Is it a sin to refuse medical treatment?
Someone who enters a hospital voluntarily and shows no imminent risk of danger to self or others may express the right to refuse treatment by stating he or she wants to leave the hospital. But a person admitted involuntarily, due to danger to …
Does a doctor have the right to refuse a patient treatment?
Although the right to refuse medical treatment is universally recognized as a fundamental principle of liberty, this right is not always honored. A refusal can be thwarted either because a patient is unable to competently communicate or because providers insist …
Is it legal for a doctor to reject a patient?
Mar 08, 2021 · Quill (1997), the U.S. Supreme Court affirmed a common law right to preserve individual autonomy, the right to refuse treatment, and the right to be free from unwanted touching. The basic principle...
Can doctors legally refuse to treat patients?
Case Scenario. An ambulance is called for a 72-year-old male who’s having chest pain. The calling party states her father called her because he wasn’t feeling well–she’s not on scene.

Does a patient have the right to refuse treatment?
What constitutes the right to refuse treatments?
What is it called when a patient refuses treatment?
What are the rules for refusing to treat the patient?
What does the Constitution say about refusing medical treatment?
On what grounds can a doctor refuse to treat a patient?
Under the Civil Rights Act of 1964, it is illegal for a healthcare provider to deny a patient treatment based on the patient's age, sex, race, sexual orientation, religion, or national origin.May 9, 2017
What are the 7 rights of a patient?
- The Right to Be Treated with Respect.
- The Right to Obtain Your Medical Records.
- The Right to Privacy of Your Medical Records.
- The Right to Make a Treatment Choice.
- The Right to Informed Consent.
- The Right to Refuse Treatment.
What should a nurse do when a patient refuses treatment?
Can a doctor stop treating a patient?
What is in the Hippocratic oath?
What is the right to treatment law?
Laws compelling a right-to-treatment law developed and became instrumental to the quality-controlled public psychiatric hospitals that exist today. In fact, in order for public psychiatric hospitals to receive Medicare and Medicaid ( and other third-party) payment , they must obtain the same national certification as academic medical centers and local community hospitals. For patients and families, this means that a person admitted to a public psychiatric hospital has a right to receive—and should receive—the standard of care delivered in any accredited psychiatric setting.
What does it mean to be admitted to a public psychiatric hospital?
For patients and families, this means that a person admitted to a public psychiatric hospital has a right to receive—and should receive—the standard of care delivered in any accredited psychiatric setting.
What is involuntary treatment?
For involuntary treatment (treatment without consent ) to be delivered outside of an acute emergency, the doctor and hospital must petition a court to order it. Laws vary from state to state and, of course, no two judges are alike. Generally, judges rule in favor of well-prepared doctors and hospitals that show that.
How long does an inpatient stay in a hospital?
Inpatient stays often last several weeks (or months) longer if court-ordered treatment is required. Notably, as clinicians have seen, once a court order is obtained, almost all patients comply with treatment within a day or so, and then, hopefully, proceed to respond to treatment.
Do patients have the right to refuse treatment?
All patients have both a right to treatment and a right to refuse treatment. These rights sometimes become the centerpiece of debate and dispute for people who are hospitalized with an acute psychiatric illness.
Can insurance refuse to pay for treatment?
Unfortunately, the right to refuse treatment can, and does, result in some patients being locked up in a hospital where doctors then cannot proceed with treatment. What’s worse, and deeply ironic, is that insurance companies may refuse to pay, stating there is “no active treatment.”.
Do psychiatric hospitals have insurance?
This state of financial affairs, by and large, does not happen in state psychiatric hospitals, which represent the true safety net of services for people with serious and persistent mental illnesses, because these hospitals are not wholly dependent on insurance payment and cannot refuse to treat someone who cannot pay.
When can a patient's right to refuse medical treatment be overridden?
The right to refuse medical treatment can only be overridden when a patient is deemed by a court to be lacking in decisional capacity.
What happens if you don't consent to treatment?
Part of that pressure may be the belief that if they do not consent, they may experience adverse consequences, such as blocked access to needed care in the future.
Why are the patient and spouse surprised when they open the door?
The patient and spouse are surprised because they are under quarantine and are not expecting anyone. They open the door. An individual identifies themself as a nurse from the hospital that provided the IV treatment and states they are there to hospitalize the patient.
What are the criteria for decision making in mental health?
Noted mental health ethicists suggest four core criteria for decisional competence: the ability to communicate a choice; understand the relevant information; appreciate the situation and its consequences; and reason about treatment options (Appelbaum, 2007; Berg, Appelbaum & Grisso, 1996).
What is the importance of autonomy in medical care?
It endorses a commitment to an individual’s rights to choose. The right to accept or reject what (if any) medical interventions falls along with other core rights, such as where to live, whom to marry, and how to worship. This right to choose or decline medical treatment can only be overridden if there is evidence that an individual lacks decisional capacity.
Why do patients capitulate to medical advice?
Some patients, despite decisional competence, may capitulate to a medical professional’s advice. This may occur because they are, as in our case example, in a vulnerable position. For example, a patient may be suffering from a condition that is potentially lethal and taking experimental treatment.
What does the nurse say about the patient's fears and distress about being in a hospital?
The nurse insists on the hospitalization and dismisses the patient’s fears and distress about being in a hospital as “silly.”. The nurse intimates that the patient’s IV procedure was approved only if they agreed to the staff’s recommendations. The patient again declines hospitalization.
How to make informed refusal?
The first step in the process of informed refusal is to establish if the patient is their own medical decision-maker. This relates to competence. Competence is a legal definition and is determined by a judge. Individuals with guardians have been deemed by the court unable to represent themselves and thus have a surrogate decision-maker. This could be the case with adults with dementia or other cognitive impairment, and minors. This may also apply to those in law enforcement custody. In these cases, the wishes of the guardian should be followed. If the guardian is unable to be contacted, the patient should be transported. The patient should go to an appropriate medical facility where a screening exam can be performed to determine if an emergency medical condition exists. Special attention must be paid to legal exceptions that allow minors to make healthcare decisions. In certain cases, like suspected abuse, transport should be pursued despite the objection of guardians.
What is informed consent?
Informed consent is an ethical and legal concept that relates to medical decision-making. It’s a generally accepted duty of the care provider, and right of the patient, to obtain informed consent. It can be defined as the process by which the care provider seeks the affirmative allowance of the patient to provide healthcare after apprising the patient of the benefits and risks of the proposed treatment. In this way, the provider respects the autonomy of the patient and their right to determine what happens to them in accordance with their personal values, health beliefs and goals. Ridley describes the concept, “Maximization of respect for patient autonomy and bodily integrity–rather than the imposition of the doctor’s professional values–is what application of the doctrine of informed consent should endeavor to achieve.” 1
Can a patient refuse to be informed?
For instance, it’s advocated by some that since informed decision-making is a two-part patient right, one or both parts can be waived by the patient at their prerogative.1 Accordingly, the patient may refuse to be informed about their medical condition and make a decision.
Can a patient who is not alert and oriented have capacity?
Capacity goes beyond just being alert and oriented. However, a patient who isn’t alert and oriented can’t have capacity. Nor can a patient who is psychotic, suicidal, or homicidal have capacity. Capacity can be altered by a medical condition.
Is there variation in the patient care guidelines?
Consequently, there’s great variation in the patient care guidelines by which they abide. It’s of the utmost importance providers understand these laws and treatment guidelines as they apply to their service area.
Can a guardian be transported if unable to be contacted?
In these cases, the wishes of the guardian should be followed. If the guardian is unable to be contacted, the patient should be transported .
Is it reasonable to ask law enforcement to assist in determining sobriety if providers are unsure
Given their specialty equipment and training, it’s reasonable to ask law enforcement to assist in determining sobriety if providers are unsure on scene. In these instances, Lu and Adams state, “If providers believe in their medical judgment that the patient in question lacks decision-making capacity (as opposed to competence, which is a legal judgment), actions should be undertaken to ensure the patient’s best interest.” 5 As noted above, a patient’s lack of insight into their medical condition can show a lack of capacity.
Which amendment states that no person can be held to answer for a capital crime?
Fifth Amendment: No person shall be held to answer for a capital, or otherwise infamous crime, unless on a presentment or indictment of a Grand Jury, except in cases arising in the land or naval forces, or in the Militia, when in actual service in time of War or public danger; nor shall any person be subject for the same offence to be twice put in ...
What is the right of a state to guard against abuses?
A State is entitled to guard against potential abuses that can occur if family members do not protect a patient’s best interests, and may properly decline to make judgments about the ‘quality’ of life that a particular individual may enjoy, and [instead] simply assert an unqualified interest in the preservation of human life to be weighed against the constitutionally protected interests of the individual. 497 U.S. at 281–82.
What is the right to die?
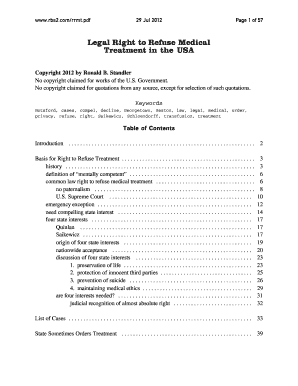
Although the popular term right to die has been used to describe the debate over end-of-life decisions, the underlying issues include a variety of legal concepts, some distinct and some overlapping. For instance, right to die could include issues of suicide, passive euthanasia (allowing a person to die by refusal or withdrawal ...
Is a state required to follow the judgment of the family, the guardian, or anyone but the patient
Despite the existence of a presumed due process right, the Court held that a state is not required to follow the judgment of the family, the guardian, or anyone but the patient herself in making this decision. 5. 497 U.S. at 286.
Is refusing nutrition and hydration the same as refusing other forms of medical treatment?
First, the Court appears, without extensive analysis, to have adopted the position that refusing nutrition and hydration is the same as refusing other forms of medical treatment . Also, the Court seems ready to extend such right not only to terminally ill patients, but also to severely incapacitated patients whose condition has stabilized.
When did the right to refuse treatment start?
Historically, the ability to force treatment on unwilling patients derived from a need-for-treatment justification. This approach started to change in the 1960s when there was a gradual move toward the "dangerous patient" justification-unwanted treatment could be imposed only if or when the patient presented a significant risk of harming himself or others. Under this new system, patient advocates began to press for the patient's right to determine what was done to his own body, creating instances in which the committed patient could decline treatment with medication. As these matters began to make legal appearances around the country, virtually every involved court recognized some substantial patient interest in a right to refuse treatment. 1
What are the issues that can be viewed as treatment refusal?
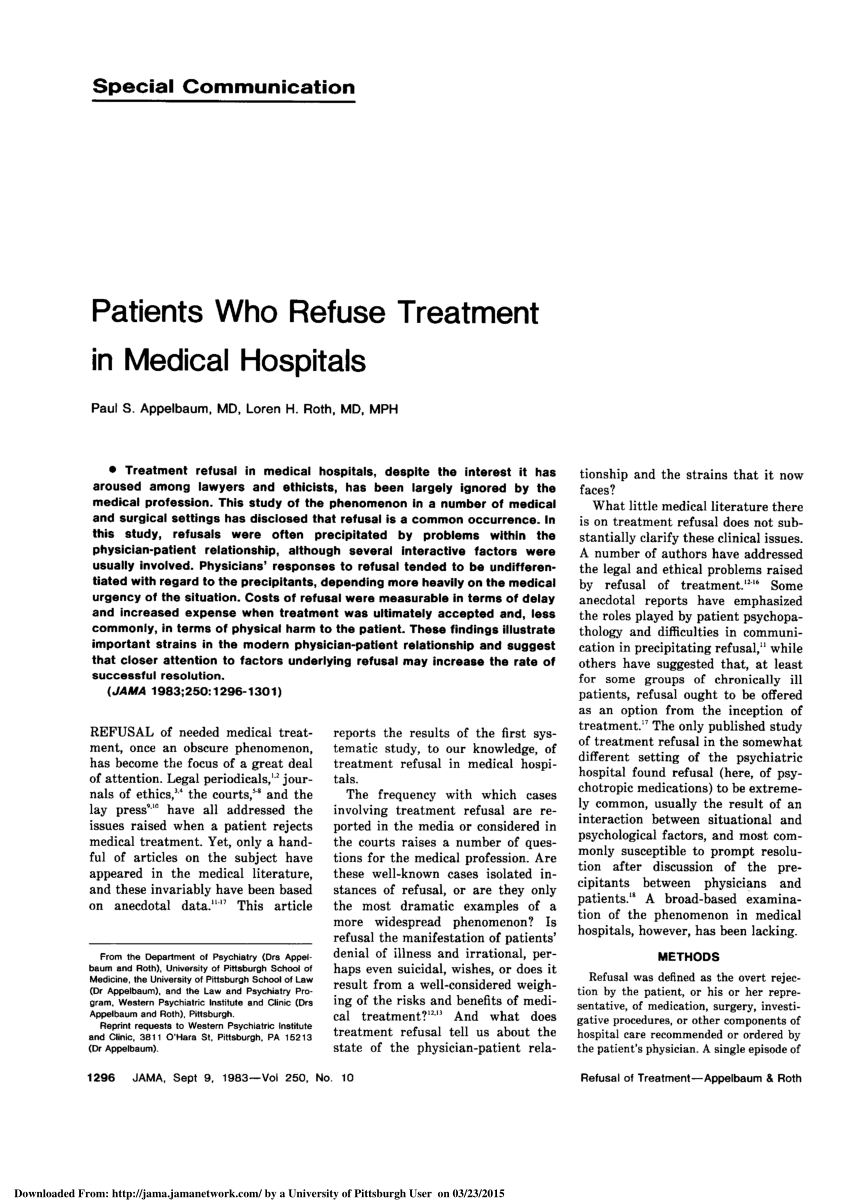
Most authors agree that treatment refusal should first be viewed as a clinical matter and an opportunity to revisit potential issues such as transference, conflicts with staff, power struggles, secondary gain surrounding the sick role, and denial of mental illness.
Which court recognized that there is a general right in all persons competent and incompetent to refuse medical treatment in
The Supreme Judicial Court of Massachusetts recognized that there "exists a general right in all persons, competent and incompetent, to refuse medical treatment in appropriate circumstances.".
Can a guardian be a substitute decision maker?
In some localities, a finding of incompetency can and will be accompanied by the appointment of a guardian who can then serve as a substitute decision maker. Some states will recognize living wills, durable power of attorney, or health care proxies as viable avenues to involuntary treatment of the incompetent patient.
Can a patient refuse treatment?
Clinicians need to be aware that despite a solid common-law and statutory foundation backing a patient's right to refuse treatment, there remains a legal (and clinical) expectation that involuntary treatment should be aggressively sought when appropriate, and liability can result from the failure to do so.
When treatment over a patient's objection would be appropriate?
KP: A simple example of when treatment over a patient’s objection would be appropriate is if a psychotic patient who had a life-threatening, easily treatable infection was refusing antibiotics for irrational reasons. Treatment would save the patient’s life without posing significant risk to the patient.
What are the first few questions in a treatment plan?
The first few questions consider the imminence and severity of the harm expected to occur by doing nothing as well as the risks, benefits, and likelihood of a successful outcome with the proposed intervention. Other questions consider the psychosocial aspects of this decision—how will the patient feel about being coerced into treatment? What is the patient’s reason for refusing treatment? The last question concerns the logistics of treating over objection: Will the patient be able to comply with treatment, such as taking multiple medications on a daily basis or undergoing frequent kidney dialysis?
Is there anything out there to help health care professionals approach the problem of delivering medical treatment against the wishes of patients
And there are fairly clear policies and laws concerning the ethics and legality of delivering psychiatric care to patients who refuse it. But there is nothing out there to help health care professionals approach the problem of delivering medical treatment against the wishes of patients who lack decisional capacity.
Can you force dialysis on a patient who resists?
As Dr. Rubin stated, one cannot force three times weekly dialysis sessions on a resistant patient even if it means that the patient will die without the treatment.
Who must refuse medical treatment?
For one, the person refusing to provide medical treatment to the patient must be someone who is employed by the hospital. In addition, that person must also possess the authority to decide which patients can or cannot receive treatment. In most cases, this generally will include any hospital staff that is in charge of the treatment and care ...
Why would a hospital refuse to admit a patient?
In contrast, if a patient’s conditions do not fall under the protections offered by EMTALA, then the hospital may refuse to admit or treat the patient simply because they are uninsured. A hospital is a business after all, which means they will sometimes have to make tough decisions in order to protect themselves from liability.
What happens if a doctor refuses to admit a patient?
On the other hand, if a doctor refuses to admit or treat a patient without ever considering the patient’s current medical condition, then some courts will find that the hospital should be held liable for refusing to admit or treat the patient.
What is an example of a hospital being held liable for refusing treatment?
For instance, if a patient arrives in critical condition and failing to treat them will result in severe injuries or possibly death, then the hospital will be held responsible for turning away a patient who needs immediate medical attention.
What happens if a patient arrives in critical condition and fails to treat them?
For instance, if a patient arrives in critical condition and failing to treat them will result in severe injuries or possibly death, then the hospital will be held responsible for turning away a patient who needs immediate medical attention.
What does it mean when a hospital is short on resources?
If the hospital is short on resources (e.g., not enough beds, staff, medicine, overcrowded, etc.); When the hospital believes that the patient would receive better treatment at a different facility; and/or. If the hospital lacks the appropriate equipment or type of medical personnel required to properly treat a patient’s injury or illness.
What to do if you are denied admission to a hospital?
If you have suffered further injuries or illness due to being denied admittance or treatment by a hospital, then you should consider contacting a local personal injury lawyer for advice. Your attorney will be able to determine whether you have a viable claim, and if so, they can walk you through the process of recovering any damages you might be owed for the harm done to you.