Treatment 5.1. Restorations, Crowns, and Veneers Crowns may be placed to widen the clinical crown which may camouflage the exposed root surface 5.2. Construction of Gingival Mask Patients who have several teeth with recession may have unaesthetic appearance because of black triangles.
What are the treatments for gum recession?
Mild cases of gum recession may be improved with nonsurgical treatments, such as topical antibiotics, dental bonding or orthodontics. In most instances, however, gum recession surgery is needed to fully correct the problem. Nonsurgical treatments. Nonsurgical treatments for gum recession may include: Topical antibiotics.
How can we avoid dehiscence and recession during orthodontic treatment?
May 10, 2022 · Dental adhesives (also called dentin bonding agents) are light-cured resins that can be used as desensitizers by depositing resin tags and covering exposed dentinal tubules. However, dentin bonding agents are hydrophobic agents that should be placed in a dry field. Another option for desensitization is the use of a dental laser.
Can orthodontic treatment prevent gingival recession?
Dec 13, 2013 · If the gum recession is severe, gum grafting is another option to reinforce the residual tissues; covering the exposed tooth root. If the tooth decay caused due to gum recession is much, then a dental bone grafting is favourable. With tooth recession of more than 1.5mm in deepness, consult your periodontist; most likely a gingival flap surgery would be prescribed to …
What is a ‘dental recession’?
Oct 02, 2012 · When the recession is caused by frenal pull in those cases, frenectomy is advised. If appropriate hygiene aids do not enable the patient to maintain the area plaque free, then frenectomy is advised to give ease to entrance to the site [ 15 ]. 5.5. Surgical Root Coverage Techniques Free epithelialised gingival graft [ 16 ].

How do you fix a dental recession?
- Bone Regeneration - Regenerative surgery is needed when you've lost bone and gum tissue. ...
- Tissue Graft - If too much gum material has been lost, a gum tissue graft may be needed to restore the gums.
What is the best treatment for gum recession?
Can a dentist treat gum recession?
What can be done for exposed tooth root?
- Crown. A dental crown is a cap for your tooth that can protect and strengthen it. ...
- Gingival mask. If you have several teeth with gum recession, your dentist may recommend a gingival mask. ...
- Gum graft. ...
- Flap surgery.
How do you fix gum recession without surgery?
- Scaling and Root Planing. An important goal in the treatment of gum disease is to rid the teeth and gums of pathogenic bacteria and the toxins they produce, which may become incorporated into the root surface of the teeth. ...
- Antibiotics/Antimicrobials. ...
- Bite Adjustment. ...
- Oral Hygiene.
Can receding gums be repaired without surgery?
What is the best antibiotic for gum infection?
...
Penicillins are a group of antibiotics including:
- Penicillin.
- Amoxicillin.
- Amoxicillin/potassium clavulanate.
Does mouthwash help receding gums?
Therapeutic mouthwash helps prevent gum recession and disease, reduces the rate of tartar buildup, reduces the amount of plaque on your teeth, and removes food particles trapped between teeth and elsewhere in the mouth.Feb 19, 2020
How do you prevent gum recession from getting worse?
Can exposed tooth roots be fixed?
What happens if a tooth root is exposed?
Can an exposed tooth nerve fix itself?
What is recession in dentistry?
Dental Recession is a common treatable condition often seen at St. Lawrence Dentistry. In health the gum (gingival) margin normally extends about 1mm above the ‘cementoenamel junction’ or ‘CEJ’.
What is the most widely accepted classification of dental recession?
The most widely accepted classification of dental recession is the Miller system. Dr. Hawryluk will diagnose what recession category your teeth fall into. The key to understanding the classification system us to familiar with the term ‘mucogingival junction’. This is is an anatomical feature found on the intraoral mucosa. The mucosa of the cheeks and floor of the mouth are freely moveable and fragile, whereas the mucosa around the teeth and on the palate are firm and keratinized. Where the two tissue types meet is known as a mucogingival junction. The Miller classes are as follows:
What is a Class 2 gum recession?
Class 2: Recession that extends to or beyond the mucovingival junction, with no interdental bone loss. Dental grafting can many times regain all or almost all of the original gum present. Class 3: Recession that extends to or beyond the mucogingival junction, with some periodontal bone loss.
What is the CEJ of a tooth?
The CEJ is the location where the enamel, which covers the anatomical crown of a tooth, and the cementum, which covers the anatomical root of a tooth, meet. Gum recession is the shift of the gum below the CEJ toward the root of the tooth. By definition, recession results in the exposure of cementum portion of the tooth.
When does recession occur?
Recession usually occurs in people older than the age of 30 on the front aspect of teeth; it occurs less frequently on the back of teeth, and rarely in between teeth. Recession may be localized or generalized and often occurs during periods of inflammation that are combined with bad habits (improper tooth brushing technique, fingernail injuries). It appears more on teeth which are prominently located and on teeth which have very thin gum tissue.
Can a recession of the gums be grafted?
Gum recession begins as a small oval defect but may progress to expose the entire root. St. Lawrence Dentistry offers grafting procedures to treat dental recession can recover the root of the tooth with new gum tissue.
Can grafting regain gum?
Dental grafting can usually regain some of the lost gum but it is sometimes not as successful as treating as in a class II situation. Class 4: Recession that extends to or beyond the mucogingival junction, with severe bone and/or soft-tissue loss in the interdental area and/or severe malpositioning of the teeth.
What is the best treatment for gum recession?
If the gum recession is severe, gum grafting is another option to reinforce the residual tissues; covering the exposed tooth root. If the tooth decay caused due to gum recession is much, then a dental bone grafting is favourable.
Can gingivitis cause recession?
Dental Treatments for Gingival (Gum) Recession – Exposed Tooth Root! Gingival recession, a tooth root surface exposure, is simply caused by collapsed gum tissues. Yes, true! It should immediately be treated not only for pain relief but also to preserve healthier tooth life. It causes many other oral disorders such as tooth decay/cavity, gingivitis, ...
Can periodontal recession cause tooth pain?
Yes, true! It should immediately be treated not only for pain relief but also to preserve healthier tooth life. It causes many other oral disorders such as tooth decay/cavity, gingivitis, aching jaw, lighter-to-heavier tooth pain and other periodontal worsening; if the recession continues, the periodontal ligaments may get damaged;
What is gingival recession?
Gingival recession is a problem affecting almost all middle and older aged to some degree. Gingival recession is the apical migration of gingival margin to the cementoenamel junction (CEJ). The distance between the CEJ and gingival margin gives the level of recession.
Which group has more gingival recession?
The people who smoke have more gingival recession than nonsmokers.
What does it mean when a tooth erupts close to the mucogingival line?
Tooth which erupts close to mucogingival line may show localised gingival recession as there may be very little or no keratinized tissue [6].
What is the goal of periodontal therapy?
The main goal of periodontal therapy is to improve periodontal health and thereby to maintain a patient's functional dentition right through his/her life. However, aesthetics symbolize an inseparable part of today's oral therapy, and numerous procedures have been proposed to preserve or enhance patient aesthetics.
What age group is most affected by ingival recession?
Gingival recession is associated with the presence of supragingival and subgingival calculus and showed that the lingual surfaces of the lower anterior teeth were most frequently affected in 20–34 year age group in Tanzanian adult population [3].
How many root surfaces are exposed to oral environment?
Patients on periodontal maintenance with an average of 64.7 exposed root surfaces per patient; the mean number of caries lesions which were detected were 4.3 in a prevalence study [14].
What is the prevalence of recession in the youngest cohort?
In the youngest age cohort (30 to 39 years), the prevalence of recession was 37.8% and the extent averaged 8.6% teeth. In contrast, the oldest cohort, aged 80 to 90 years, had a prevalence of 90.4% (more than twice as high) and the extent averaged 56.3% teeth (more than six times as large) [2].
What is a gingival recession?
Gingival recession is represented by atrophic periodontal changes. The term "atrophy" makes reference to all processes of cell lesion characterized by a decrease in volume and cell population of a given organ or tissue, resulting from sublethal cell aggression, such as hypoxia, mechanical compression, local reduced vascularization, among others. Sublethal cell aggression is essentially reversible.
How to reduce gingival enlargement?
This will decrease gingival enlargement caused by inflammatory infiltrate and exudate accumulation, which allows the sites to be subjected to surgery to become better outlined. The patient will notice that root exposure did not result from treatment, but rather from getting rid of the problem.
Why is there a stretch of periodontal fibers?
Also due to the increase in functional demand, caused by excessive occlusal load, there is an intense and continuous stretch of periodontal fibers, especially those attached to the most cervical region of the alveolar bone crest. This overload might cause occasional collagenous fiber structures to break, in addition to over stressing periodontal ligament cells and, as a result, significantly increasing the cervical local levels of chemical mediators released by those cells, especially mediators associated with bone resorption, thereby promoting bone loss, whether vertical or angled, on the periodontal surface of the alveolar bone crest.
What happens to the root after periodontal treatment?
After periodontal treatment and once the causes have been eliminated, the exudate will undergo resorption while inflammatory cells will undergo migration, with a decrease and retraction of gingival tissue volume. During the repair process, root will become exposed to the oral environment.
What is a U-shaped recession?
U-shaped gingival recession associated with inadequate tooth brushing, with cervical abrasion of maxillary canines and premolars. Recession is more severe in mandibular premolars.
Is gingival recession a part of aging?
For decades, it was believed that gingival recession was a part of human aging processes; however, all evidence supporting such a statement are quite weak. Aging might increase the possibility for the causes of gingival retraction to act, but that does not mean they are inherent to aging.
Is "recession" a synonym for "retraction"?
Within our specialty, the term "gingival recession" is indistinctly used as a synonym for gingival retraction, although some researchers prefer using one rather than the other. In dictionaries, it is possible to find: 1) recession = the act or effect of moving back, withdraw; 2) retraction = the act or effect of retracting; 3) retract = to pull back, to draw back, withdraw. In the present article, we take both terms as synonyms.
What is an exposed tooth root?
The portion of your tooth that is naturally above the gumline is the crown, which is covered by a hard white substance enamel. The part of your tooth that should be anchored in the bone and covered with gum tissue is called the root. Generally, 1/3rd of the tooth is visible and 2/3rds of the tooth is under the gum and bone.
What are the symptoms of an exposed tooth root?
Sometimes even very tiny amounts of root exposure can cause sensitivity with tooth brushing, or when eating and drinking cold, acidic, sour, or sweet foods and drinks. Occasionally the gum will be tender or swollen. Some people have no symptoms at all.
Why are exposed roots and gum recession concerning?
If you can see the root of your tooth, there is less bone holding your tooth in place. Also, the crowns of your teeth are protected by dental enamel, while the roots of your teeth are not. That inner layer of the tooth is known as dentin, which is more much more prone to cavities and sensitivity.
What causes an exposed root?
Teeth can have exposed roots for many reasons including gum disease, grinding, trauma, tobacco use, tooth position, orthodontics, and genetics.
Does brushing too hard cause gum recession?
Overly aggressive tooth brushing can worsen gum recession, but it is usually not the primary cause. If exposed roots were caused by brushing too hard, the gum recession would be mostly even throughout the entire mouth, which is rarely the case. However, soft-bristled toothbrushes are strongly recommended.
Are exposed roots normal with aging?
Exposed roots and gum recession are not a normal, inevitable consequence of aging, although it is more common to see gum recession in older people. This is because all the damage to your teeth and gums is cumulative over your lifetime, so anything that happened when you were younger will be visible as you age unless you have had it repaired.
How do you treat an exposed root?
Once the gum is gone, the only way to get it back is to have it surgically covered back up with a gingival graft. Donor tissue (either from the roof of the mouth, or from an alternative source like cadaver tissue) is used to cover the exposed root.
Why do patients with gingival recession seek treatment?
Patient Concerns — Unsatisfactory esthetics is a major reason why patients with gingival recession seek treatment. Hypersensitivity is another chief concern, and it has been shown to be significantly reduced following root coverage procedures.4,12 In some cases, however, a complete resolution of root sensitivity may require additional treatment, such as a Class V restoration. In areas of root sensitivity with minimal gingival recession, nonsurgical treatment should be explored before surgical root coverage is presented as an option. Figure 8 illustrates generalized gingival recession in a patient who presented with esthetics as a chief complaint.
How to describe gingival recession?
After reading this course, the participant should be able to: 1 Discuss the percentage of patients presenting with gingival recession, and explain the importance of determining etiology. 2 Describe systems for categorizing various factors associated with gingival recession. 3 Explain why patients seek treatment for gingival recession, management strategies and possible interventions.
What are the factors that contribute to gingival recession?
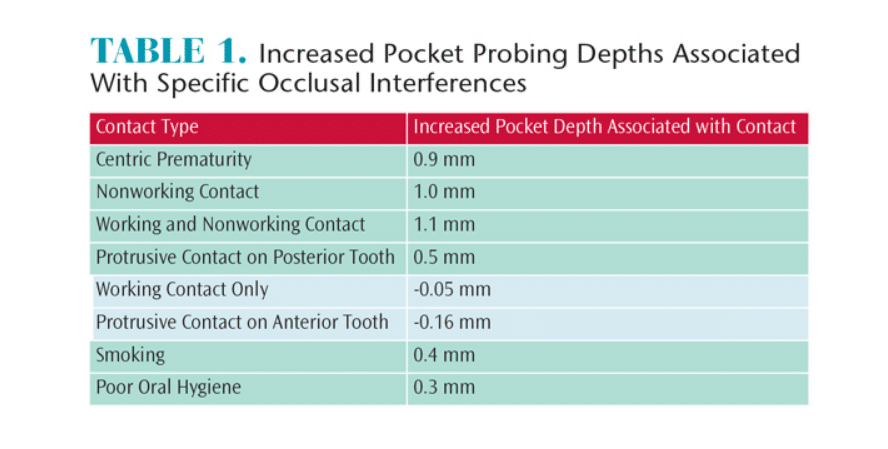
Chan et al4 categorize the etiological factors of gingival recession under predisposing factors and precipitating factors (Table 1). Although predisposing factors are mainly linked to anatomical factors — such as presence of underlying bone and thickness of the gingival biotype — inflammation can also be implicated. Additional anatomical predisposing factors include frenal pull (Figure 1) and a lack of adequate keratinized gingiva.5 Studies that compared sites with insufficient attached mucosa noted that attachment loss or recession did not progress over time.6 However, in a recent meta-analysis evaluating 1647 sites of buccal gingival recession, 78.1% experienced a progression in gingival recession at follow up (≥ 24 months). Pooled estimates showed increased odds of recession developing long term (odds ratio 2.43; p=0.03) or number of sites with gingival recession (odds ratio 2.16; p=0.0005). The authors concluded that untreated gingival recession has a high probability of progressing, even in the presence of optimal home care.7 Figures 2A through 2C demonstrate the progression of gingival recession without treatment.
What is gingival recession?
Gingival recession is associated with oral exposure of the root surface due to a displacement of the gingival margin apical to the cementoenamel junction. 1 This is a fairly common clinical condition, and research indicates it presents in at least one or more tooth surfaces in 23% of U.S. adults between 30 and 90 years of age. 2 According to the classification system developed by the American Academy of Periodontology, mucogingival deformities and conditions around teeth and edentulous ridges 3 include gingival/mucosal tissue recession, lack of keratinized gingiva, decreased vestibular depth, aberrant frenal pull/muscle position, gingival excess and abnormal color. While this article will focus on key aspects of gingival recession, it will not discuss decreased vestibular depth, gingival excess or abnormal color.
What is mucogingival therapy?
According to the American Academy of Periodontology’s “Parameters on Mucogingival Conditions,”20 therapeutic goals of mucogingival therapy are defined as nonsurgical and/or surgical correction of defects in morphology, position, and/or amount of soft tissue and underlying bone. This may be accomplished through a variety of procedures — including soft-tissue grafting for root coverage or gingival augmentation using alloplasts — and by controlling etiologic factors (including iatrogenic factors).
Does overzealous oral hygiene cause gingival recession?
PRECIPITATING FACTORS. Although lack of oral hygiene and subsequent inflammation are precipitating factors in gingival recession, overzealous oral hygiene can also have negative effects on gingiva. The results of traumatic toothbrushing most commonly present as recession on the facial of teeth prominent in the arch.4 Figure 3 illustrates gingival ...
Is gingival recession a primary indication?
While there are several indications for treatment of gingival recession, esthetic concern is a primary indication, according to Cairo, et al. 10