Hypothyroidism
A condition resulting from decreased production of thyroid hormones.
Hyperthyroidism
Over production of hormones by the thyroid gland located at the front of neck.
What are the dangers of not treating hypothyroidism?
Nov 15, 2001 · TSH or free T 4 levels are monitored annually in most patients with hypothyroidism, although no data support this practice. Generally, once a stable maintenance dosage of levothyroxine is achieved,...
What is the best test for hypothyroidism?
Dec 22, 2020 · Fetal ultrasound can be used to monitor for goiter (which can be associated with both fetal hyper- and hypothyroidism) and signs of fetal hyperthyroidism (42, 43). Patient’s disease course Unfortunately, the patient experienced a spontaneous pregnancy loss at about 9 weeks’ gestation.
How do doctors diagnose hypothyroidism?
Apr 03, 2012 · The symptoms of autoimmune hypothyroidism usually develop gradually and correcting them is also a slow process. For patients, this is often the most frustrating aspect of the disease! Your doctor will typically schedule follow-up TSH, T4 and T3 blood tests about two months after you start thyroid hormone replacement.
How to naturally cure hypothyroidism?
Dec 01, 2014 · Resolution of symptoms can be documented even with treatment of mild hypothyroidism , but few studies document longitudinal monitoring of both symptoms and biochemical parameters within individual treated patients. Symptoms, therefore, are probably best followed within a framework of biochemical parameters, particularly serum TSH.

How do you monitor levothyroxine therapy?
Results: The sensitive thyrotropin (TSH) test is the preferred method to monitor therapy because it agrees with physiologic measures of thyroid hormone effect.
What should I monitor with levothyroxine?
Response to thyroxine (levothyroxine sodium) is best monitored biochemically. Thyroid function should be assessed every 6-8 weeks until the patient is euthyroid and then rechecked annunally, aiming to maintain T4 and TSH within the normal range (1).
What happens after treatment for hypothyroidism?
You should start to feel better a few days after you begin taking medicine. But it may take a few months for your thyroid hormone levels to get back to normal. If your levels get better, but you still have symptoms like fatigue and weight gain, your doctor may need to change your treatment.Jan 27, 2022
What labs should be monitored with hypothyroidism?
Thyroid-stimulating hormone (TSH) level is the preferred test for initial evaluation of suspected primary hypothyroidism (strength of recommendation [SOR]: expert opinion). If TSH is abnormal, a free thyroxine (T4) level will further narrow the diagnosis.
Does TSH reliably detect hypothyroidism?
Results: Patients with symptoms consistent with hypothyroidism but with normal TSH values in the range of 1-4 IU/mL and normal free T4 (FT4) values by immunoassay measurements were confirmed to be biochemically hypothyroid following measurements of thyroid hormones by mass spectrometry.Feb 20, 2018
How often should TSH be monitored?
A TSH blood test should be obtained at least every 6-12 months while you are on a stable thyroxine dose, and more often if your dose is changed. Your doctor will usually wait 6-8 weeks after a thyroxine dose adjustment to measure your TSH, when the levels of thyroxine have reached a steady state.
How do you diagnose hypothyroidism?
The main way to diagnose hypothyroidism is a blood test called the thyroid stimulating hormone (TSH) test. Your healthcare provider may also order blood tests for conditions like Hashimoto's disease. If the thyroid is enlarged, your provider may be able to feel it during a physical exam during an appointment.Apr 19, 2020
What is the prognosis for hypothyroidism?
The prognosis of hypothyroidism is good with early treatment. However, once the disease has progressed to myxedema coma, the mortality rate may exceed 20% in the treated population. Relapses occur if treatment is discontinued. The mortality rate in myxedema coma has historically been as high as 80%.
What are early warning signs of thyroid problems?
7 Early Warning Signs of Thyroid IssuesFatigue.Weight gain.Weight loss.Slowed heart rate.Increased heart rate.Sensitivity to heat.Sensitivity to cold.Jan 11, 2021
When T3 and T4 are normal but TSH is high?
When the thyroid gland becomes inefficient such as in early hypothyroidism, the TSH becomes elevated even though the T4 and T3 may still be within the "normal" range.
Why T3 T4 TSH test is done?
A T3 test is most often used to diagnose hyperthyroidism, a condition in which the body makes too much thyroid hormone. T3 tests are frequently ordered with T4 and TSH (thyroid stimulating hormone) tests. A T3 test may also be used to monitor treatment for thyroid disease.Sep 13, 2021
What does the free T4 test show?
A free T 4 test is used to find out how well your thyroid gland is working. T 4 is 1 of 2 hormones produced by the thyroid, a butterfly-shaped gland in your neck. There are 2 forms of T 4. Some T 4 in your blood is bound to proteins, and some T 4 circulates freely, or unbound from proteins.
What is the best treatment for hypothyroidism?
Standard treatment for hypothyroidism involves daily use of the synthetic thyroid hormone levothyroxine (Levo-T, Synthroid, others). This oral medication restores adequate hormone levels, reversing the signs and symptoms of hypothyroidism. You'll likely start to feel better soon after you start treatment.
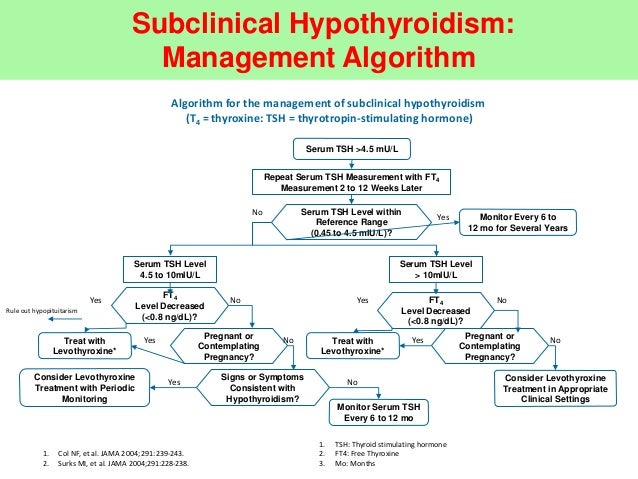
Why do you need a TSH test?
TSH tests also play an important role in managing hypothyroidism. They help your doctor determine the right dosage of medication, both initially and over time. In addition, TSH tests are used to help diagnose a condition called subclinical hypothyroidism, which usually causes no outward signs or symptoms.
What does a low TSH level mean?
A low level of thyroxine and high level of TSH indicate an underactive thyroid. That's because your pituitary produces more TSH in an effort to stimulate your thyroid gland ...
What are the side effects of a thyroid medication?
Excessive amounts of the hormone can cause side effects, such as: Increased appetite. Insomnia. Heart palpitations. Shakiness. If you have coronary artery disease or severe hypothyroidism, your doctor may start treatment with a smaller amount of medication and gradually increase the dosage.
Can you test for thyroid problems?
Diagnosis. In general, your doctor may test for an underactive thyroid if you are feeling increasingly tired, have dry skin, constipation and weight gain, or have had previous thyroid problems or a goiter.
Does levothyroxine help with weight gain?
The medication gradually lowers cholesterol levels elevated by the disease and may reverse any weight gain. Treatment with levothyroxine will likely be lifelong, but because the dosage you need may change, your doctor is likely to check your TSH level every year.
Does levothyroxine cause side effects?
Levothyroxine causes virtually no side effects when used in the appropriate dose and is relative ly inexp ensive. If you change brands, let your doctor know to ensure you're still receiving the right dosage.
What are the symptoms of hypothyroidism?
The signs and symptoms associated with hypothyroidism are well known and include, but are not limited to, dry skin, cold intolerance, constipation, slowed thinking, weight gain, coarse skin, puffiness, slowed heart rate, and delayed relaxation of ankle reflexes. The symptoms often have an insidious onset and overlap significantly between patients with thyroid disease and those without. Many signs and symptoms of thyroid dysfunction are neither sensitive nor specific ( 57 ). For example, signs and symptoms associated with hypothyroidism such as dry skin, fatigue, and constipation may not reveal themselves with modest degrees of hypothyroidism and could have other causes. Several studies report a correlation between signs and symptoms of hypothyroidism and biochemical disease either based on an increasing cumulative number of symptoms ( 57) or on an abnormal clinical score ( 58 ). Unfortunately, while several signs or symptoms show relatively high specificity, such as puffiness and slowed movements, the sensitivity is relatively low. Physiological, psychological, and biochemical biomarkers of thyroid status, in addition to thyroid hormone levels, are available. Physiological parameters include heart rate, pulse wave arrival time ( 59, 60 ), echocardiographic parameters of left ventricular function, Achilles reflex time ( 58 ), voice fundamental frequency, and basal metabolic rate ( 61–63 ). To illustrate the lack of specificity, basal metabolic rate, although profoundly affected by extreme hypothyroidism, is also affected by other conditions such as fever, malignancy, and nutritional status ( 64, 65 ). Pulse wave arrival time can also be affected by atherosclerosis and systemic sclerosis. Achilles reflex time seems to have a reasonable sensitivity of 77% and a good specificity of 93% to confirm or exclude hypothyroidism ( 58 ), but it is limited by the fact that a small percentage of euthyroid individuals have an abnormal reflex time. Other clinical indices used to assess thyroid function include psychiatric and neuropsychological measures. Various rating scales have been used to assess the degree of hypothyroidism ( 57, 58, 66–68 ). However, such clinical scores may not be sufficiently sensitive to signal subtle changes in thyroid status ( 69 ).
What is the TSH range for thyroid disease?
The TSH range for each trimester should be defined within the medical system in which care is being provided, with a generalized range as follows: 0.1–2.5 mIU/L for the first trimester, 0.2–3.0 mIU/L for the second trimester, and 0.3–3.0 mIU/L for the third trimester, as outlined in the ATA guidelines for the management of thyroid disease during pregnancy ( 1 ). Several studies, including the Generation R study by Medici et al. ( 262 ), have reported a higher TSH reference range during pregnancy, suggesting that ethnicity-based polymorphisms and dietary factors may play an important role in the thyroid axis response to pregnancy ( 262–266 ). The use of FT 4 immunoassays to further define the thyroid status during pregnancy is complicated by interferences associated with physiological changes during pregnancy. These changes include increases in TBG and nonesterified fatty acids, as well as lower concentrations of albumin. Liquid chromatography–tandem mass spectrometry (LC/MS/MS) assays eliminate some of these confounding factors ( 267 ). However, these assays are time consuming and more expensive. The increasing availability of LC/MS/MS assays may increase their acceptance and decrease their cost. LC/MS/MS appears to be associated with improved accuracy and reliability of FT 4 measurements ( 268) and is the method endorsed by the ATA guidelines for the diagnosis and management of thyroid disease during pregnancy ( 1 ).
What is factitious thyrotoxicosis?
Factitious thyrotoxicosis (thyrotoxicosis factitia) has traditionally been defined as a syndrome wherein patients surreptitiously ingest TH ( 452 ). It can be associated with Münchausen's syndrome (in which physical symptoms and signs of illness are intentionally produced) and is also associated with neuroses related to poor body image and concerns about increased body weight. More recently, the term factitious thyrotoxicosis has been expanded ( 453) to include instances of accidental LT 4 ingestion, such as in pediatric poisoning or pharmacy error, or through intentional or unintentional ingestion of supplements that contain thyroid gland extract ( 454 ). The treatment is the discontinuation of TH. In individuals with psychiatric disorders who are secretly taking TH, psychiatric consultation is warranted. Such a consult may not only provide relief for the underlying disorder, but also serves to protect the patient from thyrotoxic-related events. Factitious thyrotoxicosis has not been studied in a systematic manner. A strong recommendation is made despite low-quality evidence because there are benefits, but few risks.
What is the main molecule secreted by the thyroid gland?
The thyroid gland secretes a variety of iodinated and noniodinated molecules that collectively play important roles during prenatal and adult lives. Understanding what these molecules are and what they do informs our understanding of the therapy for hypothyroidism. The main noniodinated molecule secreted by the thyroid is calcitonin, an endogenous hormone with probable effects on calcium and bone metabolism. The other iodine-containing molecules include T 4, T 3, rT 3, 3,3′-diiodothyronine, 3,5-diiodothyronine (3,5-T 2 ), monoiodothyronine, and their decarboxylated forms known as thyronamines.
What is desiccated thyroid?
Desiccated thyroid or thyroid extract refers to preparations that are derived from the thyroid gland of animals. These preparations were the primary therapy for hypothyroidism until the advent of synthetic T 4 preparations in the 1960s. All commercially available prescription desiccated preparations are derived from pigs. As per the United States Pharmacopeia (USP), desiccated thyroid is “the cleaned, dried, and powdered thyroid gland previously deprived of connective tissue and fat. It is obtained from domesticated animals that are used for food by humans.” Tablets are measured for T 4 and T 3 content and are formulated into doses expressed as “grains” with 1 grain (65 mg) tablets containing 38 μg of T 4; 9 μg of T 3; protein-bound iodine; and unmeasured quantities of diiodothyronine, monoiodothyronine, and calcitonin, to which inactive ingredients are added for tablet stability. Varying strengths from fractions to multiples of a grain are commercially available. One process used to achieve specific dosage strengths is to mix different batches of the product during manufacture. The bioavailability of the T 4 and T 3 components has been shown to be the same between desiccated thyroid and synthetic preparations ( 473 ).
What is NTIS in patients?
As patients with normal thyroid function become critically ill, a progressive decline in circulating T 3 is observed, followed by decreases in serum T 4 and TSH if the clinical course does not improve. This stereotypic pattern, known as NTIS or alternatively “euthyroid-sick syndrome,” occurs without regard to the etiology of the primary illness, suggesting a physiologic, adaptive role. At the same time, since untreated hypothyroidism can itself lead to critical illness in the form of myxedema coma, debate continues as to whether NTIS patients might benefit from TH replacement.
What is LT 4?
An oral gel preparation that contains only LT 4, glycerin, gelatin, and water has been developed. The gelatin capsule contains LT 4 as a liquid ( 109 ). This formulation is in contrast to standard solid LT 4 tablets that contain excipients and dyes. Pabla et al. ( 110) studied in vitro dissolution of gel capsules and noted rapid and efficient dissolution at low pH concentrations. Colucci et al. ( 111) observed that gel capsules met the revised FDA potency guidelines of 95%–105% ( 103, 104) and also met equivalence criteria. At present, there are no prospective, randomized clinical trials in hypothyroid individuals comparing gel capsules to other commercial LT 4 preparations in terms of the serum FT 4, T 3, and TSH concentrations achieved during chronic therapy.
What happens if you have low thyroid?
Low thyroid hormone production can leave your muscles weak, achy or stiff. Dry skin. Low thyroid hormone levels directly affect the skin. This can cause a variety of changes, including dryness, thickening, and scaling. Heartburn. Hypothyroidism slows digestion.
What is the function of the thyroid gland?
As part of the endocrine system, the thyroid gland helps to regulate the body’s metabolism in the form of blood pressure, blood temperature, and heart rate.
What is a goiter?
Goiter. A goiter is an abnormally enlarged thyroid gland that can happen in people with diseases like Hashimoto thyroiditis. Peripheral neuropathy. hypothyroidism that isn't treated can interfere with how the nerves send signals to and from your brain, spinal cord, and body. Thinning hair.
What causes hair loss?
The effects of hypothyroidism can cause you to lose hair on your scalp, face and body. Brain Fog. Hypothyroidism can affect your memory and your ability to think clearly. This mental fuzziness is sometimes called "brain fog". Weakness. Low thyroid hormone production can leave your muscles weak, achy or stiff. Dry skin.
Does hypothyroidism cause heart attacks?
Gallstones. Hypothyroidism may increase your risk of gallstones, hard pieces made up of substances like cholesterol or bile that form in your gallbladder. Heart attack risk. Hypothyroidism may increase cholesterol levels and narrow arteries. This could contribute to an increased risk of heart attack. Goiter.
Why does my belly feel bloated?
A lack of thyroid hormone slows the movement of food through your digestive tract, which can leave your belly bloated. Slow Metabolism. Too little thyroid hormone sows the body's metabolism, which can lead to weight gain. High blood pressure.
Where does NDT come from?
Natural Desiccated Thyroid (NDT) is derived from the dried (desiccated) thyroid glands of pigs or cow and provides T3, T4, and other thyroid hormones found in the human thyroid gland.
How to diagnose hypothyroidism?
Diagnosis of Hypothyroid. Your consultant usually will diagnose hypothyroidism by a thorough physical examination followed by a blood test. A medical history will probably be taken as well. The most common blood test used is the TSH test.
What blood test is used to diagnose hypothyroidism?
Additional blood tests used to confirm the diagnosis or determine the cause of hypothyroidism are the free T3 & free T4 test and the thyroid auto-antibody test. For all of the aforementioned tests a 12 hours fasting blood sample is required.
What causes hypothyroidism?
Causes of Hypothyroid. 1.Hashimoto’s thyroiditis -In this thyroid gland is usually enlarged and has a decreased ability to make thyroid hormones. It is an autoimmune disease in which the body’s immune system inappropriately attacks the thyroid tissue.
What medications can cause hypothyroidism?
6.Medications -Medicines that are used to an overactive thyroid may cause hypothyroidism. These include Methimazole, Propylthiouracil etc. 7.Severe iodine deficiency -In areas of world where there is an iodine deficiency in the diet severe hypothyroidism can be seen.
What causes a decrease in T4 and T3?
4.Pituitary or hypothalamic disease -If for some reason the pituitary gland or hypothalamus are unable to signal the thyroid and instruct it to produce thyroid hormones, a decreased level of circulating T4 and T3 may result, even if the thyroid gland itself is normal.
Does homeopathy help with thyroid?
Specially formulated Homeopathy medicines for thyroid, available exclusively at Welling Clinics can be very effective to cure hypothyroid and reverse the effects of low thyroid hormones like obesity, PCOS, hair fall & infertility. For more details of diet and tailor-made dietary advise for you, ask your specialist at Welling Clinic.
Can you use homeopathic medicine for hypothyroidism?
The Homeopathic medicines for Hypothyroid have to be specific to every individual person . That is the reason a detailed history is required to customise the treatment for Hypothyroid. The Homeopathic treatment for under active thyroid is chalked out after a detailed analysis and review of your past treatments for psoriasis ...

Diagnosis
Treatment
- Standard treatment for hypothyroidism involves daily use of the synthetic thyroid hormone levothyroxine (Levo-T, Synthroid, others). This oral medication restores adequate hormone levels, reversing the signs and symptoms of hypothyroidism. You'll likely start to feel better soon after you start treatment. The medication gradually lowers cholesterol...
Alternative Medicine
Preparing For Your Appointment