Full Answer
What is the best medication for treatment resistant depression?
- Repetitive transcranial magnetic stimulation (rTMS). This type of treatment uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression. ...
- Ketamine is a medication that's delivered through an IV in low doses. ...
- Electroconvulsive therapy (ECT). ...
- Vagus nerve stimulation (VNS). ...
What are the options for treatment resistant depression?
Treatment-Resistant Depression: Options to Ask Your Doctor About. The options for the treatment of treatment-resistant depression include: Making changes to your medication: It may be that you need to try a new medication for treatment-resistant depression, or that you need to increase your current dose. Your doctor might suggest a different type of antidepressant or consider tweaking your drug schedule before exploring other treatment-resistant depression options.
How do you treat treatment resistant depression?
Psychedelic-assisted psychotherapy works to create a therapeutic model which improves clinical symptoms and promotes lasting, positive change for patients. Through this partnership with leading psychiatrists and researchers, Beckley Psytech aims to develop a holistic system which will enable delivery of the best care to patients.
How to treat severe depression?
FITCHBURG (WKOW) -- Despite its reputation as a party drug, recent studies have shown ketamine can be used to treat people with severe depression. And now, Fitchburg's first ketamine clinic is set to open in just a couple of weeks. The face behind it all ...

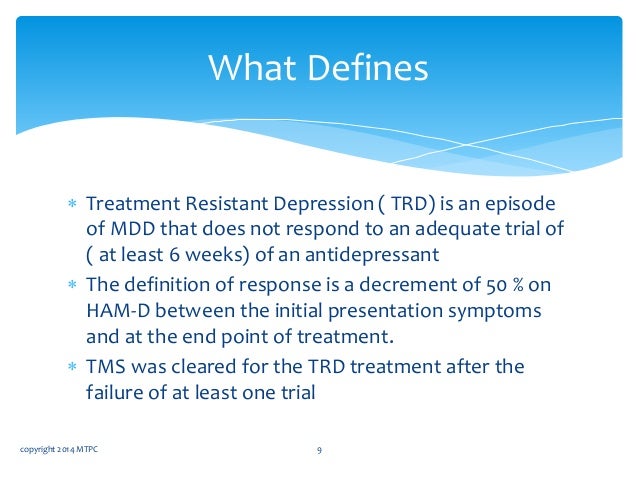
What is treatment-resistant depression definition?
Abstract. Treatment-resistant depression (TRD) typically refers to inadequate response to at least one antidepressant trial of adequate doses and duration. TRD is a relatively common occurrence in clinical practice, with up to 50% to 60% of the patients not achieving adequate response following antidepressant treatment ...
What is treatment-resistant major depressive disorder?
A major depressive disorder, TRD describes depression that has failed to respond to at least two different antidepressant treatments. Anyone who has experienced depression knows how inescapable and hopeless it can feel.
What is the criteria for treatment-resistant depression?
A general consensus is emerging that unipolar major depression is considered resistant or refractory when at least two trials with antidepressants from different pharmacologic classes (adequate in dose, duration, and compliance) fail to produce a significant clinical improvement.
What is treatment-resistant mental illness?
Treatment resistance comprises the trinity of establishing the correct psychiatric diagnosis, adequate treatment (in terms of dose and duration), and inadequate symptomatic response. It is commonly seen in many psychiatric disorders and associated with substantial functional impairment and economic and social costs.
Is treatment-resistant depression permanent?
Taking an antidepressant or going to psychological counseling (psychotherapy) eases depression symptoms for most people. But with treatment-resistant depression, standard treatments aren't enough. They may not help much at all, or your symptoms may improve, only to keep coming back.
What medications are used for treatment-resistant depression?
These are often the first antidepressant prescribed, because they're less likely to cause side effects. They include fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), and escitalopram (Lexapro). Serotonin and norepinephrine reuptake inhibitors (SNRIs).
How does the FDA define treatment-resistant depression?
Patients with major depressive disorder who, despite trying at least two antidepressant treatments given at adequate doses for an adequate duration in the current episode, have not responded to treatment are considered to have treatment-resistant depression.
What is the prognosis for treatment-resistant depression?
Complete remission is achieved in 70%–90% of patients with depression, leaving 10%–30% refractory to treatment, and managed by a variety of therapeutic modalities. Unfortunately, approximately 30% of patients with treatment-resistant depression do not respond to any treatment.
What is the most effective drug for treatment-resistant depression?
Esketamine reduces depression symptoms in a majority of these people in clinical trials. The only other approved drug therapy for treatment-resistant depression is a combination of olanzapine (an antipsychotic drug) and fluoxetine (a conventional antidepressant).
How many treatments are needed for TRD?
Other experts say that a person needs to try at least four different treatments before depression can be truly considered treatment-resistant.
How to help someone with depression?
Talk therapy. Approaches like cognitive behavioral therapy - which focuses on concrete goals and how your own thoughts and behaviors contribute to your depression -- can really help people with depression. There’s some evidence it works especially well with treatment-resistant depression.
What is ECT therapy?
ECT (electroconvulsive therapy.) ECT is typically used in people with serious or life-threatening depression that can’t be resolved by other treatments, or in significant depressive episodes that have not gotten better after several medication trials. It uses electric impulses to trigger controlled seizures in the brain. A series of ECT treatments (usually 6-12 over a few weeks) can often rapidly relieve depression, although some form of continued therapy (either a medicine or else periodic ECT "booster" treatments are usually necessary to prevent relapse.
How many people with depression don't respond to antidepressants?
As many as two-thirds of people with depression aren't helped by the first antidepressant they try. Up to a third don't respond to several attempts at treatment. Treatment-resistant depression (TRD) can leave you feeling hopeless and discouraged. Months or even years can go by without any relief.
How long does it take for depression medication to take effect?
They miss doses or stop taking them because of side effects. Some give up too soon - it can take 4-12 weeks for a medicine to take effect. Sometimes taking a medicine at too low a dose also explains an inadequate response.
What to do if your depression isn't working?
But if your depression treatment isn't working, don't give up. Many people can get their treatment-resistant depression under control. You and your doctor just need to find the right approach. This might include different drugs, therapy, and other treatments.
Can thyroid problems cause depression?
Check for other causes. Other issues - ranging from thyroid problems to substance abuse - can worsen or cause depression. So can many medicines used to treat common medical problems. Sometimes, switching medicines or treating an underlying condition can resolve a hard-to-treat depression.
What is treatment resistant depression?
What is treatment-resistant depression? Feeling sad or hopeless from time to time is a normal and natural part of life. It happens to everyone. For people with depression, these feelings can become intense and long-lasting. This can lead to problems at work, home, or school.
What is the first choice for treating depression?
Antidepressants. Antidepressant medications are the first choice for treating depression. If you’ve tried antidepressants without much success, your doctor will likely start by suggesting an antidepressant in a different drug class. A drug class is a group of medications that work in a similar way.
How long does it take for an antidepressant to work?
However, some research shows that people who show some improvement within a couple weeks of starting an antidepressant are more likely to eventually have a full improvement in their symptoms. Those who don’t have any response early in treatment are less likely to have full improvement, even after several weeks.
What is it called when you don't respond to antidepressants?
Depression that doesn’t respond to antidepressants is known as treatment-resistant depression. Some also refer to it as treatment-refractory depression. Read on to learn more about treatment-resistant depression, including treatment approaches that can help.
What are the risk factors for depression?
These risk factors include: Length of depression. People who’ve had major depression for a longer period of time are more likely to have treatment-resistant depression. Severity of symptoms. People with very severe depression symptoms or very mild symptoms are less likely to respond well to antidepressants.
What are the factors that affect the effectiveness of antidepressants?
Genetic factors. One or more genetic factors likely have a role in treatment-resistant depression. Certain genetic variations may increase how the body breaks down antidepressants, which could make them less effective. Other genetic variants might change how the body responds to antidepressants.
Does methylphenidate help with depression?
For example, in one study, using methylphenidate with antidepressants didn’t improve overall symptoms of depression. Similar results were found in another study that looked at the use of methylphenidate with antidepressants and one that evaluated using modafinil with antidepressants.
What is TRD treatment?
Treatment-resistant depression (TRD) is a subset of Major Depressive Disorder which does not respond to traditional and first-line therapeutic options. There are several definitions and staging models of TRD and a consensus for each has not yet been established. However, in common for each model is the inadequate response to at least 2 trials of antidepressant pharmacotherapy. In this review, a comprehensive analysis of existing literature regarding the challenges and management of TRD has been compiled. A PubMed search was performed to assemble meta-analyses, trials and reviews on the topic of TRD. First, we address the confounds in the definitions and staging models of TRD, and subsequently the difficulties inherent in assessing the illness. Pharmacological augmentation strategies including lithium, triiodothyronine and second-generation antipsychotics are reviewed, as is switching of antidepressant class. Somatic therapies, including several modalities of brain stimulation (electroconvulsive therapy, repetitive transcranial magnetic stimulation, magnetic seizure therapy and deep brain stimulation) are detailed, psychotherapeutic strategies and subsequently novel therapeutics including ketamine, psilocybin, anti-inflammatories and new directions are reviewed in this manuscript. Our review of the evidence suggests that further large-scale work is necessary to understand the appropriate treatment pathways for TRD and to prescribe effective therapeutic options for patients suffering from TRD.
How many trials of antidepressants are there for TRD?
Although many definitions for TRD have been proposed, the general consensus appears to be 2 unsuccessful trials of antidepressant pharmacotherapy (AD). Several “staging” models to classify levels of treatment resistance have been proposed. The initial model proposed by Thase and Rush138included treatment resistance levels ranging from one failed AD trial to a lack of response to electroconvulsive therapy (ECT). Further staging models have included the Massachusetts General Hospital Staging method117which carefully documents the optimization of medication doses and number of failed medications. The Souery Operational Criteria for TRD provide a slightly different approach to staging TRD as an illness, by defining TRD as any single failure of an adequate (6–8 week) trial of an AD.133The Maudsley Staging Method (MSM) assesses treatment resistance in depression in a “multi-dimensional” manner.34The majority of investigations into TRD utilize the definition of at least 2 suitable trials of AD without adequate response, although even the term “adequate response” may be fraught with contention, as there is not consensus on what constitutes “adequate.” In fact, even the term TRD may not be the ideal term to define a depressive illness that is not responding to therapeutic interventions. The term “difficult-to-treat depression” has been suggested, with the benefit of not introducing any “therapeutic nihilism” to the psychiatrist–patient relationship.103For consistency in this manuscript, we will use the term TRD. There has been considerable debate regarding what constitutes TRD, and whether medications from more than one class must be trialed prior to meeting criteria for this classification, or that the focus should be regarding homogeneous biological subtypes or endophenotypes.23However, the argument may be made that lack of achieving remission may be classified as an inadequate response as residual depressive symptoms can significantly contribute to difficulty functioning. Chronically depressed patients have a lower chance of recovery,98and often suffer from TRD.25,87
What are the perils of diagnosing TRD?
One of the perils of diagnosing TRD is that of “pseudo-resistance”.107Pseudo-re sistance may encompass the profile of patients who unfortunately were prescribed suboptimal doses of AD or had early discontinuation of a medication for any number of reasons, including intolerable side effects, patient non-adherence or under-dosing. Further, comorbidities such as anxiety disorders, personality disorders or substance-use disorders may complicate the clinical picture and can have deleterious effects on treatment response.114,127When interviewing patients in assessment of TRD, the potential for recall bias when reporting pharmacological trials and response adds a significant layer of difficulty in diagnosing TRD. Prospectively using objective clinical scales such as the Hamilton Depression Rating Scale48and the Inventory of Depressive Symptomatology124and retrospectively using treatment history forms such as the Antidepressant Treatment History Form (ATHF)127can be very helpful in delineating the nature and course of the treatment resistance. Since the ATHF was initially developed, there have been several developments in the treatment of MDD and specifically TRD, some of which will be elaborated upon in the ensuing sections of this paper. As such, the authors of the original ATHF127developed an updated and revised version, the short form ATHF (ATHF-SF), as well as an instruction manual and scoring checklist, among other documents.128Importantly, the ATHF-SF focuses on the current episode of depression, as opposed to life-time trials of pharmacological treatments, a more streamlined approach to assessing the level of resistance of the current illness episode. Utilizing a standardized approach to understand the level of treatment resistance in the current episode of depression may provide a useful measure of consistency in assessment of TRD.
How often is ECT used for TRD?
In the treatment of TRD, ECT is applied 2–3 times per week and acute courses can range between 6–18 total sessions. A report from the Consortium for Research in ECT (CORE)57revealed that over half of the subjects showed an improvement within the first week. Other studies have reported that over 50% of patients who have failed to respond to one or more adequate antidepressant medication trials respond to ECT.120Meta-analyses have shown that ECT is superior to sham ECT, placebo or antidepressant medications.45,111
How long does it take for a patient to go into remission after taking antidepressants?
Several large-scale clinical trials have examined response rates to traditional therapeutic approaches for depression. In the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, the cumulative remission rate after 4 trials of antidepressant treatment (within 14 months) was 67%.125Even after sequential treatments, 10% to 20% of the MDD patients remained significantly symptomatic for 2 years or longer.69,70In general, it is accepted that although antidepressant medications can be effective in treating MDD, they fail to achieve remission in approximately 1 out of 3 patients.73
Is TRD a first line treatment?
There are multiple modalities of somatic or brain stimulation therapies which have been investigated and applied in the treatment of TRD and are not first line but are turned to once several trials of pharmacotherapy and/or psychosocial therapies have been ineffective.
Is mood disorder a disorder?
Major Depressive Disorder (MDD) and associated mood syndromes are among the most common psychiatric disorders in specialist and general medical practice. These syndromes span life stages and present with varying combinations of symptoms. While depressive symptoms are at times part of normal human behavior, MDD can be debilitating and at its worst, life threatening. MDD can present at any age across the life span, differences in biological vulnerability, age of onset, risk factors, symptomatic presentation and comorbidities are present among people with the same diagnosis. MDD is, therefore, a very heterogeneous disorder, and approximately 30% of people with this illness are resistant to conventional treatments.96
How many prior treatment failures are required for TRD?
The most common TRD definition for major depressive disorder required a minimum of two prior treatment failures and confirmation of prior adequate dose and duration. The most common TRD definition for bipolar disorder required one prior treatment failure.
Is there consensus on TRD?
Results: We found that no consensus definition existed for TRD. The most common TRD definition for major depressive disorder required a minimum of two prior treatment failures and confirmation of prior adequate dose and duration. The most common TRD definition for bipolar disorder required one prior treatment failure. No clear consensus emerged on defining adequacy of either dose or duration. Our systematic review found that only 17% of intervention studies enrolled samples meeting the most frequently specified criteria for TRD. Depressive outcomes and clinical global impressions were commonly measured; functional impairment and quality-of-life tools were rarely used.
What other treatments might doctors try for TRD?
Light therapy is a well-established treatment option for people whose depression may be seasonal. If your mood deteriorates in the fall months, it may have a seasonal component.
What are common challenges in treating TRD?
To find the best treatment, it’s important to understand other conditions you may have, like anxiety, obsessive-compulsive disorder, personality disorder, or other medical problems.
How do you know it’s TRD?
Most experts would agree the definition of treatment-resistant depression is the failure of two or more antidepressants, prescribed and taken at maximum dose, for at least 6 weeks each.
What can you do to improve your chances of finding a treatment that works?
Work with your primary care provider and a therapist to try different strategies. It may be helpful to consult an experienced psychiatrist or psychopharmacologist.
What is treatment-resistant depression (TRD)?
If a doctor diagnoses you with TRD, this usually means that you have not responded to at least two different antidepressants after taking them with proper dose and duration. If symptoms of depression, such as sadness, an “empty” mood, hopelessness, decreased energy and concentration, thoughts of or attempts at suicide, etc., continue after you have tried two or more treatments, you may have TRD.
How is TRD treated?
There are many ways to treat TRD. In addition to the wide variety of traditional antidepressants available, there are newer medical treatments such as psychedelic medicine and transcranial magnetic stimulation (TMS).
How to keep track of mood?
Keep track of your mood and symptoms while seeking and trying new treatments. You can do this by writing in a journal, on a calendar or even an app. This can be shared with your doctor to ensure that you are getting the best treatment possible
Can you have TRD if you have depression?
If you have TRD, you are not alone: TRD affects about one third of Americans with depression [1].
Can you take antidepressants with TRD?
Antidepressants may still work for people with TRD. It is possible that you just haven’t found one that works best for you, so this may still be an option that is available. Different antidepressants will work in different ways, and medications take from two or more weeks to become fully effective [3]. Sometimes you might need a higher dose of a medication that you’re trying for it to be effective. Many people find that combining more than one antidepressant can be helpful. Be sure to talk with your doctor about options if the antidepressant that you’re trying is not working.
Can antidepressants work for TRD?
If this treatment works for you, your symptoms may improve or go away completely. Antidepressants may still work for people with TRD.
Can medication help with depression?
It’s hard when you’re taking medication that is supposed to treat your depression, but nothing seems to be helping. If you’ve tried two or more treatments and you still experience symptoms of depression, you might have treatment-resistant depression (TRD).
