What is the best and safest treatment for osteoporosis?
Aug 13, 2020 · Which osteoporosis medications are usually tried first? Alendronate (Fosamax), a weekly pill. Risedronate (Actonel), a weekly or monthly pill. Ibandronate (Boniva), a monthly pill or quarterly intravenous (IV) infusion. Zoledronic acid (Reclast), an annual IV infusion.
What are the medications for treating osteoporosis?
12 rows · The AACE/ACE recommends denosumab as first-line therapy for patients at high risk of fracture and ...
Which is better for osteoporosis?
Aug 17, 2020 · Plenty of fruits and vegetables. An appropriate amount of calories for your age, height, and weight. Your health care provider or doctor can help you determine the amount of calories ... Foods and liquids that include calcium, vitamin D, and protein. These help minimize bone loss and maintain ...
How long does Reclast IV stay in your body?
Exercise is an important part of an osteoporosis treatment program. During childhood and adulthood, exercises such as walking, dancing, or weight lifting can make bones stronger. For older adults, regular exercise can help: Keep muscles strong and improve coordination and balance. This can help lower your chance of falling. Keep your independence.
How osteoporosis is usually treated?
How is osteoporosis treated? Treatments for established osteoporosis may include exercise, vitamin and mineral supplements, and medications. Exercise and supplementation are often suggested to help you prevent osteoporosis. Weight-bearing, resistance and balance exercises are all important.Apr 27, 2020
Can osteoporosis be cured or treated?
Osteoporosis affects many people all over the world, and although there isn't currently a cure, treatments are available. Medications, hormone therapy, and exercise can strengthen your bones and slow bone loss. If you have osteoporosis, talk to your doctor.
What is the life expectancy of a person with osteoporosis?
The average life expectancy of osteoporosis patients is in excess of 15 years in women younger than 75 years and in men younger than 60 years, highlighting the importance of developing tools for long-term management.
What is the latest treatment for osteoporosis?
FDA approves new treatment for osteoporosis in postmenopausal women at high risk of fracture. The U.S. Food and Drug Administration today approved Evenity (romosozumab-aqqg) to treat osteoporosis in postmenopausal women at high risk of breaking a bone (fracture).Apr 9, 2019
What not to eat if you have osteoporosis?
Foods to limit or avoidHigh-salt foods.Alcohol. While a moderate amount of alcohol is considered safe for those with osteoporosis, excess alcohol can lead to bone loss. ... Beans/legumes. While beans have some healthy attributes for women with osteoporosis, they're also high in phytates. ... Wheat bran. ... Excess vitamin A. ... Caffeine.
What does osteoporosis pain feel like?
Compression Fractures and Osteoporosis Pain Sudden, severe back pain that gets worse when you are standing or walking with some relief when you lie down. Trouble twisting or bending your body, and pain when you do. Loss of height. A curved spine called kyphosis, also known as a “dowager's hump.”Nov 23, 2020
Should I worry if I have osteoporosis?
Talk with your doctor about an earlier scan if you have any warning signs or risk factors for osteoporosis: a bone fracture after age 50. sudden back pain. loss of height or increasingly stooped posture.
Is walking good for osteoporosis?
You can prevent bone loss with regular exercise, such as walking. If you have osteoporosis or fragile bones, regular brisk walking can help to keep your bones strong and reduce the risk of a fracture in the future.Jan 17, 2018
What organs are affected by osteoporosis?
About 2 million fractures in the US each year are due to osteoporosis. Although all bones can be affected by the disease, the bones of the spine, hip, and wrist are most likely to break. In older people, hip fractures can be particularly dangerous.Jul 30, 2021
What is the fastest way to increase bone density?
10 Natural Ways to Build Healthy BonesEat Lots of Vegetables. ... Perform Strength Training and Weight-Bearing Exercises. ... Consume Enough Protein. ... Eat High-Calcium Foods Throughout the Day. ... Get Plenty of Vitamin D and Vitamin K. ... Avoid Very Low-Calorie Diets. ... Consider Taking a Collagen Supplement. ... Maintain a Stable, Healthy Weight.More items...•Jan 18, 2017
What is the best kind of doctor to treat osteoporosis?
Rheumatologists treat patients with age-related bone diseases. They can diagnose and treat osteoporosis. Endocrinologists, who see patients with hormone-related issues, also manage the treatment of metabolic disorders such as osteoporosis. Orthopedic surgeons may fix fractures.
What is the monthly injection for osteoporosis?
How is romosozumab given? The medication is injected once a month using two separate prefilled syringes for a full dose. Romosozumab should only be taken for one year, because its bone-making activity wanes after 12 months.Jul 17, 2019
What is the best treatment for osteoporosis?
If you can't tolerate the more common treatments for osteoporosis — or if they don't work well enough — your doctor might suggest trying: Teriparatide (Forteo). This powerful drug is similar to parathyroid hormone and stimulates new bone growth. It's given by daily injection under the skin.
How to reduce the risk of osteoporosis?
Smoking increases rates of bone loss and the chance of fracture. Avoid excessive alcohol. Consuming more than two alcoholic drinks a day might decrease bone formation.
What is the complication of bisphosphonates and denosumab?
A very rare complication of bisphosphonates and denosumab is a break or crack in the middle of the thighbone. A second rare complication is delayed healing of the jawbone (osteonecrosis of the jaw). This can occur after an invasive dental procedure such as removing a tooth.
How long can you take teriparatide for osteoporosis?
After two years of treatment with teriparatide, another osteoporosis drug is taken to maintain the new bone growth. Abaloparatide (Tymlos) is another drug similar to parathyroid hormone. You can take it for only two years, which will be followed by another osteoporosis medication. Romosozumab (Evenity).
What is the newest bone building medication?
Romosozumab (Evenity). This is the newest bone-building medication to treat osteoporosis. It is given as an injection every month at your doctor's office. It is limited to one year of treatment, followed by other osteoporosis medications.
How often is denosumab shot?
Denosumab is delivered via a shot under the skin every six months. If you take denosumab, you might have to continue to do so indefinitely.
How to prevent falling?
Prevent falls. Wear low-heeled shoes with nonslip soles and check your house for electrical cords, area rugs and slippery surfaces that might cause you to fall.
Abstract
Approximately 10 million men and women in the U.S. have osteoporosis, 1 a metabolic bone disease characterized by low bone density and deterioration of bone architecture that increase the risk of fractures. 2 Osteoporosis-related fractures can increase pain, disability, nursing home placement, total health care costs, and mortality.
INTRODUCTION
Osteoporosis is a bone disorder that increases a person’s risk of fracture due to low bone mineral density (BMD), impaired bone microarchitecture/mineralization, and/or decreased bone strength.
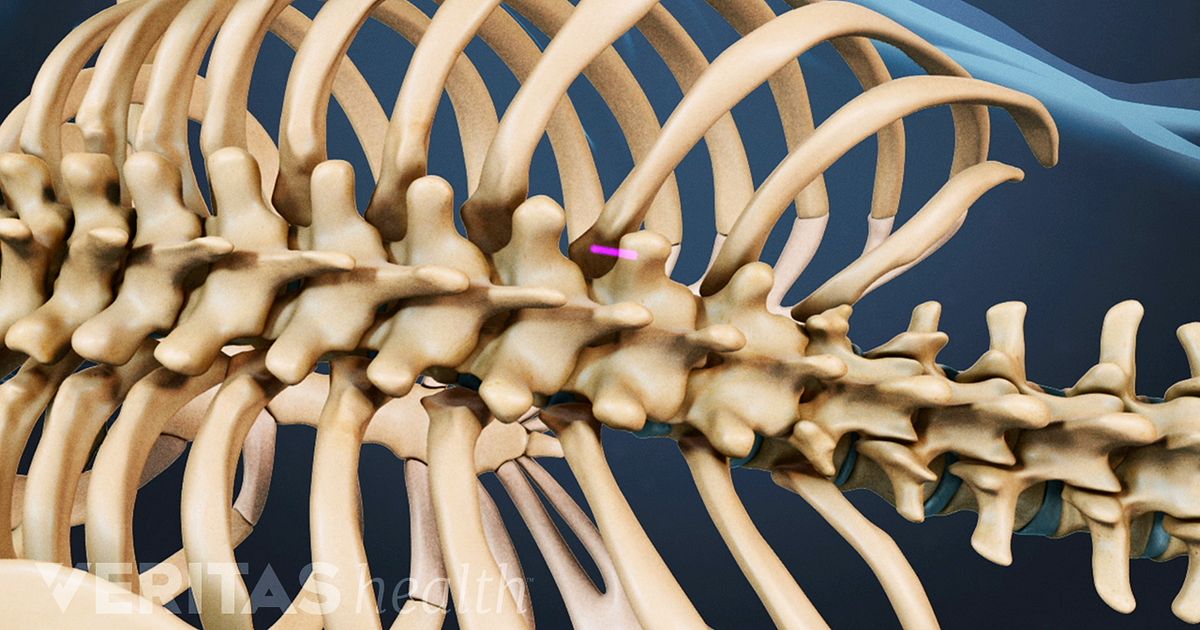
PATHOPHYSIOLOGY
Bones provide structure for the body, protection for the organs, and storage for minerals, such as calcium and phosphorus, that are essential for bone development and stability. Individuals continue to build bone and will reach peak bone mass at about 30 years of age, after which they begin to lose bone mass steadily.
ETIOLOGY
Primary osteoporosis is often associated with age and sex hormone deficiency. Age-related osteoporosis results from the continuous deterioration of the trabeculae in bone. In addition, the reduction of estrogen production in post menopausal women causes a significant increase in bone loss.
SCREENING AND DIAGNOSIS
Published osteoporosis screening guidelines vary greatly. In general, most organizations recommend that all adults older than 50 years of age with a history of fracture receive BMD screening.
SELECT GUIDELINES AND RECOMMENDATIONS
In a systematic review, Solomon et al. looked at 18 osteoporosis guidelines, among them those of the NOF, the ACR, and the American Association of Clinical Endocrinologists and American College of Endocrinology (AACE/ACE).
NONPHARMACOLOGICAL MANAGEMENT
Nonpharmacological management of osteoporosis includes adequate calcium and vitamin D intake, weight-bearing exercise, smoking cessation, limitation of alcohol/caffeine consumption, and fall-prevention techniques. 2 – 6, 9, 18, 34
What is the best treatment for osteoporosis?
Bisphosphonates are commonly prescribed for osteoporosis treatment and prevention. The FDA has approved many bisphosphonates to prevent bone loss and fractures in post-menopausal women: alendronate (brand name Fosamax), etidronate (brand name Didronel), ibandronate (brand name Boniva), risedronate (brand name Actonel), tiludronate (brand name Skelid), pamidronate (brand name Aredia) and zoledronic acid (brand names Reclast and Zometa). Some are taken daily; others are formulated for weekly, monthly or yearly use. Bisphosphonates decrease the rate that bone is destroyed, a process called resorption, by stopping the activity of the cells that cause bone breakdown, called osteoclasts. This slows down the rate of bone loss. The drugs are also incorporated into newly formed bone and can persist in them for years, so the effects last well beyond the final treatment.
What hormones are used to treat osteoporosis?
Two other hormones have been approved to treat osteoporosis: teriparatide and abaloparatide. Teriparatide (brand name Forteo) is a lab-made derivative of human parathyroid hormone (PTH), and abaloparatide (band name Tymlos) is a derivative of human parathyroid hormone-related protein.
How has osteoporosis changed?
Osteoporosis treatment has radically changed in a relatively short period. In the early 1990s, women had few treatment options. Now, there are many different types of treatments available. This has created a dilemma for women trying to decide which, if any, of these medications they need. The NWHN believes that treatment should be focused on women ...
What is the name of the drug that stops bone breakdown?
Denosumab (brand name Prolia) osteoporosis medication (Amgen) Denosumab (brand name Prolia) is an osteoporosis medication that uses human monoclonal antibody. Approved in 2010, this drug works by targeting and inactivating osteoclasts to stop natural bone breakdown, or resorption, processes.
How do bisphosphonates affect bone?
Bisphosphonates decrease the rate that bone is destroyed, a process called resorption, by stopping the activity of the cells that cause bone breakdown, called osteoclasts. This slows down the rate of bone loss.
Can bisphosphonates cause jaw pain?
The jaw tissue of some women taking bisphosphonates dies (jaw necrosis), which can necessitate removal of an area of the jaw bone.
Where are fatty tissue injections given?
Both drugs are administered through injections into the fatty tissue, usually in the abdomen or thigh. These drugs have been shown to stimulate new bone formation and prevent fractures in women with osteoporosis. However, the absolute reduction in fractures in clinical trials of these drugs were very small, between 2-4%.
What is the best medicine for osteoporosis?
It’s said to increase bone strength and reduce fractures in the hip, spine, wrist, arm, leg, and ribs. Another osteoporosis med, raloxifene ( Evista) works like estrogen in keeping up your bone mass.
How to prevent osteoporosis?
However, there is no proof that these foods help prevent or delay osteoporosis. Exercise. Make it a habit to do weight-bearing activities such as running, walking, tennis, dancing, stair climbing, aerobics, and weightlifting. When you do this regularly, this helps your bone density, so your bones are stronger.
How to get more calcium at home?
For instance, you can add nonfat dry milk to everyday foods and beverages, including soups, stews, and casseroles. Each cup of dry milk adds about a third of the calcium you need each day.
What is the best medicine to take before eating?
Ibandronate ( Boniva), which is a pill that you need to take at least an hour before you eat or take any other meds. Risedronate ( Actonel, Atelvia), which is a pill that you need to take at least half an hour before you eat or take any other meds.
How many doses of Prolia are there?
It is an antsclerostin antibody and works mainly by increasing new bone formation. A dose is given as two injections, one after another. It is limited to only 12 doses which must be administered by your doctor. There’s also a biologic drug -- denosumab ( Prolia, Xgeva) -- for osteoporosis.
Can you take calcium supplements at the same time?
They can check that it won’t make it harder for your body to use any other medicines you take. Your doctor can also tell you if you need to take calcium supplements at a different time than your other medications.
Can hormone replacement therapy be used to treat osteoporosis?
But doctors don’t prescribe hormone replacement therapy to only prevent osteoporosis, due to potential health risks. In women who have been on hormone replacement therapy in the past and then stopped it, their bones start to thin again, at the same pace as during menopause. WebMD Medical Reference. Sources.
What are some exercises to help with osteoporosis?
So is regular weight-bearing exercise, such as weight training, walking, hiking, jogging, climbing stairs, tennis, and dancing . If you have osteoporosis, avoid activities that involve twisting your spine or bending forward from the waist, such as conventional sit-ups, toe touches, or swinging a golf club.
How to contact the National Osteoporosis Foundation?
301-565-2966 (TTY ) [email protected]. www.niams.nih.gov. National Osteoporosis Foundation. 800-231-4222 (toll-free) [email protected]. www.nof.org. This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
What is a bone mineral density test?
A bone mineral density test compares your bone density to the bones of an average healthy young adult. The test result, known as a T-score, tells you how strong your bones are, whether you have osteoporosis or osteopenia, and your risk for having a fracture.
Why is osteoporosis considered a silent disease?
Osteoporosis is called a “silent disease” because you may not notice any changes until a bone breaks. All the while, though, your bones had been losing strength for many years. Bone is living tissue. To keep bones strong, your body breaks down old bone and replaces it with new bone tissue.
What happens to the bones in your 40s?
As people enter their 40s and 50s, more bone may be broken down than is replaced. A close look at the inside of bone shows something like a honeycomb. When you have osteoporosis, the spaces in this honeycomb grow larger, and the bone that forms the honeycomb gets smaller. The outer shell of your bones also gets thinner.
How do you know if you have osteoporosis?
For some people, the first sign of osteoporosis is to realize they are getting shorter or to break a bone easily. Don’t wait until that happens to see if you have osteoporosis. You can have a bone density test to find out how strong your bones are.
How to keep bones strong?
To keep bones strong, your body breaks down old bone and replaces it with new bone tissue. Sometime around age 30, bone mass stops increasing, and the goal for bone health is to keep as much bone as possible for as long as you can. As people enter their 40s and 50s, more bone may be broken down than is replaced.
How can osteoporosis be prevented?
Osteoporosis can be prevented. Exercise, especially lifting weights, helps to maintain healthy bone mass. Healthy lifestyle choices, such as not smoking or misusing substances, also decrease your risk for developing osteoporosis.
Can osteoporosis be treated with alternative medicine?
The goal of any alternative treatment is to manage or heal the condition without the use of medication. Some alternative therapies can be used for osteoporosis. While there’s little scientific or clinical evidence to suggest that they’re truly effective, many people report success. Always inform your doctor before beginning any alternative medicine ...
Does black cohosh help with bone loss?
It contains phytoestrogens (estrogen-like substances) that may help prevent bone loss. A 2008 study. Trusted Source. found that black cohosh promoted bone formation in mice. More scientific research is needed to determine if these results can be extended to treatment in humans with osteoporosis.
Can you lose bone mass with osteoporosis?
When a person is diagnosed with osteoporosis, they’re advised to change their diet to incorporate more calcium. Though bone mass can’t be instantly corrected, dietary changes may stop you from losing more bone mass. Hormone replacement drugs, particularly ones that contain estrogen, are often prescribed.
Can soy be used for osteoporosis?
Isoflavones are estrogen-like compounds that may help protect bones and stop bone loss. It’s generally recommended that you talk to your doctor before using soy for osteoporosis, especially if you have an increased risk of estrogen-dependent breast cancer .
Does red clover help with osteoporosis?
Red clover is thought to contain estrogen-like compounds. Since natural estrogen can help protect bone, some alternative care practitioners may recommend its use to treat osteoporosis. However, there’s no scientific evidence to show that red clover is effective in slowing down bone loss. The estrogen-like compounds in red clover may interfere ...

Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Preparing For Your Appointment
- Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of mineral in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only certain bones are checked — usually in the hip and spine.
Treatment
- Treatment recommendations are often based on an estimate of your risk of breaking a bone in the next 10 years using information such as the bone density test. If your risk isn't high, treatment might not include medication and might focus instead on modifying risk factors for bone loss and falls.
Purpose
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Medical uses
- These suggestions might help reduce your risk of developing osteoporosis or breaking bones: 1. Don't smoke.Smoking increases rates of bone loss and the chance of fracture. 2. Limit alcohol.Consuming more than two alcoholic drinks a day may decrease bone formation. Being under the influence of alcohol also can increase your risk of falling. 3. Prevent falls.Wear low-he…
Prevention
- Your doctor might suggest bone density testing. Screening for osteoporosis is recommended for all women over age 65. Some guidelines also recommend screening men by age 70, especially if they have health issues likely to cause osteoporosis. If you have a broken bone after a minor force injury, such as a simple fall, bone density testing may be important to assess your risk of more fr…
Risks
- Osteoporosis treatment has radically changed in a relatively short period. In the early 1990s, women had few treatment options. Now, there are many different types of treatments available. This has created a dilemma for women trying to decide which, if any, of these medications they need. Women want to know when it is appropriate to take a drug for osteoporosis, and which tre…
Overview
- Weve developed this fact sheet to help women understand what treatment options exist, what the side effects and risks are, what evidence supports their efficacy, and how to adopt non-drug approaches to preventing fracture. We hope this tool will help empower women to have conversations about osteoporosis with their providers, make informed decisions about whether …
Side effects
- Bisphosphonates are commonly prescribed for osteoporosis treatment and prevention. The FDA has approved many bisphosphonates to prevent bone loss and fractures in post-menopausal women: alendronate (brand name Fosamax), etidronate (brand name Didronel), ibandronate (brand name Boniva), risedronate (brand name Actonel), tiludronate (brand name Skelid), pamidr…
Benefits
- Although many clinicians and pharma-sponsored education campaigns conflate prevention and treatment, the NWHN thinks that it is important for people considering bisphosphonates to understand how the effectiveness differs based on individuals bone health. These drugs have been shown to reduce the risk of a hip fracture in women who have been diagnosed with osteop…
Selected publications
- There have been numerous reports of unusual fractures in the thighbones of otherwise healthy women that took an inordinately long time to heal. Other women experienced severe bone, joint, and/or muscle pain. The FDA advises patients with such pain to consider discontinuing the drug, which usually causes the pain to go away. The jaw tissue of some women taking bisphosphonat…
Resources
- Denosumab (brand name Prolia) is an osteoporosis medication that uses human monoclonal antibody. Approved in 2010, this drug works by targeting and inactivating osteoclasts to stop natural bone breakdown, or resorption, processes. Denosumab is given in a subcutaneous (just below the skin) injection twice a year. This treatment is intended for women with severe osteopo…
Clinical significance
- Denosumab has proven effective at building bone density and reducing spine and hip fractures. However, it carries a risk of serious side effects. Denosumabs cellular target in bone also exists in the immune system. This has led some women taking denosumab to experience serious infections requiring hospitalization (e.g. heart infections), making this a poor option for those wi…
Sources
- Exercise is another critical way to maintain healthy bones. Studies have shown that exerciseespecially weight bearing exercise regimens like walking, dancing, or runningleads to increased bone density. Tai Chi an ancient Chinese practice that combines slow, deliberate movements, breathing exercises, and meditation has been shown to be one of the most effectiv…