Will a tooth abscess go away with just antibiotics?
When you are suffering from a tooth infection, you may want an easy solution, such as a course of antibiotics. However, antibiotics won't cure your tooth infection. Oral bacterial infections cause abscesses, which are small pockets of pus and dead tissue in the mouth.
What is the best treatment for a tooth abscess?
Depending on the type and severity of your abscess, treatment options include:Draining the abscess. Your dentist will make a small cut in the abscess to drain the pus. ... A root canal procedure. ... Tooth extraction. ... Antibiotics. ... Removal of foreign object.
How serious is an abscess tooth?
Tooth abscess is absolutely a dental emergency. If you have a tooth abscess, you need to seek treatment immediately. Left untreated, abscess can lead to infection that spreads through the body causing serious and even life-threatening effects. The sooner these issues are treated the better!
How can I get rid of an abscess without going to the dentist?
If your heart is set on avoiding the dentist though, below are six ways to get rid of a tooth abscess without going to the dentist.Saltwater Mouth Rinse. ... Rinse Your Mouth With Baking Soda. ... Use Oregano Essential Oil. ... Garlic Paste. ... Cold Compress With Ice. ... Aloe Vera Gel.
Can tooth abscess heal on its own?
A dental abscess is a build-up of pus in the teeth or gums caused by an infection. It needs urgent treatment by a dentist. A dental abscess will not go away on its own.
How long can a tooth abscess go untreated?
If left untreated, it may take a few more weeks or months for the infection to spread to other tissues and cause complications. However, once this has happened, death can occur quickly. Factors like older age, having diabetes, or being immunocompromised can increase your risk of complications from a dental abscess.
When should I worry about a tooth abscess?
A person who has a suspected tooth infection and develops any of these symptoms should seek immediate medical attention: painful tongue and mouth. swelling of the face, neck, and cheeks. itching or burning sensation on the skin.
What is an abscess tooth look like?
The raised swelling looks like a pimple near the affected tooth. An open pimple is called a "draining fistula" and has ruptured to release pus. This is an obvious sign of infection. Other signs of a tooth abscess are a bad taste or bad odor in the mouth.
What should I do to deal with a toothache?
Take an over-the-counter pain medication like ibuprofen or Tylenol. You can also wash your mouth out with some warm salt water. In general, you're...
Which type of antibiotic will get rid of abscesses?
Dentists usually use penicillin or amoxicillin which are active on a large spectrum of dental bacteria. When patients are allergic to penicillin yo...
Can an abscessed tooth cause excessive saliva?
It increases the flow but it is more of a sensation. When an abscessed tooth is influencing swallowing and making it painful, then you may feel an...
How to treat a tooth abscess?
Treatment options include: Incision and drainage: Your dentist makes a small incision (cut) in the abscess to drain the pus. Sometimes a small rubber drain is placed to keep the area open for drainage. Root canal: This option helps to eliminate the infection and save your tooth.
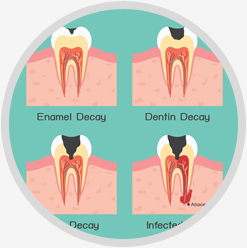
What is an abscess in a tooth?
A tooth abscess is a pocket of pus from a bacterial infection. Abscesses can occur in different places around a tooth for different reasons and affect the involved tooth, but also the surrounding bone and sometimes adjacent teeth. Three types of tooth infections can cause abscesses:
Why does a tooth abscess?
This occurs because bacteria can spread to the inside of the tooth to the pulp through a fracture or cavity. The pulp is the innermost part of the tooth that contains nerves and blood vessels. When bacteria invades the pulp, they can spread to the tip of the tooth’s root causing the infection to spread to the bone eventually leading to an abscess.
What are the three types of tooth infections?
Three types of tooth infections can cause abscesses: Gingival: This infection develops in the gums. It does not usually affect the tooth or supporting structures. Periapical: A periapical abscess is an infection that forms at the tip of the root.
What is the term for the infection of the gums around the teeth?
Broken, chipped or cracked teeth: Bacteria can seep into any opening in a tooth and spread to the pulp. Gum disease ( periodontitis ): Gum disease is an infection and inflammation of the tissues around the teeth.
What is gum disease?
Gum disease ( periodontitis ): Gum disease is an infection and inflammation of the tissues around the teeth. As gum disease progresses, the bacteria gain access to deeper tissues. Injury to the tooth: Trauma to a tooth can injure the inner pulp even if there’s no visible crack.
What is the best way to check for infection in a tooth?
In addition to examining the tooth and surrounding tissue for signs of infection, your dentist may: Recommend an X-ray. This can help identify sources of dental disease that may have led to the infection. Your dentist can also use X-rays to determine if the infection has spread and may be affecting other areas.
How to get rid of a tooth abscess?
Brush your teeth twice daily for 2 minutes with a fluoride toothpaste. Floss daily to clean hard-to-reach spots between your teeth and gums. Make a dentist appointment as soon as possible if you have a loose or cracked tooth. Limit sugary foods and drinks. Sweets and sodas lead to cavities, which can cause an abscess.
What is an abscess in dentistry?
By Rachel Duran. Medically Reviewed by Minesh Khatri, MD on November 23, 2019. An abscess is a pocket of pus that forms around the root of an infected tooth. Anyone, from children to the elderly, can get one. If you have one, it won’t get better on its own.
What is the best way to save a tooth?
Extraction. If the endodontist can’t save the tooth, it will have to come out. Root canal. You may have heard about this common way to treat an abscess. It’s the best way to save your tooth. The endodontist drills into your tooth and cleans the pulp from inside it and the root canals that go down into your gum.
What to do if your dentist can't diagnose an abscess?
If your dentist can’t diagnose the abscess on their own, they’ll probably send you to an endodontist, who’s specially trained to work on abscessed teeth. They can tell for sure if you have an abscess and treat it if you do.
How to get rid of an abscess in the jaw?
The goal is to get rid of the infection. To do that, the endodontist may try: Antibiotics . If the infection has spread past the abscess site to your jaw or farther into your body, you’ll probably get them. However, they won’t cure the abscess. Extraction.
What does it mean when you chew a tooth?
A bad odor when you chew with that tooth. Sometimes an abscess causes a pimple-like bump on your gum. If you press it and liquid oozes out, it’s a sure bet you have an abscessed tooth. That liquid is pus. If you have swelling in your face and a fever, or you have trouble breathing or swallowing, go to the emergency room.
How to tell if you have an abscess?
To find out if you have an abscessed tooth, your dentist probably will: Tap on your teeth. If you have an abscess, it’ll hurt when they touch the affected tooth. Take an X-ray. This can tell your dentist if you have an abscess and if it has spread to other parts of your mouth.
What is the procedure to fill a tooth with a root canal?
During a root canal, a dentist will drill into the tooth and remove the diseased pulp, completely sterilize the entire canal of the tooth, and then fill and seal the tooth's inner chambers and cap the tooth using a filling, inlay or even a crown when there is not enough dental substance.
What is an abscess in the UK?
The abscess is a pocket filled with pus caused by a bacterial infection that's developed in your damaged tooth.
How to tell if you have an abscess on your tooth?
Symptoms of a tooth abscess include fever, pain when chewing, a bad taste in the mouth, lingering bad breath, swollen neck glands, redness and swelling of the gums, discoloration of the tooth, swelling of the upper or lower jaw, or an open, pus-filled sore on the side of the gum.
What happens when you have an abscessed tooth?
It increases the flow but it is more of a sensation. When an abscessed tooth is influencing swallowing and making it painful, then you may feel an excess of saliva, but what actually happens is that the saliva stagnates on the lower jaw under the tongue.
How much does it cost to pull a tooth?
If you do not have dental insurance, try to find a free or reduced-cost dental clinic near you, and remember that any dentist should be able to simply pull your tooth for under $100.
How to treat an abscess that is not coming back?
Take all antibiotics that are prescribed by your doctor. Antibiotics are a critical part of the treatment for an abscess, and are necessary to ensure that the infection is completely gone and does not come back. They can also help to prevent severe pain, such as from a dry socket.
How long do you have to take antibiotics for a tooth infection?
You will need to take antibiotics for at least two days first to reduce the risk of bacteremia. Don't hesitate to go to the emergency room right away if you develop signs of major infection. They may not be able to fix your tooth, but the hospital is obligated to treat the infection, even if you don't have insurance.
How to treat an abscess in a tooth?
Depending on the type and severity of your abscess, treatment options include: 1 Draining the abscess. Your dentist will make a small cut in the abscess to drain the pus. They’ll follow up by cleaning the area with a saline solution. 2 A root canal procedure. A root canal involves drilling into the affected tooth to drain the abscess and remove any infected pulp. Next, your dentist will fill and seal the pulp chamber, which holds pulp, and the root canal. They may also cap your tooth with a crown to strengthen it. A crown procedure is usually done during a separate appointment. 3 Tooth extraction. If your tooth is too damaged, your dentist might remove it before draining the abscess. Your dentist may pull the tooth if it can’t be saved and then drain the abscess. 4 Antibiotics. If the infection has spread beyond the abscessed area or you have a weakened immune system, your dentist might prescribe oral antibiotics to help clear the infection. 5 Removal of foreign object. If your abscess is caused by a foreign object in your gums, your dentist will remove it. They’ll finish up by cleaning the area with a saline solution.
What is the procedure to remove an abscess from a tooth?
They’ll follow up by cleaning the area with a saline solution. A root canal procedure. A root canal involves drilling into the affected tooth to drain the abscess and remove any infected pulp. Next, your dentist will fill and seal the pulp chamber, which holds pulp, and the root canal.
What to do if you have an abscess and can't save it?
Your dentist may pull the tooth if it can’t be saved and then drain the abscess. Antibiotics. If the infection has spread beyond the abscessed area or you have a weakened immune system, your dentist might prescribe oral antibiotics to help clear the infection. Removal of foreign object.
What are the different types of dental abscesses?
The different types of dental abscesses depend on location. The three most common types are: Periapical abscess. This is an abscess at the tip of a tooth’s root. Periodontal abscess. This is an abscess on the gum next to the root of a tooth. It might also spread to the surrounding tissue and bone. Gingival abscess.
What is it called when you have a tooth that hurts?
It’s sometimes called a dental abscess. An abscessed tooth causes moderate to severe pain that can sometimes radiate to your ear or neck. Left untreated, an abscessed tooth can turn into a serious, life-threatening condition. Read on to learn more about the different types and how to recognize them.
What happens if you have an abscess ruptured in your jaw?
tooth sensitivity. discolored or loose teeth. bad breath. foul taste in your mouth. tender or swollen lymph nodes in your neck or under your jaw. fever. If an abscess ruptures, you’ll feel almost immediate pain relief. You might also notice a sudden bad taste in your mouth as the pus drains out.
What is the pulp of a tooth?
Bacteria enter the pulp within your teeth, usually through a cavity. Pulp refers to the soft, inner part of your tooth. This is made up of nerves, connective tissue, and blood vessels. Periodontal abscess. Gum disease usually causes this type, but it can also be the result of an injury. Gingival abscess.
How to prevent tooth decay?
Get a new toothbrush every 3 or 4 months or when the bristles on the one you’re using look frayed. Use an antiseptic or fluoride mouth rinse to help prevent tooth decay. Drink fluoridated water.
What is the term for a tooth infection that doesn't go away on its own?
Bhargava, MD on August 17, 2020. When bacteria gets into the root of a tooth, it can cause a buildup of pus. This kind of infection is called an abscessed tooth , or a periapical abscess. These infections don’t go away on their own, so it’s important to see your dentist if you think you have ...
How to stop a tooth from hurting when you brush it?
Take over-the-counter pain relievers like aspirin, ibuprofen, or naproxen for the discomfort. Try to chew on the side of your mouth away from the tooth. When you brush your teeth, use a toothbrush with soft bristles. Don’t eat foods that are hot or cold. Put a cold compress on your jaw where your tooth hurts.
How to get toothpaste off your teeth?
Brush with fluoride toothpaste twice a day for at least 2 minutes each time. Don’t rinse your mouth with mouthwash or water immediately after brushing -- that can take the protective toothpaste off your teeth. Floss at least once a day to clean between your teeth and under your gums.
What to do if you have an abscess in your tooth?
If you have an abscessed tooth, your dentist may recommend one of the following treatments, depending on how serious the abscess is: If you have a simple abscess, your dentist, or a specialist called an endodontist, can do a root canal to get rid of the infection and hopefully save the tooth.
What to do after a tooth is sealed back up?
After the tooth is sealed back up, your dentist can then put on a cap, or crown, as a top layer to protect the tooth and make sure you don’t get another abscess. If your tooth can’t be saved, your dentist might need to pull it, then drain the abscess to get rid of the infection.
How to prevent abcess from teeth?
Dental abscess prevention tips include: Brush your teeth twice a day with fluoride toothpaste. You can either use a regular or electric toothbrush. Replace your toothbrush or toothbrush head every 3 to 4 months. Floss between your teeth daily with dental floss, floss sticks, or a water flosser.
Why do I have tooth abscesses?
The long-term build-up of pus inside the gums or teeth triggers an abscess, which forms due to a bacterial infection. The infection affects the surrounding structures of teeth and can cause persistent toothaches and other symptoms. There are three main types of oral abscesses that can form in different regions around a tooth, including:
What is a periodontal abscess?
Periodontal Abscess. A periodontal abscess is a localized pocket of pus that forms in the tissues of the periodontium (gums). This abscess appears as a shiny, smooth swelling that protrudes out of the gums and is sensitive to the touch. The tooth or teeth around the abscess may also become sensitive or loosen.
How to tell if you have an abscess?
Depending on the type of dental abscess and how long it has been progressing, common symptoms may include: 1 Severe toothache and throbbing near the affected tooth. This can include the gums, tooth root, or the tooth directly. The pain typically comes and goes suddenly 2 Painful, swollen lymph nodes in the neck and/or jaw 3 Redness, swelling, and inflammation near the abscess 4 Swollen, inflamed, and shiny gums 5 Pain that worsens when lying down and interrupts sleep 6 Tooth sensitivity to cold, sweet, or hot substances 7 Consistent bad breath, even after brushing or rinsing the mouth 8 A loose tooth or multiple loose teeth near the infection site 9 Severe ear, neck, and/or jaw pain 10 Pain when biting down or chewing 11 Difficulties swallowing and breathing 12 Face swelling 13 Fever
What is the pain of an abscess?
SUMMARY. A tooth abscess is a painful pocket of pus that develops from a bacterial infection in the mouth. There are three types: gingival, periodontal, and periapical abscesses.
What is the cause of a gingival abscess?
The most common cause of a gingival abscess is from the impact of a foreign object, such as popcorn, a toothpick splinter, or shellfish fragments.
When is root canal therapy necessary?
Root canal treatment is typically necessary when a tooth becomes heavily decayed and the bacteria spreads to the dental pulp and teeth roots. If there is also an abscess at the root of a tooth (periapical abscess), root canal therapy is typically necessary.
What is the best oil to use for an abscessed tooth?
Oregano oil is an antibacterial and antioxidant. It may help reduce the swelling and pain of an abscessed tooth. Be sure to dilute any essential oil with a carrier oil to prevent further irritation. Here’s how to choose a carrier oil.
How to make a mouthwash with baking soda?
Mix 1/2 tablespoon of baking soda with 1/2 cup of water and a pinch of salt. Swish the mixture in your mouth for up to five minutes. Spit out, and repeat until you’ve finished the mixture. You can repeat this up to two times per day.
How to get rid of a swollen mouth?
To use this remedy: Mix 1/2 teaspoon of normal table salt with 1/2 cup of warm tap water. Rinse your mouth with the salt water. Try to swish it around inside your mouth for at least two minutes. Spit the water out. Repeat up to three times per day.
How to treat an abscess in the gums?
If not treated, the infection could spread to the gums and bone of the mouth. A tooth abscess should be treated by a dentist, but some home remedies can relieve the discomfort caused by the infection. The following home remedies can be applied along with prescribed treatments. 1. Saltwater rinse.
How to treat a swollen ear?
To use this remedy: Make a fenugreek tea by heating 1 cup of water in a saucepan and stirring in 1 teaspoon of ground fenugreek. Allow the mixture to cool. Apply a small amount to the affected area using a cotton ball. Repeat up to three times per day.
What to do if you have an abscess on your face?
If you have a tooth abscess, see a doctor immediately and a dentist as soon as possible. The home remedies listed above are meant as complementary treatments to the ones prescribed by a doctor.
What is the best way to heal a wound?
This may be repeated multiple times per day. 5. Fenugreek tea . Fen ugreek has antibacterial properties and a long history of use as a home remedy for healing wounds and reducing inflammation. It may be available in the spice aisle of your supermarket or online.
How to treat an abscess in a tooth?
Dentists will treat a tooth abscess by draining it and getting rid of the infection. They may be able to save your tooth with a root canal treatment, but in some cases the tooth may need to be pulled. Leaving a tooth abscess untreated can lead to serious, even life-threatening, complications.
What are the risks of tooth abscess?
Risk factors. These factors may increase your risk of a tooth abscess: Poor dental hygiene. Not taking proper care of your teeth and gums — such as not brushing your teeth twice a day and not flossing — can increase your risk of tooth decay, gum disease, tooth abscess, and other dental and mouth complications. A diet high in sugar.
How to tell if you have an abscess?
Signs and symptoms of a tooth abscess include: 1 Severe, persistent, throbbing toothache that can radiate to the jawbone, neck or ear 2 Sensitivity to hot and cold temperatures 3 Sensitivity to the pressure of chewing or biting 4 Fever 5 Swelling in your face or cheek 6 Tender, swollen lymph nodes under your jaw or in your neck 7 Sudden rush of foul-smelling and foul-tasting, salty fluid in your mouth and pain relief, if the abscess ruptures 8 Difficulty breathing or swallowing
What is a periapical tooth?
Periapical tooth abscess. Periapical tooth abscess. Bacteria can enter the innermost part of the tooth through either a deep cavity or a chip or crack in your tooth. The resulting infection and inflammation can cause an abscess at the tip of the root. A tooth abscess is a pocket of pus that's caused by a bacterial infection.
What causes periapical abscess?
Causes. A periapical tooth abscess occurs when bacteria invade the dental pulp — the innermost part of the tooth that contains blood vessels, nerves and connective tissue. Bacteria enter through either a dental cavity or a chip or crack in the tooth and spread all the way down to the root. The bacterial infection can cause swelling ...
How do you know if you have an abscess on your jaw?
Sensitivity to hot and cold temperatures. Sensitivity to the pressure of chewing or biting. Fever. Swelling in your face or cheek. Tender, swollen lymph nodes under your jaw or in your neck.
What does it feel like to have an abscess in your neck?
Tender, swollen lymph nodes under your jaw or in your neck. Sudden rush of foul-smelling and foul-tasting, salty fluid in your mouth and pain relief, if the abscess ruptures. Difficulty breathing or swallowing.
Overview
- A tooth abscess is a pocket of pus that's caused by a bacterial infection. The abscess can occur at different regions of the tooth for different reasons. A periapical (per-e-AP-ih-kul) abscess occurs at the tip of the root, whereas a periodontal (per-e-o-DON-tul) abscess occurs in the gums at the side of a tooth root. The information here refers specifically to periapical abscesses.A per…
Treatment
- The goal of treatment is to get rid of the infection. To accomplish this, your dentist may: 1. Open up (incise) and drain the abscess. The dentist will make a small cut into the abscess, allowing the pus to drain out, and then wash the area with salt water (saline). Occasionally, a small rubber drain is placed to keep the area open for drainage while the swelling decreases. 2. Perform a roo…
- The treatment of a periapical abscess varies according to the extent, location, severity and duration of the abscess. The available tooth structure is also a chief factor in determining the treatment plan. A periapical dental x-ray is a must to determine the diagnosis as the lesion is similar to infected periapical granuloma or an infected dental cyst.
Complications
- An undiagnosed or untreated periapical abscess can lead to complications. 1. A chronic periapical abscess can lead to dental cyst formation or diseases such as osteomylitis. 2. In certain circumstances such as in immune compromised patients, the abscess can spread to vital organs. 3. The abscess can lead to a condition called as Ludwig’s angina, characterized by cellulitis invol…
- A tooth abscess won't go away without treatment. If the abscess ruptures, the pain may decrease significantly — but you still need dental treatment. If the abscess doesn't drain, the infection may spread to your jaw and to other areas of your head and neck. You might even develop sepsis — a life-threatening infection that spreads throughout your body.If you have a weakened immune sys…
Signs And Symptoms
- A small periapical abscess may be asymptomatic apart from the history of tooth decay and pain associated with the decay itself. In most cases a dental abscess is associated with intense pain. The pain is often described as throbbing and sharp shooting in nature. The tooth becomes tender on pressure application and chewing from the affected side becomes difficult. The affected toot…
- Signs and symptoms of a tooth abscess include: 1. Severe, persistent, throbbing toothache that can radiate to the jawbone, neck or ear 2. Sensitivity to hot and cold temperatures 3. Sensitivity to the pressure of chewing or biting 4. Fever 5. Swelling in your face or cheek 6. Tender, swollen lymph nodes under your jaw or in your neck 7. Sudden rush of foul-smelling and foul-tasting, salt…
Diagnosis
- In addition to examining your tooth and the surrounding area, your dentist may: 1. Tap on your teeth. A tooth that has an abscess at its root is generally sensitive to touch or pressure. 2. Recommend an X-ray. An X-ray of the aching tooth can help identify an abscess. Your dentist may also use X-rays to determine whether the infection has spread, causing abscesses in other area…
Lifestyle And Home Remedies
- While the area is healing, your dentist may recommend these steps to help ease discomfort: 1. Rinse your mouth with warm salt water. 2. Take over-the-counter pain relievers, such as acetaminophen (Tylenol, others) and ibuprofen (Advil, Motrin IB, others), as needed.
Causes
- The bacteria involved in formation of periapical abscess include Streptococcus viridians, Prevotella and Fusobacterium. These infections are more likely to arise in cases of tooth decay and dental cavity formation. Here the bacteria gain entry through the opening to the mouth. However, sometimes the bacteria may reach the site via the bloodstream.
- A periapical tooth abscess occurs when bacteria invade the dental pulp — the innermost part of the tooth that contains blood vessels, nerves and connective tissue.Bacteria enter through either a dental cavity or a chip or crack in the tooth and spread all the way down to the root. The bacterial infection can cause swelling and inflammation at the tip of the root.
Prevention
- Avoiding tooth decay is essential to preventing a tooth abscess. Take good care of your teeth to avoid tooth decay: 1. Use fluoridated drinking water. 2. Brush your teeth at least twice a day with a fluoride toothpaste. 3. Use dental floss or an interdental cleaner to clean between your teeth on a daily basis. 4. Replace your toothbrush every three or four months, or whenever the bristles are f…
Risk Factors
- These factors may increase your risk of a tooth abscess: 1. Poor dental hygiene. Not taking proper care of your teeth and gums — such as not brushing your teeth twice a day and not flossing — can increase your risk of tooth decay, gum disease, tooth abscess, and other dental and mouth complications. 2. A diet high in sugar. Frequently eating and drinking foods rich in su…