Treatment
- Surgery. Lung cancer surgery offers the best chance for a cure when LCLC is caught in the early stages. ...
- Chemotherapy. Chemotherapy may be used on its own or along with surgery. ...
- Targeted Therapies. Targeted therapies are medications that are designed to attack cancer cells and leave normal cells largely untouched.
- Radiation Therapy. ...
- Immunotherapy. ...
Why small cell lung cancer is tough to treat?
Treatment Surgery (wedge resection, lobectomy, or pneumonectomy). Surgery is the most effective for combating large cell carcinoma... Radiation Therapy or Chemotherapy. Radiation …
What to expect from lung cancer treatment?
· Treatment Surgery. In the earlier stages of large cell carcinoma, a person may only require surgery. Here, a healthcare... Chemotherapy. Chemotherapy is a systemic treatment for …
What is life expectancy after lung cancer?
Surgery is a common treatment method for large cell carcinoma. It might be recommended for numerous reasons, such as to remove a tumor or at least remove some so it is smaller. …
Is there a cure for small cell lung cancer?
· Giant cell carcinoma of the lung (GCCL) is a rare variant of non-small cell lung carcinoma (NSCLC), accounting for 0.1–0.4% of all lung cancers . It is clinically aggressive with …

Is large cell lung cancer treatable?
For example, large cell neuroendocrine carcinoma, a rare type of LCLC, has a median survival rate of about 6 months after diagnosis. Many individual factors, as well as diagnosis and treatment, are all factors in your prognosis with LCLC. Survival rates are improving with advanced treatments.
How is large cell carcinoma treated?
According to the National Cancer Institute, the treatment options are as follows:Surgery. In the earlier stages of large cell carcinoma, a person may only require surgery. ... Chemotherapy. ... Targeted therapy. ... Radiation therapy. ... Immunotherapy. ... Additional treatment options.
How long can you live with large cell carcinoma?
Currently, the five-year survival rate is approximately 11 percent for men and 14 percent for women (meaning, 11 and 14 percent of men and women have survived five years after diagnosis). Overall, the five-year survival rate for lung cancer is 18 percent.
Which type of lung cancer is more treatable?
Small cell lung cancer is the least common type of lung cancer, but it spreads faster than non-small cell lung cancer. Early lung cancer screenings can detect small cell lung cancer before it spreads, when the disease is most treatable by methods like radiation therapy, immunotherapy and chemotherapy.
What causes large cell lung carcinoma?
Smoking causes the majority of lung cancers — both in smokers and in people exposed to secondhand smoke. But lung cancer also occurs in people who never smoked and in those who never had prolonged exposure to secondhand smoke. In these cases, there may be no clear cause of lung cancer.
What is large cell carcinoma of the lung?
Large cell lung carcinoma (LCLC) is one of several forms of non-small cell lung cancer (NSCLC). LCLC often develops in the outer regions of the lungs and tends to grow rapidly and spreads more aggressively than some other forms of lung cancer. 1 Early symptoms of LCLC mainly include shortness of breath and fatigue.
Does 5 year survival rate mean you have 5 years to live?
Most importantly, five-year survival doesn't mean you will only live five years. Instead it relates to the percentage of people in research studies who were still alive five years after diagnosis.
Is small cell worse than large cell?
Some types are more aggressive than others, but generally, small cell cancer is more aggressive than non-small cell lung cancer.
Is Stage 4 always terminal?
Stage 4 cancer is not always terminal. It is usually advanced and requires more aggressive treatment. Terminal cancer refers to cancer that is not curable and eventually results in death. Some may refer to it as end stage cancer.
Which type of lung cancer is most likely to metastasis?
Lung carcinomas when detected are most often in a metastatic stage IV. Lung carcinomas metastasize by lymphatic as well as blood vessels.
Where is the first place lung cancer spreads?
Most lung cancers first spread to lymph nodes within the lung or around the major airways. 4 Lymph nodes are tiny organs clustered throughout the body that trap and filter foreign substances.
How successful is chemotherapy for lung cancer?
More important to patients, however, may be the comparison of 1 and 2 year survival; 29% of those treated with chemotherapy were alive at 1 year compared with 20% in the supportive care arm, and 2 year survival was doubled in the chemotherapy arm from 5% to 10%.
What is considered a large squamous cell carcinoma?
Stage 4 squamous cell carcinoma: In stage 4, the cancer can be any size and has spread (metastasized) to 1 or more lymph nodes which are larger than 3 cm and may have spread to bones or other organs in the body.
Is carcinoma life threatening?
Untreated squamous cell carcinoma of the skin can destroy nearby healthy tissue, spread to the lymph nodes or other organs, and may be fatal, although this is uncommon. The risk of aggressive squamous cell carcinoma of the skin may be increased in cases where the cancer: Is particularly large or deep.
How long does it take to recover from squamous cell carcinoma surgery?
The wound may take 3 to 6 weeks to heal. How long it takes depends on the size of the area treated. Good wound care may help the scar fade with time.
What is the difference between small cell and large cell carcinoma?
There are several key differences, including the outlook. In a person with small cell cancer, the cancerous cells appear small and round under a microscope. The cells of non-small cell lung cancer are larger. Smoking is a major risk factor for both types.
What is a large cell lung carcinoma?
What is large cell lung carcinoma? LCLC is a type of cancer that affects the lung. It can form anywhere in the lung but is more common on the outer edges. Non-small cell carcinomas, like LCLC, are the most common form of lung cancer, making up 80 to 85 percent of all lung cancers.
What is the name of the cancer that grows in the lungs?
Large cell carcinoma. This type of lung cancer is named so because of its large, abnormal-looking cells. These cells can be found throughout the lungs. They also tend to grow more quickly and spread faster than other forms of non-small cell lung cancers. LCLC makes up 10 to 15 percent of all non-small cell lung cancers.
Why do we need annual lung screenings?
If you’re at high risk for developing lung cancer, such as if you smoke or work around airborne chemicals, annual screenings can help your doctor make a diagnosis early.
How long do you live with LCLC?
For example, large cell neuroendocrine carcinoma, a rare type of LCLC, has a median survival rate of about 6 months after diagnosis.
How long do people with lung cancer live?
Early diagnosis is key to a good prognosis. Overall, about a quarter of the people with some form of non-small cell lung cancer live for at least 5 years after their diagnosis — up from about 16 percent. Trusted Source.
When is non-small cell lung cancer diagnosed?
Ideally, non-small cell lung cancers are diagnosed in the early stages, when there are more and better treatment options. However, since many symptoms are common to other conditions, a diagnosis isn’t made until the later stages in many cases of non-small cell lung cancer.
Is LCLC the same as nonsmall cell lung cancer?
Despite their unique qualities, LCLC and other forms of non-small cell lung cancer share the same symptoms, which may include:
What is a large cell lung carcinoma?
Large cell lung carcinoma (LCLC) is one of several forms of non-small cell lung cancer (NSCLC ). LCLC often develops in the outer regions of the lungs and tends to grow rapidly and spread more aggressively than some other forms of lung cancer. 1 Early symptoms of LCLC mainly include shortness of breath and fatigue.
What is the best immunotherapy for lung cancer?
As of October 2020, immunotherapy drugs approved by the U.S. Food and Drug Administration (FDA) for the treatment of lung cancer include: 18 1 Imfinzi (durvalumab): Approved for treating advanced NSCLC and SCLC, including use in first-line therapy 2 Keytruda (pembrolizumab): Approved for treating advanced NSCLC, including use in first-line therapy, and for some patients with SCLC 3 Opdivo (nivolumab): Approved for advanced NSCLC and SCLC after platinum-based chemotherapy and at least one other line of treatment has failed 4 Yervoy (ipilimumab): Approved for first-line use in combination with Opdivo in some cases of mesothelioma, a different type of cancer affecting lungs that's linked to asbestos exposure 5 Tecentriq (atezolizumab): Approved for advanced NSCLC and SCLC, including use in first-line therapy
Can a chest X-ray show lung cancer?
Lung cancer is often detected with a chest X-ray. With that said, a normal chest X-ray cannot rule out cancer, as smaller tumors are not usually visible with this type of imaging.
What genes are involved in LCLC?
Research suggests that certain gene mutations may contribute to the risk of some types of LCLC, including mutations of the RUNX1, ERBB4, BRCA1, and EPHA3 genes. 8. Risk Factors for Non-Small Cell Lung Cancer.
Is radon a risk factor for lung cancer?
Exposure to radon in the home is the second leading risk factor for lung cancer. Produced by the breakdown of natural uranium in soil, radon is found in excessively high levels in many houses. 6
What percentage of lung cancers are caused by paraneoplastic syndrome?
Paraneoplastic syndromes occur in 5% to 10% of all lung cancers and can develop in the early stages of malignancy. 4
What are the symptoms of LCLC?
The symptoms include dyspnea, and pain in the chest or side that gets worse with a deep breath. 3.
What is the treatment for nonsmall cell lung cancer?
Immunotherapy is a type of treatment that boosts the body’s natural immune response to combat cancer cells, thus circumventing side effects caused by systemic treatments like radiation and chemotherapy. There are several immunotherapy drugs now being used to treat non-small cell lung cancers.
What is the best treatment for large cell carcinoma?
Surgery is the most effective for combating large cell carcinoma when it is treated at an early stage. Wedge resection, lobectomy, or pneumonectomy may all be options for removing the lung tumor. In wedge resection, the tumor and a portion of the surrounding tissue is removed. A lobectomy removes the entire lobe of the lung. And a pneumonectomy removes the entire lung. (Most people can live with one lung as long as the remaining lung is healthy!)
What does donating to LCFA do?
Stand with survivors and help fund lung cancer research. By donating to LCFA, you help to fund innovative new research in the field of lung cancer treatment.
What are the advances in treatment?
Topping the list are refinements in surgery, better diagnostic scanning, more precise use of radiation, the impact of newer drugs and genetic testing
What is progress in lung cancer research?
Progress in lung cancer research means that lung cancer patients can live longer, healthier lives. Your donation can help make sure that new, more effective treatments get to the people who need them most even faster.
What is targeted therapy?
Targeted therapy is a type of treatment that detects specific features of the targeted cell, such as mutations or other characteristics, and disrupts the functioning of those specific cells – thus minimizing side effects of non-targeted, systemic treatments. There are several drugs being used to treat non-small cell lung cancers based on the tumors’ biomarkers. Make sure to request for biomarker testing to understand your best options for treatment.
What is stage IV cancer?
Stage IV: the cancer has spread (metastasized) to other areas of the body outside the lungs
What are the two types of lung cancer?
According to the American Cancer Society, the two main types of lung cancer are small cell lung cancer (SCLC) and NSCLC. Large cell carcinoma is a type of NSCLC. The National Cancer Institute state that large cell carcinoma is a type of cancer that can begin in several types of large cells. As the name suggests, these cancer cells appear larger ...
What is the best way to treat a tumor in the airways?
For tumors in the airways, a healthcare professional uses an endoscope to apply the radiation directly to the tumor.
What is targeted therapy?
Targeted therapy involves the use of drugs to target cancer cells without affecting normal cells.
What is the cause of 90% of lung cancer cases?
The American Lung Association estimate that the cause of almost 90% of lung cancer cases is smoking.
Can you have surgery for large cell carcinoma?
In the earlier stages of large cell carcinoma, a person may only require surgery. Here, a healthcare professional will remove all or part of the cancer, depending on the size and location.
What is the staging system for large cell carcinoma?
Healthcare professionals usually categorize large cell carcinoma and other NSCLC in stages using the Tumor Node Metastasis system, also known as TNM staging.
How do you know if you have lung cancer?
Some of the most common symptoms of large cell carcinoma and other types of lung cancer include: persistent cough. coughing up blood or rust-colored phlegm. hoarse voice. chest pain that worsens with deep breathing, laughing, or coughing. loss of appetite. shortness of breath. fatigue. unexplained weight loss.
How to treat large cell carcinoma?
Surgery is a common treatment method for large cell carcinoma. It might be recommended for numerous reasons, such as to remove a tumor or at least remove some so it is smaller. Removing some of it, a process referred to as debulking, may help reduce the risk of damage to the nearby body structures. This could also be done to decrease certain symptoms the tumor and its size might be causing. Surgical procedures may be done during the diagnostic phase to help in staging cancer or confirming the diagnosis of this disease. It might also be used to improve the efficacy of other treatments or as a palliative measure when a patient’s cancer is advanced. There are numerous techniques surgeons might employ for cancer. Cryosurgery kills cancer cells via freezing temperatures and electrosurgery kills cancer cells via an electrical current. Laser procedures might be considered when the surgeon needs extreme precision or when tumors are tiny. Microscopically controlled procedures may be done when delicate areas are being operated on.
Why are these two treatments often used together for large cell carcinomas?
These two treatment options are often used together for large cell carcinomas because they can boost the efficacy of each other and other cancer treatments. Continue to reveal more treatments for large cell carcinoma.
How does immunotherapy work for cancer?
This may be accomplished by attacking the cells via stimulating the patient’s immune system or by providing the patient’s immune system with certain proteins and other components. There are four primary types of this therapy being used for cancer regularly. Immune checkpoint inhibitors essentially stop the body from keeping the immune system in check, so it has free rein to kill cancer cells. Non-specific immunotherapies provide a general boost to the immune system so it has the strength it requires to attack cancer cells. Monoclonal antibodies are a type of man-made immune system protein. These are made in a way that allows them to precisely focus and only attack a particular cancer cell component. Cancer vaccines are also classified as this type of therapy. They are typically used as a preventative measure, but in some cases, they may also be used as part of a treatment regimen.
How does radiation help cancer?
Chemotherapy and radiation are among the most common cancer treatments. There are dozens of medications administered in several ways, such as orally, intrathecally into the space between the spine or brain and the tissue covering them, intra-arterially into an artery, intravenously, intraperitoneally into the peritoneal cavity, or topically. The purpose of chemotherapy is to shrink tumors, improve the efficacy of other treatments, and kill cancer cells. Radiation uses intense forms of energy to destroy cancer cells. The internal radiation type involves inserting liquid or solid radiation into the body at the cancer site. The external radiation type uses machines that aim the radiation at the area of the body where the cancer is present. For example, the machines will be aimed at the chest when using radiation for lung cancer. These two treatment options are often used together for large cell carcinomas because they can boost the efficacy of each other and other cancer treatments.
What is targeted therapy?
Targeted therapies involve various drugs technically considered types of chemotherapy. However, compared to chemotherapy, targeted medications do have different mechanisms of action. For example, certain medications in this category might focus on the inner workings of a cell, which would result in the cancer cells being impacted and the healthy cells being left alone. The purpose of these therapies is to focus solely on the cancer cells. These medications can differentiate between healthy cells and cancer cells due to the DNA changes cancer cells undergo, making it possible for these therapies to switch off or block chemical signals, so the cancerous cells stop dividing or growing. They may cause cancer cell death via inhibiting blood vessel growth to the tumor or by changing proteins or kill the cancer cells by delivering toxins to them. These therapies may also work to kill cancer cells by triggering the patient’s immune system. The administration of these therapies depends on the medication used and may include any of the chemotherapy delivery routes.
What is the treatment for giant cell carcinoma of the lung?
Giant cell carcinoma of the lung successfully treated with surgical resection and adjuvant vinorelbine and cisplatin
What stage of lung cancer was T2N0MX?
The tumor stage was T2N0Mx, equal to stage 1b non-small cell lung cancer. Subsequently, the patient underwent right upper lobectomy with mediastinal lymph node dissection and received four cycles of adjuvant chemotherapy with vinorelbine and cisplatin. Eventually, the patient quit smoking and was successfully treated with no evidence of recurrence on further imaging and follow up.
Is GCCL a tumor?
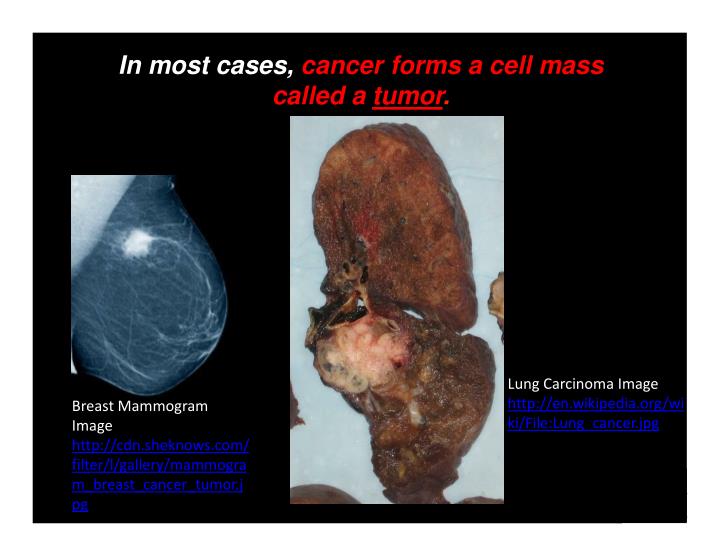
The majority of patients with suspected lung cancer require tissue biopsy to confirm the diagnosis [8]. GCCL is easily distinguished from other forms of lung cancers by histopathology [3]. Under the microscope, GCCL tumor cells are big, multi-core, bizarre with plenty of neutrophils and lymphocytes in the background [7]. A characteristic feature of GCCL is emperipolesis, which is the presence of collections of polymorphonuclear leukocytes within the giant cells, apparently phagocytosing cytoplasmic contents [7].
Is GCCL a NSCLC?
Giant Cell Carcinoma of the lung's existing literature is limited, and the current NSCLC's general literature guides the current management. Our patient's Giant Cell Carcinoma of lung was treated successfully with surgical resection and adjuvant vinorelbine and cisplatin. Giant cell carcinoma of the lung was first discovered and named by Nash and Stout in 1958 [5]. Giant Cell Carcinoma has been categorized by the World Health Organization as a sarcomatoid carcinoma [3], along with other subtypes, including pleomorphic carcinoma, spindle cell carcinoma, carcinosarcoma, and pulmonary blastoma [3]. GCCL is different from Large Cell Carcinoma of the lung which is also a subtype of NSCLC [6]. GCCL is associated with smoking, and it is more commonly seen in males [5]. GCCL can occur in any lung lobe, but it is more commonly found in the upper lobes [7]. GCCL may be asymptomatic like other NSCLCs, or patients may complain of non-specific signs and symptoms like cough or hemoptysis [7]. GCCL is a poorly differentiated tumor with early metastasis to the brain, bone, adrenal gland, and liver, through lymph and blood circulation. Uncommon metastasis to the gastrointestinal tract, kidney, and heart has also been reported [7].
How many people die from lung cancer every year?
Lung cancer is still the leading cause of cancer-related deaths, accounting for 1.4 million deaths worldwide [1] and approximately 160,000 deaths in the United States every year [1] with increasing incidence worldwide [2]. Giant cell carcinoma of the lung (GCCL) is a rare variant of non-small cell lung carcinoma (NSCLC), accounting for 0.1–0.4% of all lung cancers [3]. It is clinically aggressive with inadequate response to antitumor chemotherapy, resulting in a very poor prognosis [4]. Herein, we present a rare case of Giant Cell Carcinoma of lung treated successfully with surgical resection and adjuvant vinorelbine and cisplatin.
Is Giant Cell Carcinoma reportable?
Giant Cell Carcinoma's existing literature is limited, and hence our case is reportable. Our case is unique because of the better outcome which we believe might be the result of early detection and treatment with surgical resection along with adjuvant chemotherapy. More studies are needed to deeply understand the need for adjuvant chemotherapy in stage 1 b GCCL, and proper guidelines are required for the indications of adjuvant chemotherapy in Stage 1b GCCL.
Is GCCL a small cell lung cancer?
Giant Cell Carcinoma of the lung, a subtype of Sarcomatoid lung cancer is a poorly differentiated Non-Small-Cell Lung Cancer. GCCL has exceptionally aggressive characteristics, and its prognosis is much poorer than any other NSCLCs. Herein, we present a rare case of Giant Cell Carcinoma of lung treated successfully with surgical resection and adjuvant vinorelbine and cisplatin.
What is the response rate to platinum based chemotherapy?
Sun et al. [39] revealed that the response rate to platinum-based chemotherapy was 60 %, whereas the response rate to non-platinum-based chemotherapy was 11 %. Moreover, they examined whether advanced LCNEC should be treated similarly to SCLC versus non-SCLC with respect to chemotherapeutic regimens, and they concluded that advanced LCNEC could be treated appropriately in a manner similar to SCLC rather than NSCLC. Igawa et al. [40] reported that the effectiveness of chemotherapy for unresectable LCNEC was comparable to that for extended disease SCLC. Tokito et al. [41] reported that the response rate for SCLC-based chemotherapy was 70 % in patients with LCNEC. Shimada et al. [42] suggested that the overall response rate to initial chemotherapy or chemoradiotherapy and the survival outcomes of high-grade neuroendocrine carcinoma-probable LCNEC were comparable to those of SCLC, even though the efficacy of second-line chemotherapy might differ between LCNEC and SCLC. Yamazaki et al. [43] reported that the response rate of LCNEC to cisplatin-based chemotherapy was comparable with that of SCLC.
How long do LCNEC patients live?
Because most LCNECs have been diagnosed postoperatively by surgical specimens, many reports on LCNEC have referred to surgical cases, of which the majority [6, 20–27] revealed that patients with LCNEC had poor prognoses with five-year survival rates of 15–57 %. Moreover, even patients with pathological stage I LCNEC have had poor prognoses, with five-year survival rates of 27–67 % [22–26]. Iyoda et al. [28] compared the prognoses of LCNEC patients with pathological stage IA with those of patients with adenocarcinomas or squamous cell carcinomas of the same stage, and they revealed that the five-year survival rate of the LCNEC patients was 54.5 versus 89.3 % for the adenocarcinoma or squamous cell carcinoma patients. In LCNEC patients with complete resection, many recurrent tumors were observed as distant metastases [29, 30]. Therefore, surgery alone is not sufficient to treat patients with LCNEC, and subsequent adjuvant therapy may be necessary [4, 31, 32]. In 2001, Iyoda et al. [33] reported that postoperative adjuvant chemotherapy was effective in patients with LCNEC. Veronesi et al. [23] reported that 12 of 15 LCNEC cases administered induction chemotherapy were responsive (a partial response in 11 patients, a complete response in one patient) and that stage I LCNEC patients with induction or adjuvant chemotherapy tended to have a better survival than those without such therapies (p = 0.077). In 2005, in a retrospective study by Rossi et al. [25] adjuvant chemotherapy with CDDP+VP-16 was reported to be effective for patients with LCNEC. Iyoda et al. [34] started a prospective study of adjuvant chemotherapy in patients with LCNEC in 2000, and they selected CDDP+VP-16 as the chemotherapeutic regimen because the clinicopathologic and biological features of LCNEC are very similar to those of SCLC. They reported in 2006 that patients with adjuvant chemotherapy after complete surgical resection had a good prognosis compared with the historical control group.
Is platinum based chemo effective for LCNEC?
Many reports revealed that platinum-based and SCLC-based chemotherapies were effective for patients with LCNEC. However, those results were not enough to improve the prognoses of patients with LCNEC, especially those with advanced stages. Therefore, we need to discover new treatments for patients with LCNEC.
Can you have surgery with stage 1 SCLC?
The indication for surgery is limited to stage I in patients with SCLC, however, surgery with adjuvant chemotherapy may achieve satisfactory results in terms of survival in regard to surgical indications for patients with not only stage I but also stage II/III in LCNEC [46]. Iyoda et al. [29] reported that platinum-based adjuvant chemotherapy after surgery might be useful for preventing recurrence in patients with LCNEC. Therefore, surgical indications for patients with LCNEC may not be limited to clinical stage I cases, and surgery with adjuvant chemotherapy should be attempted for resectable LCNEC.
Can perioperative chemotherapy help with LCNEC?
Recently, many studies have reported that perioperative chemotherapy may be beneficial in patients with resected LCNEC [32, 36, 37]. Tanaka et al. [38] performed a unique study and suggested that perioperative chemotherapy might benefit the survival of patients with LCNEC if the tumors are not immunoreactive to the three neuroendocrine markers evaluated.
Is there a consensus on lung LCNEC?
Although we are beginning to understand the clinicopathological and biological features of patients with LCNEC little by little, there is no consensus on treatment in patients with lung LCNEC. We need large-scale trials in order to reach a consensus; however, in the near future, we may not be able to perform such trials because of the rarity of LCNEC cases. Therefore, we should continue trying to obtain useful information from several small-scale studies as well as to evaluate new strategies, including molecular targeted therapies, for patients with LCNEC.
Is LCNEC the same as SCLC?
Several reports [5–7] revealed that the clinical behavior, morphology, and prognosis of LCNEC were similar to those of SCLC, even though there might be several clinicopathological differences between SCLC and LCNEC in peripheral, small-sized, high-grade neuroendocrine tumors [8]. Although Varlotto et al. [9] obtained and evaluated data on LCNEC from the Surveillance, Epidemiology, and End Results Program to show that the clinical, histopathologic, and biologic features of LCNEC were more similar to those of large cell carcinoma than SCLC, a central pathological review by an expert panel was necessary to confirm the diagnosis, a requisite lacking in the report by Varlotto et al. [10, 11]. Cytomorphologically, LCNEC shows characteristic arrangements, such as palisading or rosettes with necrosis [12]. Morphometric analysis revealed significantly different features between LCNEC and classic large cell carcinomas. Iyoda et al. [13] showed that LCNEC had significantly higher expression rates of Bcl-2 and the Ki-67 labeling index than did classic large cell carcinoma. These results revealed that the cytological and biological features of LCNEC were different from those of classic large cell carcinoma. Jones et al. [14] examined the gene expression profiles of LCNEC, SCLC, adenocarcinoma, and normal lung using microarray analysis, which was unable to distinguish LCNEC from SCLC. Using the telomeric repeat amplification protocol assay, Zaffaroni et al. [15] reported that almost all LCNEC tumors showed telomerase activity comparable to that of SCLC.
What are the characteristics of pulmonary LCNEC?
Pulmonary and extra-pulmonary LCNEC share many similar clinical characteristics. Patients with pulmonary LCNEC were more likely to be white males (9, 30). Patients with pulmonary LCNEC are less likely to present with advanced stage disease as compared to SCLC (31) . Cough is the most common presenting symptom of pulmonary LCNEC (32). Although pulmonary LCNECs can occur throughout the lungs, they are most likely to occur in the upper lung lobes (33). In large studies of GI HGNEC, most patients are also men, most patients are in their 60s, and most are white. The majority of patients also presented with stage IV disease. In one large study the most common primary site was the colon, followed by pancreas, and esophagus (34). Other studies showed that the stomach and small intestine were also frequent sites of HGNEC (35). Pulmonary LCNEC is commonly associated with a smoking history (36, 37). In limited data available, patients with a history of colorectal HGNEC are slightly more likely to describe a history of smoking but the contrast with nonsmokers is less pronounced than in pulmonary disease. In addition common presenting symptoms include abdominal pain, hematochezia, melena, and altered bowel movements (38). Although data is limited in extra-pulmonary LCNEC and OS is variable depending on primary site (39), in large studies 5 year OS in pulmonary LCNEC was 16.7% (9) and 13.3% (40) in colorectal HGNEC. Brain metastasis are more common in pulmonary LCNEC (12-19.2% at presentation in large studies) (8, 41) versus1.6% in GI HGNEC (31).
How many mitoses are in a carcinoid?
Carcinoid morphology with 2 to 10 mitoses/2mm2, or necrosis
What is a LCNEC?
Large cell neuroendocrine carcinoma (LCNEC) is a rare subgroup of high grade neuroendocrine cancer that can occur throughout the body (Figure 1). The most common primary site is the lung, however, LCNEC also occurs in the gastrointestinal tract and in other locations including cervix, uterus, kidney, bladder, prostate, pharynx, larynx and many other primary sites (Figure 2) (1–6). LCNEC is an aggressive, fast growing neuroendocrine carcinoma, similar to small cell lung cancer (SCLC). The incidence of LCNEC is increasing worldwide. Most LCNEC originates in the lungs and pulmonary LCNEC represents 2 to 3.5% of all lung cancers (7). In studies using SEER data, age adjusted incidence of pulmonary LCNEC is 0.3 per 100,000 with a rise by 0.011 people per 100,000 per year from 2004-2015 (8, 9). In addition to pulmonary LCNEC, there is evidence that LCNEC of all sites are increasing. A Dutch registry study of 47,800 patients with neuroendocrine tumors examined LCNECs, revealing an increase in incidence of LCNEC of all sites from 0.01 per 100,000 people to 1.8 per 100,000 people in 2010 (10). In this same population 5 year overall survival (OS) of patients with LCNEC was 20% (10, 11). This manuscript is intended to review current best evidence of management of this rare and deadly disease as well as several promising new directions for classification and treatment.
Is LCNEC a rare disease?
Large cell neuroendocrine carcinoma (LCNEC) is a rare, aggressive cancer with a dismal prognosis. The majority of cases occur in the lung and the gastrointestinal tract; however, it can occur throughout the body. Recently advances in the understanding of the molecular underpinnings of this disease have paved the way for additional novel promising therapies. This review will discuss the current best evidence for management of LCNEC and new directions in the classification and treatment of this rare disease.
Is PD-L1 associated with lower overall mortality?
In combined assessment of 74 SCLC and 41 LCNEC PD-L1 expression was significantly associated with lower overall mortality.
Large Cell Lung Cancer Symptoms
Causes
- Risk factors for LCLC are the same as the risk factors for other forms of lung cancer. Smoking is the single greatest risk factor for lung cancer. Even living with someone who smokes increases a nonsmoker's risk of lung cancer by 20% to 30%.5 Exposure to radon in the home is the second leading risk factor for lung cancer. Produced by the breakdown of natural uranium in soil, radon i…
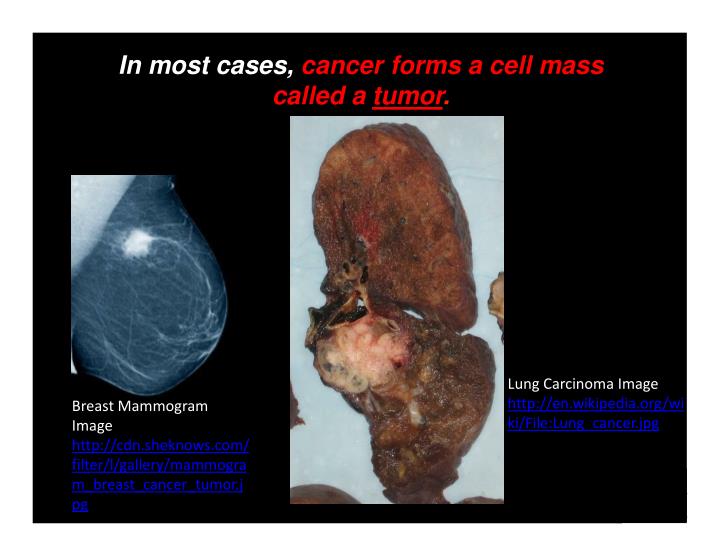
Diagnosis
- Lung cancer is often detected with a chest X-ray. With that said, a normal chest X-ray cannot rule out cancer, as smaller tumors are not usually visible with this type of imaging. If any symptom of LCLC is present, further testing is usually pursued even if a chest X-ray is normal. These tests may include:9 1. Computed tomography (CT)scan, which uses multiple X-ray images to create a thre…
Stages
- The extent and severity of lung cancer is broken down into four stages.10 They range from stage 1, in which the cancer is localized within the lung and has not spread to any lymph nodes, to stage 4, in which cancer has metastasized (spread) to distant parts of the body.
Treatment
- Depending on the stage of cancer, treatment options for LCLC include surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, or a combination of these. Clinical trialsare also available for those who may not be responding to standard therapy.
Prognosis
- The stage of lung cancer can help predict a patient's long-term outcome. The prognosis is typically described by the five-year survival rate, which estimates the percentage of people who will survive for at least five years after the diagnosis. According to the American Cancer Society, as of January 2021, the five-year survival rates for people with LCLC and other NSCLCs like aden…
Coping
- A diagnosis of lung cancer can be frightening and make you feel very alone. Allow your loved ones to support you. Many people have no idea how to react to someone who has been diagnosed with cancer. Letting people know specific things they can do can help provide you with extra support when you need it. You can better cope with LCLC by learning as much as you can about the dise…
A Word from Verywell
- Although people with lung cancer have historically had less than favorable prognoses, treatments and survival times are improving every year. If you are uncertain about a recommended treatment plan, do not hesitate to seek a second opinion, such as from a large National Cancer Institute-designated treatment center. Your team of oncologists should be knowledgeable about the late…