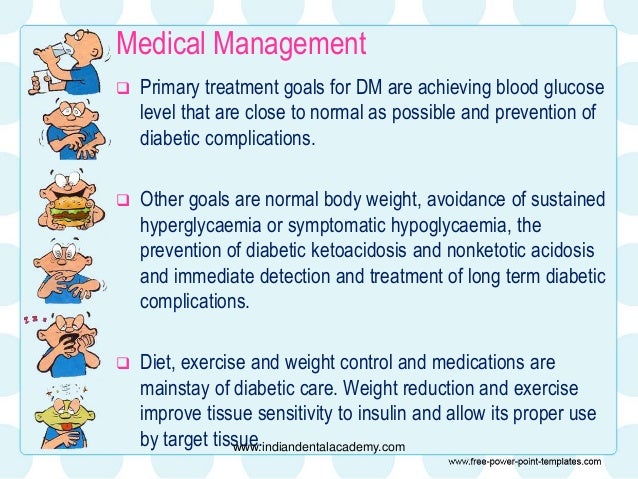
Diabetes Mellitus Treatments The goal of diabetes management is to keep blood glucose levels as close to normal as safely possible. Since diabetes may greatly increase risk for heart disease and peripheral artery disease, measures to control blood pressure and cholesterol levels are an essential part of diabetes treatment as well.
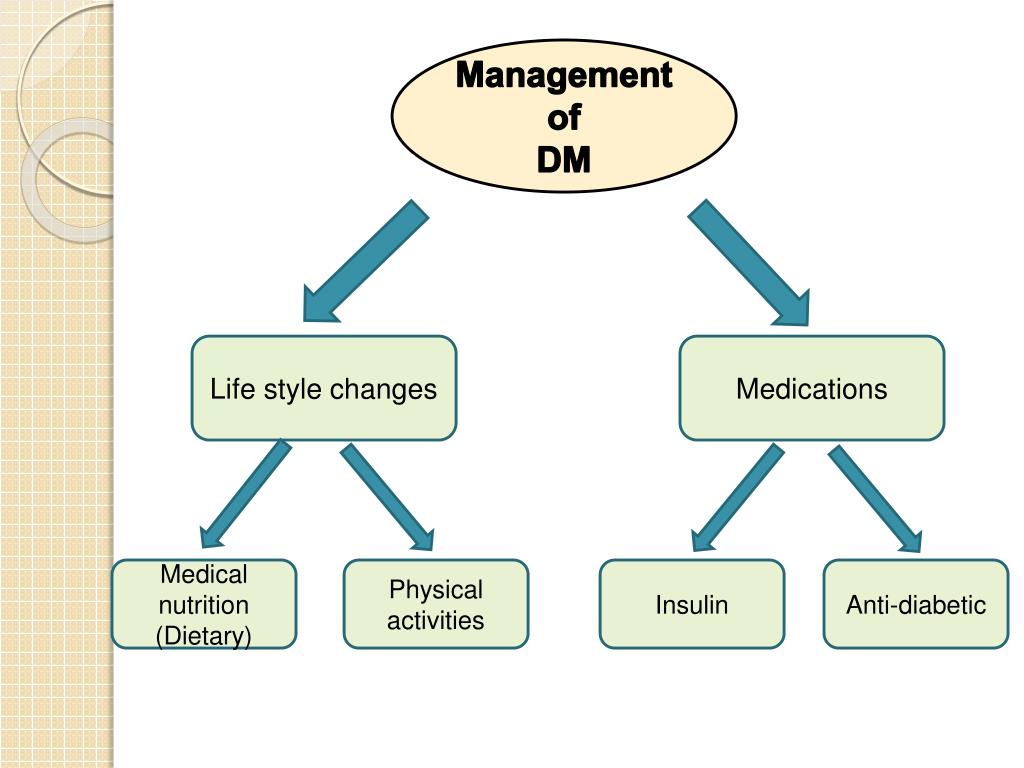
How is diabetes mellitus (DM) treated?
The general goals of the treatment of diabetes are to avoid acute decompensation, prevent or delay the appearance of late disease complications, …
What is the goal of diabetes management?
Goals of Treatment To keep the blood sugar as normal as possible without serious high or low blood sugars To prevent tissue damage caused by too much sugar in the blood stream
What is the therapeutic focus in patients with diabetes mellitus (DM)?
Treatment Goals in Diabetes Abstract The quality of glycaemic control in diabetes mellitus relies on accurate individualization of available treatment options. Treatment targets depend on the type and duration of diabetes, the patients' abilities and characteristics and the individual risk for acute and/or late-stage complications.
What is diabetes mellitus (DM)?
In patients diagnosed with diabetes mellitus (DM), the therapeutic focus is on preventing complications caused by hyperglycemia. In the United States, 57.9% of patients with diabetes have 1 or more diabetes-related complications and 14.3% have 3 or more. 1 Strict control of glycemia within the established recommended values is the primary method for reducing the …

What is the goal of type 2 diabetes treatment?
The main goals of treatment in type 2 diabetes are to keep your blood sugar levels within your goal range and treat other medical conditions that go along with diabetes (like high blood pressure); it is also very important to stop smoking if you smoke. These measures will reduce your risk of complications.Oct 28, 2020
What is the goal for blood sugar levels?
The American Diabetes Association (ADA) generally recommends the following target blood sugar levels: Between 80 and 130 milligrams per deciliter (mg/dL) or 4.4 to 7.2 millimoles per liter (mmol/L) before meals. Less than 180 mg/dL (10.0 mmol/L) two hours after meals.
What are the goals of diabetes treatment?
Goals Of Diabetes Treatment. To keep the blood sugar as normal as possible without serious high or low blood sugars. To prevent tissue damage caused by too much sugar in the blood stream.
What is the goal of insulin replacement therapy?
The goal is to replace the insulin in the right amount and at the right time. Sometimes, more insulin than needed is taken and this will cause hypoglycemia.
What is the ultimate goal for Type 1 diabetes?
What are the blood sugar (glucose) targets for diabetes? The ultimate treatment goal for Type 1 diabetes is to re-create normal (non-diabetic) or NEARLY normal blood sugar levels – without causing low blood sugars. Good blood sugar control requires that you know and understand a few general numbers.
What is the therapeutic focus of diabetes mellitus?
In patients diagnosed with diabetes mellitus (DM), the therapeutic focus is on preventing complications caused by hyperglycemia. In the United States, 57.9% of patients with diabetes have 1 or more diabetes-related complications and 14.3% have 3 or more. 1 Strict control of glycemia within the established recommended values is the primary method for reducing the development and progression of many complications associated with microvascular effects of diabetes (eg, retinopathy, nephropathy, and neuropathy). Aggressive treatment of dyslipidemia and hypertension focuses on decreasing the cardiovascular complications associated with macrovascular effects. The positive outcomes from adequate glycemic control on microvascular and macrovascular complications have been established in large well-controlled trials. 2-5 See the chapter on diabetes: Macro- and microvascular effects.
Why is glycemic control important?
Glycemic control is crucial for preventing microvascular and macrovascular complications of diabetes. Type 2 DM is a progressive disease and requires therapy intensification with time. Insulin sensitizers and incretin-based therapy should be used early in the course of type 2 DM.
What is SMBG used for?
Use of SMBG is an effective method to evaluate short-term glycemic control by providing real-time measure of blood glucose. It helps patients and physicians assess the effects of food, medications, stress, and activity on blood glucose levels and make appropriate adjustments.
What is the best way to reduce glycemic load?
Insulin sensiti zers reduce glycemic load primarily by improving insulin actions in peripheral tissues. Two classes of these oral hypoglycemic drugs are available: biguanides and thiazolidinediones. They have been shown in clinical use to have positive, durable effects in the treatment of diabetes.
How often is liglutide given?
It is administered once a day as a subcutaneous injection from its pen device. Timing is independent of meals. Half-life is about 13 hours. Its beneficial effects and side effects are similar to those of exenatide, but it may be slightly more powerful in its actions.
Do patients with type 1 diabetes need insulin?
Patients with type 1 DM require insulin therapy; some patients with advanced type 2 DM also require insulin. Multiple daily doses of insulin providing basal, prandial, and supplemental insulin are the mainstay of insulin therapy. Back to Top.
What is the goal of diabetes management?
Treatments. The goal of diabetes management is to keep blood glucose levels as close to normal as safely possible. Since diabetes may greatly increase risk for heart disease and peripheral artery disease, measures to control blood pressure and cholesterol levels are an essential part of diabetes treatment as well.
What is the responsibility of a diabetic?
This includes monitoring blood glucose levels, dietary management, maintaining physical activity, keeping weight and stress under control, monitoring oral medications and, if required, insulin use via injections or pump.
How do oral diabetes medications work?
These include improve the effectiveness of the body's natural insulin, reduce blood sugar production, increase insulin production and inhibit blood sugar absorption. Oral diabetes medications are sometimes taken in combination with insulin.
How to reduce blood sugar levels at UCSF?
Dietary Management and Physical Activity. Modifying eating habits and increasing physical activity are typically the first steps toward reducing blood sugar levels. At UCSF Medical Center, all patients work with their doctor and certified dietician to develop a dietary plan.
What is insulin pump?
Using an insulin pump is an alternative to injections. The pump is about the size of a pager and is usually worn on your belt. Insulin is delivered through a small tube (catheter) that is placed under the skin (usually in the abdomen). There are four major types of insulin: Rapid-acting. Short-acting.
β-CELL DYSFUNCTION AND TYPE 2 DIABETES: IN VIVO STUDIES
Several cross-sectional and prospective studies showed that β-cell dysfunction plays a major role in determining the onset and progression of type 2 diabetes.
β-CELL DYSFUNCTION AND TYPE 2 DIABETES: HISTOLOGICAL AND EX VIVO STUDIES
The role of reduced β-cell mass in human type 2 diabetes, the primary importance of β-cell apoptosis, and the insufficiency of replication/neogenesis have been studied by several authors using histological pancreatic samples, or isolated islets.
β-CELL PRESERVATION BY CURRENT PHARMACOLOGICAL THERAPIES: IN VIVO STUDIES
As aforementioned, research performed in different categories of subjects by cross-sectional and longitudinal studies, together with histological analysis and ex vivo islet investigations, strongly suggest that β-cell failure is crucial for the onset of diabetes and progressive deterioration of glycemic control.
β-CELL PRESERVATION BY CURRENT PHARMACOLOGICAL THERAPIES: EX VIVO STUDIES
The possibility that pancreatic β-cell damage can be prevented, or even reverted, has been tested in isolated human nondiabetic islets exposed to different metabolic perturbations and, more importantly, with islets from type 2 diabetic donors. In early work, it was assessed whether metformin could affect the phenomenon of glucotoxicity ( 39 ).
CONCLUSIONS
Pancreatic β-cell dysfunction is key to the development and progression of type 2 diabetes. Both altered β-cell function and decreased β-cell mass are likely to contribute to the defects in insulin release typical of diabetes. These defects cause a progressive increase of glucose levels, with deterioration of glycemic control over the years.
Acknowledgments
This work was supported in part by the Italian Ministry of University and Research (PRIN 2007–2008).