
- Alendronate (Binosto, Fosamax)
- Ibandronate (Boniva)
- Risedronate (Actonel, Atelvia)
- Zoledronic acid (Reclast, Zometa)
What is the most effective treatment for osteoporosis?
Bisphosphonates are usually the first choice for osteoporosis treatment. These include: Alendronate (Fosamax), a weekly pill. Risedronate (Actonel), a weekly or monthly pill.
What treatment is required for osteoporosis?
Treatments for established osteoporosis may include exercise, vitamin and mineral supplements, and medications. Exercise and supplementation are often suggested to help you prevent osteoporosis. Weight-bearing, resistance and balance exercises are all important.Apr 27, 2020
What is the life expectancy of a person with osteoporosis?
The average life expectancy of osteoporosis patients is in excess of 15 years in women younger than 75 years and in men younger than 60 years, highlighting the importance of developing tools for long-term management.
What is the fastest way to increase bone density?
10 Natural Ways to Build Healthy BonesEat Lots of Vegetables. ... Perform Strength Training and Weight-Bearing Exercises. ... Consume Enough Protein. ... Eat High-Calcium Foods Throughout the Day. ... Get Plenty of Vitamin D and Vitamin K. ... Avoid Very Low-Calorie Diets. ... Consider Taking a Collagen Supplement. ... Maintain a Stable, Healthy Weight.More items...•Jan 18, 2017
What is the newest treatment for osteoporosis?
Romosozumab (Evenity). This is the newest bone-building medication to treat osteoporosis. It is given as an injection every month at your doctor's office and is limited to one year of treatment.Aug 21, 2021
What is the safest drug to take for osteoporosis?
Fosamax and Boniva both work the same way to treat osteoporosis and require you to follow a set of rules closely in order for the medication to be as safe and effective as possible.Jan 29, 2021
Is walking good for osteoporosis?
You can prevent bone loss with regular exercise, such as walking. If you have osteoporosis or fragile bones, regular brisk walking can help to keep your bones strong and reduce the risk of a fracture in the future.Jan 17, 2018
What organs are affected by osteoporosis?
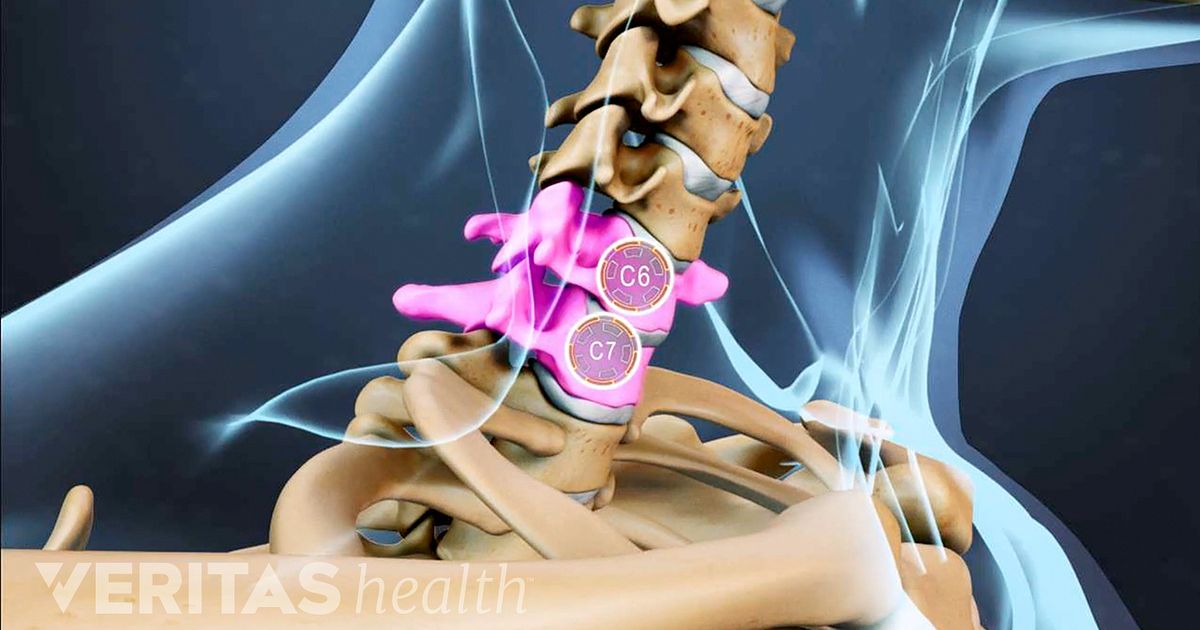
About 2 million fractures in the US each year are due to osteoporosis. Although all bones can be affected by the disease, the bones of the spine, hip, and wrist are most likely to break. In older people, hip fractures can be particularly dangerous.Jul 30, 2021
Should I worry if I have osteoporosis?
Talk with your doctor about an earlier scan if you have any warning signs or risk factors for osteoporosis: a bone fracture after age 50. sudden back pain. loss of height or increasingly stooped posture.
What activities should be avoided with osteoporosis?
Activities such as jumping, running or jogging can lead to fractures in weakened bones. Avoid jerky, rapid movements in general. Choose exercises with slow, controlled movements.
Are bananas good for osteoporosis?
As all these nutrients play an essential role for your health, they also improve your bone density. Eat pineapple, strawberries, oranges, apples, bananas and guavas. All these fruits are loaded with vitamin C, which in turn, strengthen your bones.Nov 6, 2017
What is the best fruit for bones?
FruitsBlackberries.Blueberries.Figs, dried, uncooked.Grapes.Kiwi fruit, fresh, raw.Mulberries.Plums, dried (prunes)Pomegranate juice.More items...•Jul 28, 2021
Which Medications Are Commonly Used For Osteoporosis Treatment?
Bisphosphonates are the most common medications prescribed for osteoporosis treatment. These include: 1. Alendronate (Fosamax) 2. Risedronate (Acto...
How Do Most Osteoporosis Medications Work?
With the exception of teriparatide, osteoporosis medications slow bone breakdown. Healthy bones continuously break down and rebuild.As you age — es...
How Do You Know If You're Taking The Right bisphosphonate?
Drugs in the bisphosphonate class are more alike than they are different. They all help maintain bone density. And, all bisphosphonates have been s...
When Might Other Osteoporosis Medications Be used?
Drugs such as denosumab, teriparatide and abaloparatide can be used by anyone with osteoporosis, but are more likely to be recommended for people w...
What Are Common Side Effects of Bisphosphonate pills?
Bisphosphonate pills aren't absorbed well in the stomach. The main side effects of bisphosphonate pills are stomach upset and heartburn. Generic fo...
Do Intravenous Bisphosphonates Have Advantages Over The Pill form?
Infused forms of bisphosphonates don't cause stomach upset. And it may be easier for some women to schedule a quarterly or yearly infusion than to...
Can Bisphosphonates Hurt Your Bones?
Long-term bisphosphonate therapy has been linked to a rare problem in which the upper thighbone cracks and may break. This injury, known as atypica...
How Long Should You Take A Bisphosphonate For Osteoporosis Treatment?
There's some uncertainty about how long to take bisphosphonates because of a lack of long-term studies. Bisphosphonates have been shown to be safe...
What Happens If You Break A Bone While Taking An Osteoporosis medication?
Osteoporosis medications lower the chance of fracture, but they don't eliminate all risk of breaking a bone. If you have a fracture while on treatm...
Can Medication Alone Successfully Treat Osteoporosis?
Don't rely entirely on medication as the only treatment for your osteoporosis. These practices also are important: 1. Exercise. Weight-bearing phys...
What is the best treatment for osteoporosis?
If you can't tolerate the more common treatments for osteoporosis — or if they don't work well enough — your doctor might suggest trying: Teriparatide (Forteo). This powerful drug is similar to parathyroid hormone and stimulates new bone growth. It's given by daily injection under the skin.
What supplements can help with osteoporosis?
Alternative medicine. There is limited evidence that certain supplements, such as vitamin K-2 and soy, can help lower fracture risk in osteoporosis, but more studies are needed to prove benefits and determine risks.
What is the complication of bisphosphonates and denosumab?
A very rare complication of bisphosphonates and denosumab is a break or crack in the middle of the thighbone. A second rare complication is delayed healing of the jawbone (osteonecrosis of the jaw). This can occur after an invasive dental procedure such as removing a tooth.
How long can you take teriparatide for osteoporosis?
After two years of treatment with teriparatide, another osteoporosis drug is taken to maintain the new bone growth. Abaloparatide (Tymlos) is another drug similar to parathyroid hormone. You can take it for only two years, which will be followed by another osteoporosis medication. Romosozumab (Evenity).
What is the newest bone building medication?
Romosozumab (Evenity). This is the newest bone-building medication to treat osteoporosis. It is given as an injection every month at your doctor's office. It is limited to one year of treatment, followed by other osteoporosis medications.
How often is denosumab shot?
Denosumab is delivered via a shot under the skin every six months. If you take denosumab, you might have to continue to do so indefinitely.
How to reduce the risk of osteoporosis?
Smoking increases rates of bone loss and the chance of fracture. Avoid excessive alcohol. Consuming more than two alcoholic drinks a day might decrease bone formation.
What is the best treatment for osteoporosis?
Bisphosphonates are commonly prescribed for osteoporosis treatment and prevention. The FDA has approved many bisphosphonates to prevent bone loss and fractures in post-menopausal women: alendronate (brand name Fosamax), etidronate (brand name Didronel), ibandronate (brand name Boniva), risedronate (brand name Actonel), tiludronate (brand name Skelid), pamidronate (brand name Aredia) and zoledronic acid (brand names Reclast and Zometa). Some are taken daily; others are formulated for weekly, monthly or yearly use. Bisphosphonates decrease the rate that bone is destroyed, a process called resorption, by stopping the activity of the cells that cause bone breakdown, called osteoclasts. This slows down the rate of bone loss. The drugs are also incorporated into newly formed bone and can persist in them for years, so the effects last well beyond the final treatment.
What hormones are used to treat osteoporosis?
Two other hormones have been approved to treat osteoporosis: teriparatide and abaloparatide. Teriparatide (brand name Forteo) is a lab-made derivative of human parathyroid hormone (PTH), and abaloparatide (band name Tymlos) is a derivative of human parathyroid hormone-related protein.
How has osteoporosis changed?
Osteoporosis treatment has radically changed in a relatively short period. In the early 1990s, women had few treatment options. Now, there are many different types of treatments available. This has created a dilemma for women trying to decide which, if any, of these medications they need. The NWHN believes that treatment should be focused on women ...
What is the name of the drug that stops bone breakdown?
Denosumab (brand name Prolia) osteoporosis medication (Amgen) Denosumab (brand name Prolia) is an osteoporosis medication that uses human monoclonal antibody. Approved in 2010, this drug works by targeting and inactivating osteoclasts to stop natural bone breakdown, or resorption, processes.
How do bisphosphonates affect bone?
Bisphosphonates decrease the rate that bone is destroyed, a process called resorption, by stopping the activity of the cells that cause bone breakdown, called osteoclasts. This slows down the rate of bone loss.
Can bisphosphonates cause jaw pain?
The jaw tissue of some women taking bisphosphonates dies (jaw necrosis), which can necessitate removal of an area of the jaw bone.
Where are fatty tissue injections given?
Both drugs are administered through injections into the fatty tissue, usually in the abdomen or thigh. These drugs have been shown to stimulate new bone formation and prevent fractures in women with osteoporosis. However, the absolute reduction in fractures in clinical trials of these drugs were very small, between 2-4%.
What is the treatment for osteoporosis in postmenopausal women?
Pharmacological treatments for postmenopausal women with osteoporosis are prescribed to decrease the risk of fragility fractures . Many drugs with different mechanisms of action have been approved for the prevention and treatment of osteoporosis, are effective and available worldwide. These medications must be used in conjunction with calcium ...
Is osteoporosis asymptomatic?
As osteoporosis is asymptomatic for most patients, and treatment efficacy is undetectable by them, effective communication between healthcare professionals and patients and early detection of non-adherence are required to improve patient’s adherence.
What is the best medicine for osteoporosis?
It’s said to increase bone strength and reduce fractures in the hip, spine, wrist, arm, leg, and ribs. Another osteoporosis med, raloxifene ( Evista) works like estrogen in keeping up your bone mass.
How to prevent osteoporosis?
However, there is no proof that these foods help prevent or delay osteoporosis. Exercise. Make it a habit to do weight-bearing activities such as running, walking, tennis, dancing, stair climbing, aerobics, and weightlifting. When you do this regularly, this helps your bone density, so your bones are stronger.
How to get more calcium at home?
For instance, you can add nonfat dry milk to everyday foods and beverages, including soups, stews, and casseroles. Each cup of dry milk adds about a third of the calcium you need each day.
What is the best medicine to take before eating?
Ibandronate ( Boniva), which is a pill that you need to take at least an hour before you eat or take any other meds. Risedronate ( Actonel, Atelvia), which is a pill that you need to take at least half an hour before you eat or take any other meds.
How many doses of Prolia are there?
It is an antsclerostin antibody and works mainly by increasing new bone formation. A dose is given as two injections, one after another. It is limited to only 12 doses which must be administered by your doctor. There’s also a biologic drug -- denosumab ( Prolia, Xgeva) -- for osteoporosis.
Can you take calcium supplements at the same time?
They can check that it won’t make it harder for your body to use any other medicines you take. Your doctor can also tell you if you need to take calcium supplements at a different time than your other medications.
Can hormone replacement therapy be used to treat osteoporosis?
But doctors don’t prescribe hormone replacement therapy to only prevent osteoporosis, due to potential health risks. In women who have been on hormone replacement therapy in the past and then stopped it, their bones start to thin again, at the same pace as during menopause. WebMD Medical Reference. Sources.
What is the new drug for osteoporosis?
A number of other osteoporosis drugs are in development, including a new monoclonal antibody (romosozumab) and drugs that block sclerostin, a protein that inhibits bone formation. However, Dr. Slovik doesn't think we're going to see any of these new drugs approved within the next year.
What is the best treatment for bone breakdown?
David Slovik, associate professor of medicine at Harvard Medical School and endocrinologist at Massachusetts General Hospital.
What is raloxifene used for?
Raloxifene (Evista), a selective estrogen receptor modulator (SERM), is perhaps best known for its role in breast cancer prevention and treatment, but it serves double duty in treating osteoporosis, too. It works by binding with estrogen receptors around the body to produce estrogen-like effects, one of which is to decrease bone turnover.
How to determine if you have osteoporosis?
Your doctor will determine whether you have osteoporosis by measuring your bone density —usually at the hip and spine—using dual energy x-ray absorptiometry (DEXA).
How long do women take bisphosphonates?
Doctors acknowledge that the risk of these side effects also increases with long-term use of bisphosphonates, so most women take these drugs for about five years. The good news is that the bone-protective benefits continue even after you stop taking bisphosphonates.
What is the process of breaking down old bone?
There's no one-size-fits-all answer. Understanding your options begins with knowing what's available. Throughout our lives, our bones undergo constant renovation. In a process called bone turnover, cells called osteoclasts break down and remove old bone, and then cells called osteoblasts lay down new bone.
Does calcitonin help with spinal fractures?
It's a hormone that binds to osteoclasts to prevent bone loss. When taken as a daily nasal spray or by injection, calcitonin can reduce spinal fractures, but it hasn't been shown effective for preventing other types of fractures and is not a first-line treatment for most women.
What is the best treatment for osteoporosis?
Bisphosphonates are the most common osteoporosis drug treatments. They’re typically the first treatments recommended for women who are postmenopausal. Examples of bisphosphonates include: ibandronate (Boniva), available as a monthly oral tablet or as an intravenous injection that you get four times per year.
How to prevent bone loss?
The most aggressive way to prevent additional bone loss is to take prescription medications.
What is the new antibody for bone formation?
The new antibody romosozumab (Evenity) helps to increase bone formation. It was approved by the Food and Drug Administration (FDA) in April of 2019. It’s intended for postmenopausal women with a high risk of fracture. This includes women who:
How often can you take ibandronate?
ibandronate (Boniva), available as a monthly oral tablet or as an intravenous injection that you get four times per year. risedronate (Actonel), available in daily, weekly, or monthly doses in an oral tablet. zoledronic acid (Reclast), available as an intravenous infusion that you get once every one or two years.
What vitamins are good for bone loss?
Even when you’re taking any of the medications listed above, doctors recommend getting plenty of calcium and vitamin D in your diet. That’s because this mineral and vitamin together can help slow bone loss.
Why do older people have a higher risk of osteoporosis?
As you age, you lose old bone at a faster rate than your body can replace it. Because of this, older people are at a higher risk of osteoporosis. Women also have a higher risk of developing osteoporosis because they typically have thinner bones than men.
What are some exercises that help strengthen the bones in your legs, hips, and lower spine?
This can mean free weights, weight machines, or resistance bands. Weight-bearing exercise like walking or jogging, and low-impact aerobics such as elliptical training or biking, can also be beneficial. Both can help strengthen the bones in your legs, hips, and lower spine.
What is the best treatment for osteoporosis?
Bisphosphonates: Most Commonly Prescribed For Osteoporosis. Bisphosphonates block the action of osteoclasts - responsible for breaking down bone tissue - thereby slowing bone loss. Bisphosphonates available in the U.S. include: Alendronate (Fosamax, Binosto): may be taken orally daily or a weekly tablet is also available.
How does osteoporosis medication work?
Some work by decreasing how fast bone is broken down, others increase the rate at which bone is built back up. Some can only be used in postmenopausal women.
What is the gold standard for menopausal hormone therapy?
Twenty-to-thirty years ago, menopausal hormone therapy (MHT) (previously called hormone replacement therapy [HRT]) was considered the gold standard for preventing not only osteoporosis but treating menopausal symptoms as well. That all changed after publication of the results of the Women's Initiative Trial in 2002 which showed the risks associated with MHT use (an increased risk of breast cancer, blood clots, heart attacks, and stroke) outweighed the benefits (decreased rates of hip and vertebral fractures and colon cancer).
What is the best bisphosphonate?
Bisphosphonates available in the U.S. include: 1 Alendronate (Fosamax, Binosto): may be taken orally daily or a weekly tablet is also available 2 Ibandronate (Boniva): can be taken orally monthly or given by intravenous injection every three months 3 Risedronate (Actonel, Atelvia): can be taken orally daily, weekly, bimonthly, or monthly 4 Zoledronic acid (Reclast, Zometa): given by intravenous infusion over at least 15 minutes once a year when used for treatment or once every two years when used for prevention.
What are some examples of hormonal treatments?
Examples of hormonal treatments include Premarin, estradiol, and Femhrt.
Why is calcitonin used for osteoporosis?
Other treatments are usually preferred over calcitonin for the prevention of osteoporosis because it is not clear if calcitonin increases bone density in areas other than the spine or if it prevents fractures. Calcitonin is also used to relieve sudden, intense pain caused by vertebral fractures.
How often should I take Risedronate?
Risedronate (Actonel, Atelvia): can be taken orally daily, weekly, bimonthly, or monthly. Zoledronic acid (Reclast, Zometa): given by intravenous infusion over at least 15 minutes once a year when used for treatment or once every two years when used for prevention.
What are the best medications for osteoporosis?
Which medications can help treat osteoporosis? 1 block the breakdown of bone (anti-resorptive therapies). Examples include bisphosphonates such as alendronate (Fosamax), which is a pill, and zoledronate (Reclast), which is given intravenously. Other types of anti-resorptive agents include raloxifene (Evista) and denosumab (Prolia). 2 enhance the formation of bone (anabolic therapies). Examples include teriparatide (Forteo) and abaloparatide (Tymlos).
When is romosozumab given?
September 07, 2019. Romosozumab is a welcome addition to our treatment options for postmenopausal women with osteoporosis who are at high risk of fracture. It results in rapid and profound increases in bone density and reduction in the risk of fractures after 1 year of treatment.
How many vertebral fractures did denosumab and romosozumab have?
The group that received romosozumab followed by denosumab had 21 vertebral fractures, compared to 84 in the group that received placebo followed by denosumab. Another trial enrolled more than 4,000 postmenopausal women with osteoporosis and a history of related fractures.
How long does romosozumab last?
The medication is injected once a month using two separate prefilled syringes for a full dose. Romosozumab should only be taken for one year, because its bone-making activity wanes after 12 months. Women using this therapy should also make sure they get enough calcium and vitamin D during treatment.
What are the effects of bone weakening?
As bone weakens, people are more likely to experience fractures, especially in the spine, hip, and forearm. This causes pain, diminishes a person’s ability to function, and reduces quality of life. Anything that can lower the risk of osteoporosis and fractures has major positive public health implications.
Does romosozumab inhibit bone formation?
Produced by osteocytes (bone cells), it inhibits bone formation (making new bone). Romosozumab binds sclerostin, which keeps it from blocking the signaling pathway for new bone formation. The result is an increase in new bone. To a lesser degree, it also decreases bone resorption (breakdown of bone).
Is teriparatide an anabolic agent?
Now, for the first time since 2010, a new class of medication is available to treat osteoporosis. Romosozumab (Evenity) is in a class called sclerostin inhibitors and is considered an anabolic agent. Sclerostin is a protein that helps regulate bone metabolism.
Overview
- RxAssist is a nationally recognized, web based medication assistance resource center. You can search the RXAssist website to find discounts or assistance programs available for the medications you take.
- Osteoporosis is a bone-weakening disease that frequently strikes women after menopause. The disease makes the bones less dense and susceptible to potentially disabling fractures in the spine and hip as well as other bones.
Prognosis
- Throughout our lives, our bones undergo constant renovation. In a process called bone turnover, cells called osteoclasts break down and remove old bone, and then cells called osteoblasts lay down new bone. After menopause, the rate of bone removal speeds up, and bone formation doesn't always keep pace. The net result can be bone loss and ultimately the weakened, brittle b…
- The optimal length of oral bisphosphonate therapy is unknown. One study found that women who take alendronate for five years followed by five years of placebo have no increased incidence of nonvertebral or hip fractures compared with women who take alendronate for 10 years. There is, however, an increase in vertebral fractures.38 Osteonecrosis of the jaw and atypical femoral fra…
- As osteoporosis decreases bone strength, patients are at an increased risk of fracture, often with minimal trauma, and commonly at the pelvis, hip and wrist.Oral bisphosphonates are the most commonly prescribed medications and are effective in reducing the risk of further osteoporotic fracture. There are a range of other medications that can also be used, including intravenous bis…
- Osteoporotic fragility fractures can cause substantial pain and severe disability, often leading to a reduced quality of life, and hip and vertebral fractures are associated with decreased life expectancy.Hip fracture nearly always requires hospitalisation, is fatal in 20% of cases and permanently disables 50% of those affected; only 30% of patients fully recover. Surgery carries ri…
Treatment
- Treatment recommendations are often based on an estimate of your risk of breaking a bone in the next 10 years using information such as the bone density test. If your risk isn't high, treatment might not include medication and might focus instead on modifying risk factors for bone loss and falls.
- The doctor will likely recommend medicine if you have To slow bone breakdown, many doctors first turn to one particular class of drugs. \"If someone has a very low T-score, we'll typically start with the bisphosphonates,\" says Dr. David Slovik, associate professor of medicine at Harvard Medical School and endocrinologist at Massachusetts General Hospital. There are several bisph…
- How much bone youve lost. Osteoporosis medicines work in different ways. A person with more severe bone loss or multiple broken bones may be recommended a different medicine than a person with less bone loss or no fractures. Types of medication given in a healthcare providers office or infusion center may include ibandronate (Boniva®), denosumab (Prolia®), and zoledro…
- The National Osteoporosis Foundation recommends treatment of postmenopausal women and men with a personal history of hip or vertebral fracture, a T-score of 2.5 or less, or a combination of low bone mass (T-score between 1 and 2.5) and a 10-year probability of hip fracture of at least 3% or any major fracture of at least 20% as calculated by the FRAX Fracture Risk Assessment T…
Signs And Symptoms
- Bone pain similar to that of arthritis may occur in the early course of the disease. Later, sharp pain may suddenly occur and become worse with activity or weight bearing. Fractures may occur, particularly in your spine, although you may not have fallen. These are called spontaneous fractures. These fractures compress the vertebrae in the spine and are the cause for loss of hei…
- Osteoporosis can cause the bones that make up the spine (the vertebrae) to break. This causes the spine to collapse in these areas, which leads to pain, difficulty in moving and gradual deformity. If the problem is severe enough, it causes a \"dowager's hump\" to form, a curvature of the upper back. Symptoms of bone loss do not occur until osteoporosis develops. Even then, in i…
- Osteoporosis generally does not become clinically apparent until a fracture occurs. Two thirds of vertebral fractures are painless. Typical findings in patients with painful vertebral fractures may include the following: 1. The episode of acute pain may follow a fall or minor trauma. 2. Pain is localized to a specific, identifiable, vertebral level in the midthoracic to lower thoracic or upper lu…
- Osteoarthritis is a painful, degenerative joint disease that often involves the hips, knees, neck, lower back, or the small joints of the hands. Osteoarthritis usually develops in joints that are injured by repeated overuse in the performance of a particular job or a favorite sport or from carrying around excess body weight. Eventually this injury or repeated impact thins or wears aw…
Diagnosis
- Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of mineral in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only a few bones are checked — usually in the hip and spine.
- Your doctor will determine whether you have osteoporosis by measuring your bone densityusually at the hip and spineusing dual energy x-ray absorptiometry (DEXA). The result, expressed as a number called a T-score, compares your bone density with that of a healthy 30-year-old woman.
- The outward signs of osteoporosis (height loss, easily broken bones, dowager's hump) combined with a patient's gender and age are strong signs that the patient has osteoporosis. A technology called dual X-ray absorptiometry (DXA) is the state-of-the-art technique for measuring bone mineral density (how much calcium is in the bones) and to diagnose osteoporosis.
- Osteoporosis is diagnosed radiographically based on bone mineral density (BMD) determinations from dual energy x-ray absorptiometry (DEXA) assessment.4 Although quantitative calcaneal ultrasonography and peripheral DEXA can also predict fracture risk, these modalities do not correlate well enough with central DEXA to be used diagnostically.1,5,6 The World Health Organi…
Prevention
- Weight-bearing exercise, such as walking or jogging, riding stationary bicycles, using rowing machines, or lifting weights, helps promote bone strength. A diet rich in calcium and vitamin D is important for bone development, as well as for some of the medications for prevention or treatment to work to their fullest capacity. Vitamin D is also gained from short exposure to sunli…
- The best way to get enough calcium every day is to eat a variety of healthy foods from all the different food groups. Getting enough vitamin D every day from foods like enriched milk or from natural sunlight is important to help the body absorb and use calcium from food. The U.S. Preventive Services Task Force recommends a bone density screening by DXA in all women age…
- The good news is there are many steps that can be taken to prevent and diagnosis osteoporosis. It's now a largely treatable condition and, with a combination of lifestyle changes and appropriate medical treatment, many fractures can be avoided.
Cause
- Osteoporosis occurs when the body fails to form enough new bone, when too much old bone is reabsorbed by the body, or both. Women are at a greater risk than men, especially women who are elderly, thin, or small. Other risk factors include the following:
- Bones are constantly being remodeled every day, and calcium is moving in and out of them. In children and adolescents, the body builds new bone faster than it breaks down old bone so total bone mass increases. This continues until about age 30, when new bone formation and old bone breakdown start occurring at about the same rate. In older adults, especially in post-menopausa…
- As we age some of our bone cells begin to dissolve bone matrix (resorption), while new bone cells deposit osteoid (formation). This process is known as remodeling. For people with osteoporosis, bone loss outpaces the growth of new bone. Bones become porous, brittle and prone to fracture. For more detailed information see Pathophysiology: Biological Causes of Osteoporosis.
- Primary osteoporosis is related to aging and loss of gonadal function. Secondary osteoporosis is caused by other health conditions (Table 4).2 Up to 30% of osteoporosis cases in postmenopausal women are estimated to be from a secondary cause.10 The estimate climbs to greater than 50% in men, premenopausal women, and perimenopausal women if vitamin D defici…
Epidemiology
- Approximately 12 million Americans over age 50 have osteoporosis. Post-menopausal white and Asian women are at the highest risk for osteoporosis. According to the National Institutes of Health, half of all women over age 50 and a quarter of men older than age 50 will break a bone due to osteoporosis. About 25 percent of women with osteoporosis will develop a vertebral defo…
- Around the world, 1 in 3 women and 1 in 5 men aged fifty years and over are at risk of an osteoporotic fracture. In fact, an osteoporotic fracture is estimated to occur every 3 seconds. The most common fractures associated with osteoporosis occur at the hip, spine and wrist. The likelihood of these fractures occurring, particularly at the hip and spine, increases with age in bot…
- 1. In England and Wales more than 2 million women have osteoporosis. 2. In England and Wales there are around 180,000 fractures per year due to osteoporosis. 3. 1 in 3 women and 1 in 5 men will have an osteoporotic fracture in their lifetime. 4. Osteoporosis is in general an age-related disease. Bone formation initially exceeds bone resorption but by the third decade this has revers…
- Osteoporosis is a common condition. Bone is living tissue that is in a constant state of regeneration. The body removes old bone (called bone resorption) and replaces it with new bone (bone formation). By their mid-30s, most people begin to slowly lose more bone than can be replaced. As a result, bones become thinner and weaker in structure. This accelerates in wome…
Management
- As osteoporosis is an asymptomatic condition, management is centred on preventing fragility fractures, which are associated with enormous morbidity and mortality. Treatment for osteoporosis should include not only drug treatment but also advice on lifestyle, nutrition, exercise and measures to reduce falls. Advise on smoking cessation where indicated, and mode…
- Lifestyle modification for prevention of osteoporotic fractures includes the following : 1. Increasing weight-bearing and muscle-strengthening exercise 2. Ensuring optimum calcium and vitamin D intake as an adjunct to active antifracture therapy The NOF recommends that pharmacologic therapy should be reserved for postmenopausal women and men aged 50 years …
- Fractures of the hip that occur as a consequence of osteoporosis are managed surgically through: 1. Joint replacement. Joint replacement is a surgery to replace all or part of a joint with a man-made joint called prosthesis. 2. Closed or open reduction with internal fixation. Open reduction, internal fixation involves the implementation of implants to guide the healing process of a bone, …
- According to Kurt Kennel, M.D., an endocrinology specialist from the Mayo Clinic, the most common medications used to manage osteoporosis are biphosphonates, such as Fosamax, Boniva, Actonel, Atelvia, Reclast, and Zometa. It is also a common practice to use hormones, like estrogen, to help treat and prevent osteoporosis. Some women do not elect to use these hormo…
Other Factors
- Beyond gender, risk factors for osteoporosis include: 1. Early menopause 2. Race white, Asian 3. Smoker 4. Thin frame 5. Steroid use 6. Exposure to breast cancer drugs 7. Age 8. Prior fracture as adult 9. Parental history of hip fracture 10. Vitamin D deficienciesIn Americans over age 50, osteoporosis is most common in women of European or Asian descent. Nearly half have low bo…
- Some women and men are more at risk for osteoporosis.Those who are on certain medications (including steroids, certain cancer treatment medications, excess thyroid hormones, anti-seizure medicines, and heparin) that can cause bone loss: 1. Women who are past menopause or who went through menopause before age 45 2. Caucasian or Asian women 3. Tthose with a small, th…
- A number of factors can increase the likelihood that you'll develop osteoporosis — including your age, race, lifestyle choices, and medical conditions and treatments.
- Other lifestyle factors that can help prevent osteoporosis include: 1. quitting smoking - cigarette smoking is associated with an increased risk of osteoporosis 2. limiting your alcohol intake - the recommended daily limit is no more than two standard drinks on any day. It is important to also avoid binge drinking.