Q waves persist for months and even years after the acute infarction. Occasionally, however, the abnormal Q waves diminish in size and even disappear entirely. In some cases, abnormal T wave inversions persist indefinitely. In others, improvement occurs, but minor nonspecific ST-T abnormalities such as slight T wave flattening may persist (see Figs. 8-4 and 8-5 ).
What is the first goal for healthcare professionals in management of acute myocardial infarction (MI)?
The first goal for healthcare professionals in management of acute myocardial infarction (MI) is to diagnose the condition in a very rapid manner.
How does MI reduce morbidity?
Morbidity and mortality from MI are significantly reduced if patients and bystanders recognize symptoms early, activate the emergency medical service (EMS) system, and thereby shorten the time to definitive treatment . Trained prehospital personnel can provide life-saving interventions if the patient develops cardiac arrest. The key to improved survival is the availability of early defibrillation. Approximately 1 in every 300 patients with chest pain transported to the emergency department by private vehicle goes into cardiac arrest en route. [ 66] In the United States, several studies have confirmed that patients with STEMI usually do not call 911, and only about 40% of patients with a confirmed coronary event used EMS. [ 67]
How soon after STEMI can you perform PCI?
Early mechanical intervention (primary PCI) or pharmacologic reperfusion should be performed as soon as possible for patients with clinical presentation of STEMI within 12 hours of symptom onset and who have persistent ST-segment elevation or new or presumed new left bundle branch block (LBBB). In addition, it is reasonable to consider an early reperfusion strategy for patients presenting after more than 12 hours, provided there is clinical and/or ECG evidence of ongoing ischemia, with primary PCI being the preferred method in this population.
How long does it take to get an ECG for MI?
A 12-lead electrocardiogram (ECG) interpreted by an experienced physician should be completed within 10 minutes of arrival, in addition to establishing intravenous (IV) access.
Does prehospital ECG help with door to balloon time?
Prehospital integration of ECG interpretation has been shown to decrease "door-to-balloon time,” allow paramedics to bypass non–percutaneous coronary intervation (PCI)–capable hospitals in favor of PCI-capable facilities, and to expedite care by allowing an emergency department physician to activate the catheterization laboratory before the patient's arrival.
What is an acute myocardial infarction?
What is acute myocardial infarction? Acute myocardial infarction is the medical name for a heart attack . A heart attack is a life-threatening condition that occurs when blood flow to the heart muscle is abruptly cut off, causing tissue damage. This is usually the result of a blockage in one or more of the coronary arteries.
How to unblock a heart artery?
Heart attacks require immediate treatment, so most treatments begin in the emergency room. A minimally invasive procedure called angioplasty may be used to unblock the arteries that supply blood to the heart. During an angioplasty, your surgeon will insert a long, thin tube called a catheter through your artery to reach the blockage. They will then inflate a small balloon attached to the catheter in order to reopen the artery, allowing blood flow to resume. Your surgeon may also place a small, mesh tube called a stent at the site of the blockage. The stent can prevent the artery from closing again.
What causes a blockage in the arteries?
Bad cholesterol. Bad cholesterol, also called low-density lipoprotein (LDL), is one of the leading causes of a blockage in the arteries. Cholesterol is a colorless substance that’s found in the food you eat. Your body also makes it naturally.
How to lower your risk of heart disease?
One way to lower your risk is to eat a heart-healthy diet. This diet should largely consist of:
What to do if you think someone has a heart attack?
Call 911 right away if you think that you or someone you know may be having a heart attack.
How to lower cholesterol?
You may be able to lower your cholesterol by making changes to your diet or by taking certain medications called statins.
What inotropes are used for right ventricular failure?
Inotropes that can be used in right ventricular failure are dobutamine, milrinone, levosimendan (approved only in Europe), norepinephrine, and, possibly, low-dose vasopressin. Avoid dopamine and phenylephrine. [ 27] Previous. Next: Right Ventricular Dysfunction and Shock.
What is the role of beta blockers in right ventricular hemodynamics?
Beta-blocking agents and angiotensin-converting enzyme inhibitors improve right ventricular hemodynamics in patients with biventricular failure and have theoretical benefits in isolated right ventricular failure, but their role in the latter is poorly studied. [ 27]
How long after onset of right ventricular dysfunction can you expect improvement?
Scant data exist regarding improvement in patients who present later than 12 hours after onset, and these patients most likely would do well with a conservative management strategy, considering the often spontaneous resolution of right ventricular dysfunction. [ 42]
Is right ventricular infarction considered hypotension?
Right ventricular infarction should always be considered in any patient who has inferior wall myocardial infarction and associated hypotension, especially in the absence of rales. In patients with right ventricular dysfunction and shock, the focus is on ensuring adequate right-sided filling pressures. If cardiogenic shock persists ...
Can nitric oxide be used for right ventricular infarction?
The use of inhaled nitric oxide has been of interest to treat patients with right ventricular infarctions complicated by cardiogenic shock. The principle behind this treatment is that by specifically decreasing pulmonary vascular resistance without compromising systemic vascular resistance, the filling of the left ventricle can be improved with a resultant improvement of systemic cardiac output. Utilization of inhaled nitric oxide in this setting has been associated with rapid improvement of hemodynamics. [ 43]
Does PPCI lower mortality?
A study by Lupi-Herrera et al indicated that primary percutaneous coronary intervention (PPCI) leads to lower mortality rates than does thrombolytic therapy in patients with right ventricular infarction. Patients were divided into three groups: those without right ventricular failure, those with right ventricular failure, and those with cardiogenic shock. Of all of them, 148 patients underwent thrombolytic therapy and 351 patients were treated with PPCI. In-hospital mortality rates at 30 days were as follows [ 38] :
Can tricuspid regurgitation be repaired?
Severe tricuspid regurgitation in the setting of acute right ventricular infarction can be managed with either valve replacement or repair with angioplasty rings, because the incompetent valve may serve as a mechanical impediment to maintenance of adequate cardiac output. Finally, should a patient develop arterial hypoxemia secondary to right-to-left shunting at the atrial level, then an atrial septal defect–occluding device should be considered. However, if for any reason a delay occurs in placement of the occluding device, inhaled nitric oxide can decrease the right-to-left shunting and increase systemic oxygenation. [ 43]
