
Medication
For conditions like Wolff-Parkinson-White syndrome, in which a hair-thin strand of tissue creates an extra electrical pathway between the upper and lower chambers of the heart, radiofrequency ablation offers a cure.
Procedures
Mar 24, 2022 · Catheter ablation is the most common treatment for people who have WPW syndrome and symptoms of an arrhythmia. This procedure can cure WPW syndrome in most people. If this treatment works for you, you can go back to your normal activities. You may need one of more of the following treatments for an irregular heartbeat:
Therapy
Mar 14, 2018 · The treatment for Wolff-Parkinson-White syndrome may depend on whether a person has any symptoms of the syndrome. For people who do have symptoms, medications such as antiarrhythmic drugs may be recommended.
Nutrition
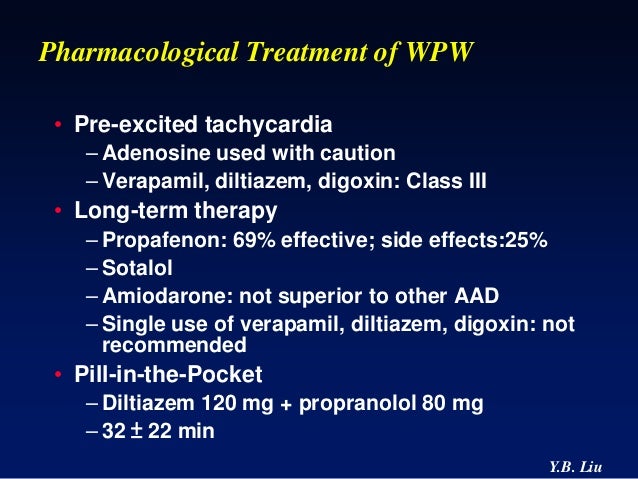
Aug 11, 2021 · Procainamide and cardioversion are accepted treatments for conversion of tachycardia associated with Wolff Parkinson White syndrome (WPW). In acute AF associated with WPW syndrome, the use of IV amiodarone may potentially lead to ventricular fibrillation in some reports and thus should be avoided.
Why is adenosine contraindicated in WPW?
Low-voltage, high-frequency electrical energy interrupts the extra pathway in your heart. Your doctor threads a catheter into your heart through a vein in your thigh. The treatment cures WPW about 95 percent of the time. Complications. WPW is not a dangerous disease for most people. You can manage or correct the condition with treatment.
How to treat WPW?
Treatment depends on the type and frequency of arrhythmias, associated symptoms such as syncope, and presence of structural heart disease. Typically a physician will recommend an ablation procedure to further define the characteristics of the accessory pathway, and ultimately, to eliminate the pathway entirely.
Can adenosine be used in WPW?
Sep 16, 2020 · WPW is a chronic condition that usually cannot be completely cured. Therefore, treatments focus on controlling and reducing the frequency of symptoms. Treatments can be used for both reducing short-term symptoms and reducing the frequency of symptoms in the long term. Short-term treatments
What is the prognosis of Wolff-Parkinson-White (WPW) syndrome?
Jan 14, 2021 · Treatments include methods to normalize the heart rate, removing the second pathway through procedures, as well as medication to limit possible adverse effects. You should visit your primary care physician soon to confirm the diagnosis and discuss treatment options. Wolff-Parkinson-White syndrome symptoms

What is the best treatment for Wolff-Parkinson-White Syndrome?
The choice is best made with a heart rhythm specialist (cardiac electrophysiologist) who has experience in treating the WPW syndrome. Radiofrequency ablation — Radiofrequency ablation of the accessory pathway is the treatment of choice for patients with WPW syndrome.Dec 19, 2019
Can WPW be treated with medication?
Their efficacy in reducing the risk of accelerated conduction of AF in WPW patients is unclear. More potent medications (eg, flecainide, propafenone, sotalol, or amiodarone) may have more effect on accessory pathway (AP) conduction or refractoriness than beta-blockers and are preferred by some.Jan 8, 2017
Does WPW require surgery?
Open heart surgery to burn or freeze the extra pathway may also provide a permanent cure for WPW syndrome. In most cases, this procedure is done only if you need heart surgery for other reasons.
What medications should not be taken with WPW?
Do not give digoxin or nondihydropyridine calcium channel blockers (eg, verapamil, diltiazem) to patients with atrial fibrillation and Wolff-Parkinson-White syndrome because these drugs may trigger ventricular fibrillation.
What is not allowed in WPW?
Do not use over-the-counter decongestants, diet pills, or "pep" pills. They often contain ingredients that make your heart beat faster (stimulants). Do not use illegal drugs, such as cocaine, ecstasy, or methamphetamine, which can speed up your heart's rhythm. Do not smoke.
How do you test for WPW?
If you have a fast heartbeat, your health care provider will likely recommend tests to check for WPW syndrome, such as: Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs.Jan 27, 2022
How serious is heart ablation surgery?
Ablation has serious risks, although they are rare. They include stroke and death. If ablation doesn't work the first time, you may need to have it done again.
Can WPW cause sudden death?
The episodes of fast heartbeats seen in WPW syndrome usually aren't life-threatening, but serious heart problems can occur. Rarely, WPW syndrome may lead to sudden cardiac death in children and young adults.Jan 27, 2022
How long does it take to recover from WPW surgery?
You'll spend a day or two in intensive care, and you may be in the hospital for up to a week. At first, you'll feel very tired and have some chest pain. You can probably go back to work in about 3 months, but it may take 6 months to get back to normal.Aug 10, 2020
Is WPW a serious heart condition?
Is it serious? It can be scary to be told that you have a problem with your heart, but WPW syndrome usually isn't serious. Many people will have no symptoms or only experience occasional, mild episodes of their heart racing. With treatment, the condition can normally be completely cured.
Why is procainamide used in WPW?
The use of intravenous procainamide is a reliable and rapid method of identifying patients with the Wolff-Parkinson-White syndrome who may be at risk for circulatory insufficiency or sudden death in case of atrial fibrillation.
Can beta blockers be used in WPW?
Beta blocker is also considered in pa- tients with arrhythmia related to an accessory pathway with a short refractory period. So, concomitant admin- istration of beta blocker and flecainide results in great- er long-term efficacy and can be one of options for the treatment of a patients with AF in WPW syndrome [9].Feb 27, 2019
What tests can be done to diagnose WPW syndrome?
Your doctor will likely recommend tests to diagnose WPW syndrome, such as: Electrocardiogram (ECG). Small sensors attached to your chest and arms record electrical signals as they travel through your heart. Your doctor can look for patterns among these signals that indicate an extra electrical pathway in your heart. Holter monitor.
What to do if you have WPW but don't have symptoms?
If you have the WPW pathway but don't have symptoms, you probably won't need treatment. If you do, the goal of treatment is to slow a fast heart rate when it occurs and to prevent future episodes. Treatment options include: Vagal maneuvers.
What is Holter monitor?
A Holter monitor is a portable ECG device at home that you wear when you're away from the doctor's office. The device records your heart's activity while you perform your everyday activities for a day or two. An event recorder monitors heart activity when your heart beats too fast.
What to do if you can't stop your heartbeat?
Medications. If vagal maneuvers don't stop the fast heartbeat, you might need an injection of an anti-arrhythmic medication. Your doctor also might recommend a medication that can slow the heart rate. Cardioversion.
What is a thin tube that is tipped with electrodes?
Thin, flexible tubes (catheters) tipped with electrodes are threaded through your blood vessels to various spots in your heart. The electrodes map the spread of electrical impulses during each heartbeat and identify an extra electrical pathway.
When is cardioversion used?
Cardioversion is typically used when maneuvers and medications aren't effective. Radiofrequency catheter ablation. Thin, flexible tubes (catheters) are threaded through blood vessels to your heart. Electrodes at the catheter tips are heated to destroy (ablate) the extra electrical pathway causing your condition.
How does catheter ablation work?
In catheter ablation, catheters are threaded through the blood vessels to the inner heart, and electrodes at the catheter tips map the spread of electrical impulses through the heart . Electrodes at the catheter tips transmit energy to destroy a small spot of heart tissue and create an electrical block along the pathway that's causing your arrhythmia.
What is the Wolff-Parkinson-White syndrome?
The term Wolff-Parkinson-White (WPW) syndrome is used to refer to the combination of supraventricular arrhythmias and an electrocardiographic pattern of preexcitation. This syndrome was first described in 1930 in an article by Louis Wolff, Sir John Parkinson, and Paul Dudley White.
What causes APs in the atria?
APs result from failure of fibrous separation between the atria and the ventricles during the embryological development. These muscle bundles typically connect the epicardial surfaces of the atria and the ventricles along the AV groove outside of the regular atrioventricular conduction system.
What is the frequency of preexcitation?
An electrocardiographic pattern of preexcitation occurs in the general population at a frequency of around 1.5 per 1000. Of these, 50% to 60% of patients become symptomatic. Approximately one-third of all patients with paroxysmal supraventricular tachycardia (PSVT) are diagnosed as having an AP-mediated tachycardia. Patients with AP-mediated tachycardias most commonly present with the syndrome of PSVT.
How many APs conduct both antegrade and retrograde?
About 60% of APs conduct both antegrade and retrograde. Antegrade-only APs are particularly uncommon (<5%). When present, they are usually right-sided and frequently demonstrate decremental conduction. Concealed APs account for approximately 17%-37% of all APs.
When was tachycardia first described?
This syndrome was first described in 1930 in an article by Louis Wolff, Sir John Parkinson, and Paul Dudley White. The authors described eleven patients with recurrent tachycardia associated with an ECG pattern of “Bundle Branch Block (BBB) with short PR interval.”. Since publication of this initial report, our understanding ...
Is catheter ablation considered first line therapy?
The Heart Rhythm Society Policy Statement on Catheter Ablation states that catheter ablation is considered first-line therapy (class 1) and the treatment of choice for patients with WPW syndrome. It is curative in more than 95% of patients and has a low complication rate. It also obviates the unwanted side effects of antiarrhythmic agents.
Is tachycardia a sign of syncope?
As in other supraventricular tachycardias, episodes of tachycardia may be associated with dyspnea, chest pain, decreased exercise tolerance, anxiety, dizziness, or syncope. Although syncope is often considered a bad prognostic sign, the evidence is not clear.
Why does Wolff-Parkinson-White syndrome occur?
In some cases, a genetic change ( mutation or pathogenic variant) in the PRKAG2 gene causes the syndrome.
What test is used to diagnose Wolff-Parkinson-White syndrome?
Because the symptoms of Wolff-Parkinson-White syndrome may only occur at certain times, a doctor may also recommend the use of a Holter monitor to confirm the diagnosis.
What is PRKAG2 inherited?
These cases appear to be inherited in an autosomal dominant manner. A diagnosis of the syndrome is based on an electrocardiogram (ECG) or Holter test that shows episodes of tachycardia.
What is the most common arrhythmia associated with Wolff-Parkinson-White syndrome?
The most common arrhythmia associated with Wolff-Parkinson-White syndrome is paroxysmal supraventricular tachycardia. The syndrome is especially common in people of Chinese descent. [1] In most cases, the cause of Wolff-Parkinson-White syndrome is unknown. A small percentage of cases are caused by genetic changes ( mutations or pathogenic variants) ...
How to determine if Wolff-Parkinson-White syndrome is sporadic?
A doctor may determine if other family members are at risk to have symptoms of Wolff-Parkinson-White syndrome by taking a detailed family history. If no other family members have symptoms of the syndrome, it is most likely that the syndrome is sporadic and is not caused by a pathogenic variant in PRKAG2. [1]
What is the Ebstein anomaly?
The Ebstein anomaly affects the tricuspid valve, which connects the right upper chamber of the heart ( atrium) to the right lower chamber ( ventricle ). However, some people with Wolff-Parkinson-White syndrome do not have any other heart abnormalities, and some people have no symptoms of the syndrome at all. [1]
What is the chance of inheriting Wolff-Parkinson-White syndrome?
When a person with Wolff-Parkinson-White syndrome that is caused by a pathogenic variant in PRKAG2 has children, for each child there is a: 50% chance to inherit the changed copy of the PRKAG2 gene, meaning he or she will have Wolff-Parkinson-White syndrome.
How to treat WPW?
Here are helpful lifestyle suggestions: 1 Don’t smoke. 2 Work with your doctor to keep conditions such as high cholesterol and high blood pressure under control. 3 Eat a heart-healthy diet. 4 Maintain a healthy weight. 5 Exercise regularly. 6 Tell your doctor right away if you have symptoms of WPW.
How does WPW affect the heart?
WPW affects one to three of every 1,000 people worldwide. Electrical signals going through your heart in an organized way control your heartbeat. This allows blood to pass from the upper chambers (the atria) to the lower chambers (the ventricles), and then to travel throughout your body. Normally, a structure in your heart called ...
Why is WPW a common cause of tachycardia?
WPW is a common cause of tachycardia in China, and you may be at increased risk if you are of Chinese descent.
How do you know if you have tachycardia with WPW?
Symptoms may also start and stop suddenly and occur at any age. Typical symptoms include: shortness of breath. a pounding in your chest. dizziness. passing out.
What is the procedure called when you have to go to the hospital for cardioversion?
This is called a Valsalva maneuver. Medication may stop or prevent tachycardia. If medication and the Valsalva maneuver do not work, you may need to go to the hospital for cardioversion. This procedure restores your heartbeat to a normal rhythm by passing an electric current through your chest into your heart.
What is the test for tachycardia?
If you have symptoms of tachycardia that come and go, your doctor will do a test called an electrocardiogram, or ECG . An ECG measures the electrical activity in your heart and your heart rate. If you are not having symptoms at the time of your ECG, results may look normal. Other tests may include:
Do you need to be treated if you don't have symptoms?
You may not need any treatment if you do not have symptoms, or if you have infrequent symptoms. Also, symptoms sometimes go away as people get older. If you do need treatment, there are several options:
What is WPW in ventricular preexcitation?
It is the most common type of ventricular preexcitation (preexcitation: the impulses travel to the ventricle earlier than what you would expect them to if they traveled down the normal pathway through the AV node). WPW occurs randomly in the general population, occurring in about 1 to 3 per 1,000 persons.
What is WPW in heart?
WPW is an electrical abnormality in the heart that may be associated with supraventricular tachycardia ( fast heart rate originating above the ventricles).
How to contact Miller Family Heart Vascular & Thoracic Institute?
If you need more information, click here to contact us, chat online with a nurse or call the Miller Family Heart, Vas cular & Thoracic Institute Resource & Information Nurse at 216.445.9288 or toll-free at 866.289.6911. We would be happy to help you.
How many people have WPW?
WPW occurs randomly in the general population, occurring in about 1 to 3 per 1,000 persons. In the general population, men have a higher incidence of WPW than women do, and there is a higher incidence of multiple accessory pathways in men. Some cases of WPW are inherited.
How do you know if you have WPW?
Symptoms of WPW may include one or more of the following: Heart palpitations – a sudden pounding, fluttering or. Racing feeling in your chest. Dizziness – feeling lightheaded or faint.
Why do you need to ablate a WPW?
How often and at what times to take them. Ablation - In people with WPW and symptoms of palpitations or syncope, an ablation procedure is recommended for two reasons: 1) to prevent symptom recurrence and 2) to prevent sudden cardiac death.
What is the accessory pathway?
When you have WPW, along with your normal conduction pathway, you have an extra pathway called an accessory pathway. They are normal heart muscle, not specialized electric tissue, and they may: Conduct impulses faster than normal. Conduct impulses in both directions.
How to treat WPW?
Short-term treatments. Short-term treatments for WPW include the following, and are usually administered sequentially in this order until symptoms are resolved: Maneuvers to slow the heart: These include massaging the sides of your neck or asking you to bear down to stimulate the vagus nerve.
Why do some people have WPW?
Having a family member with pre-excitation or WPW: This is because mutations in certain genes can cause WPW. Congenital heart defect: Some people who are born with a specific heart defect known as "Ebstein's anomaly" can develop WPW. This can occur if their mother was taking certain medications while she was pregnant.
How do you know if you have WPW?
The main symptoms of WPW include: A fluttering sensation in the chest: This occurs because the heart is beating faster than normal, and in some cases can have an irregular rhythm (arrhythmia). Dizziness or lightheadedness: This occurs because the heart is beating too fast to effectively pump blood to the brain.
What is the WPW in Buoy Chat?
Wolff-Parkinson-White (WPW) is a condition in which the heart beats abnormally fast due to electricity incorrectly traveling between pathways in the heart.
What medications slow the heart?
Medications to slow the heart: These include adenosine (Adenocard), verapamil (Calan), procainamide (Procan), or propranolol (Inderal), among others. The specific medication will vary depending on the type of abnormal rhythm you have. These medications can usually be stopped once the heart rhythm becomes normal.
What is the second pathway in the heart for electricity to be conducted called?
Having the second pathway in the heart for electricity to be conducted is also known as "pre-excitation" or "Wolff-Parkinson-White pattern.". It affects one to three people out of every 1,000.
When do symptoms of WPS start?
Symptoms usually first appear in teens or people in their 20s. People who have an extra conduction pathway ("pre-excitation") but have not developed WPS will not have any symptoms. However, if they develop WPW, they can experience symptoms that include the following.
Definition
Variations
- Treatment for Wolff-Parkinson-White (WPW) syndrome depends on the severity and frequency of symptoms and the type of heart rhythm problem (arrhythmia) causing the fast heart rate. The goals of treatment are to slow a fast heart rate when it occurs and to prevent future episodes. Treatment options for a fast heart rate include: 1. Vagal maneuvers.Si...
Classification
Types
Clinical significance
Mechanism
Cause
Specialist to consult
Epidemiology
Prognosis
Signs and symptoms
Pathophysiology
Significance
Locations
Advantages
Diagnosis
Treatment
Research
Risks
Symptoms
Assessment