Medication
Pericarditis can recur on the withdrawal of NSAID therapy. Generally, we recommend taking "treatment dose" for one to two weeks or until complete symptom resolution. After that, the NSAID dosing should be tapered in an attempt to reduce the subsequent risk of recurrence.
Procedures
Treatment will depend on type of pericarditis you have, and may include:
- non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling
- antibiotics, if there is a bacterial infection
- colchicine, a prescription-only medicine often used for recurring pericarditis
- painkillers
How long should a take naproxin for pericarditis?
The patients were masked for the treatment but not the physicians ... gastrointestinal tract, liver hilum, pericardium, diaphragm, and major vessels (larger than 3 mm) 31. Three radiologists (AR, AZ and JS) with 5–10 years of experience in ...
What is pericarditis and how is it treated?
You may need one or more tests, such as:
- Chest X-ray to see the size of your heart and any fluid in your lungs.
- Electrocardiogram (ECG or EKG) to look for changes in your heart rhythm. ...
- Echocardiogram (echo) to see how well your heart is working and check for fluid or pericardial effusion around the heart. ...
Is there a cure for pericarditis?
How can one prevent a recurrence of pericarditis?

How long does it take for pericarditis to get better?
Most people recover in 2 weeks to 3 months. However, pericarditis may come back. This is called recurrent, or chronic, if symptoms or episodes continue. Scarring and thickening of the sac-like covering and the heart muscle may occur when the problem is severe.
What is the treatment for acute pericarditis?
Acute pericarditis should be treated with a nonsteroidal anti-inflammatory drug (NSAID), typically with a 2- to 4-week taper after the resolution of symptoms. In addition, a 3-month course of colchicine (with weight-adjusted dosing) is recommended to reduce the risk of recurrent pericarditis.
What is the best anti-inflammatory for pericarditis?
Nonsteroidal antiinflammatory drugs — For nearly all patients with acute idiopathic or viral pericarditis, we recommend NSAIDs (in combination with colchicine) as the initial treatment (algorithm 1).
Do anti inflammatories help pericarditis?
For patients with idiopathic or viral pericarditis, therapy is directed at symptom relief. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the mainstay of therapy. These agents have a similar efficacy with relief of chest pain in about 85-90% of patients within days of treatment.
How long does pain from pericarditis last?
Incessant pericarditis lasts about four to six weeks but less than three months. The symptoms are continuous. Chronic constrictive pericarditis usually develops slowly and lasts longer than three months.
How long does it take colchicine to work for pericarditis?
Addition of colchicine to standard therapy results in earlier reduction in pericarditis symptoms, greater remission at 1 week, and reduces the rate of recurrent pericarditis.
Does prednisone help pericarditis?
Abstract. Background— Corticosteroid use is widespread in recurrent pericarditis, even if rarely indicated, and high doses (eg, prednisone 1.0 to 1.5 mg · kg−1 · d−1) are generally recommended, although only weak evidence supports their use with possible severe side effects.
How long do you take NSAIDs for pericarditis?
Appropriate therapy for acute idio- pathic pericarditis is an NSAID for ≈2 weeks, and it is also reasonable to pre- scribe colchicine for up to 3 months (the duration used in clinical trials), espe- cially to reduce the rate of recurrence.
What does colchicine do for pericarditis?
Colchicine is an anti-inflammatory agent that works by inhibiting tubulin polymerization, thereby interfering with migration and phagocytosis and reducing the inflammatory cycle. For acute pericarditis, colchicine is generally used in combination with other therapies.
Does omeprazole help pericarditis?
As with all NSAID use, GI prophylaxis should be strongly recommended. Gastroprotection with misoprostol (600 to 800 g/day) or omeprazole (20 mg/day) is highly recommended.
Should I rest with pericarditis?
It's important to get plenty of rest. Don't do any strenuous activity for a few weeks, until your pericarditis has gone and your heart is back to normal. This will help to reduce your risk of low blood pressure and abnormal heart rhythms.
How do you get rid of fluid around the heart?
Pericardiocentesis is a procedure done to remove fluid that has built up in the sac around the heart (pericardium). It's done using a needle and small catheter to drain excess fluid. A fibrous sac known as the pericardium surrounds the heart.
What is the best treatment for pericarditis?
Examples include: Pain relievers. Pericarditis pain can usually be treated with over-the-counter pain relievers, such as aspirin or ibuprofen (Advil, Motrin IB, others). Prescription-strength pain relievers also may be used.
What is the purpose of a pericarditis test?
The test can be used to look for thickening that may be a sign of constrictive pericarditis. Your doctor may order this test to rule out other causes of sudden chest pain, such as a blood clot in a lung (pulmonary embolus) or a tear in your aorta (aortic dissection). Cardiac magnetic resonance imaging (MRI).
What is the sound of pericarditis?
During the exam, the doctor will place a stethoscope on your chest to listen to your heart sounds. Pericarditis causes a specific sound, called a pericardial rub. The noise occurs when the two layers of the sac surrounding your heart (pericardium) ...
What is the procedure to remove fluid from the heart?
Treatments include: Pericardiocentesis. In this procedure, a doctor uses a sterile needle or a small tube (catheter) to remove and drain the excess fluid from the pericardial cavity.
What is the best medicine for pericarditis?
Stronger medicine may be needed if the pain is severe. Your doctor may prescribe a medicine called colchicine and a steroid called prednisone . If a bacterial infection is causing your pericarditis, your doctor will prescribe an antibiotic or other medicine.
How long does it take for pericarditis to go away?
Some cases, if not treated, can lead to chronic pericarditis and serious problems that affect your heart. It can take weeks or months to recover from pericarditis.
How is tamponade treated?
Cardiac tamponade is treated with a procedure called pericardiocentesis, in which a needle or tube, called a catheter, is inserted into the chest wall to remove excess fluid in the pericardium. Additional procedures may also be needed to extract the fluid from around the heart. This relieves pressure on the heart.
What are the goals of treatment?
The goals of treatment include: Reducing pain and inflammation. Treating the underlying cause, if it's known. Checking for complications.
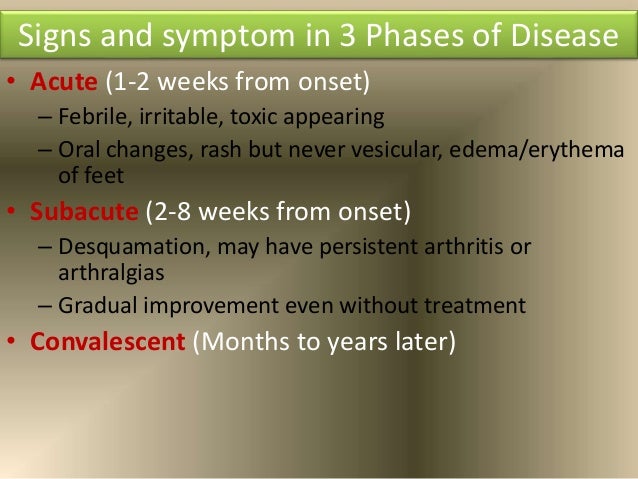
How long does pericarditis last?
The task force suggests that the term 'acute' should be adopted for new-onset pericarditis, 'incessant' for pericarditis with symptoms persisting for four to six weeks, and 'chronic' for pericarditis lasting more than three months [3]. Recurrent pericarditis is diagnosed with a documented first episode of acute pericarditis, a symptom-free interval of four to six weeks or longer and evidence of subsequent recurrence of pericarditis. The recurrence rate after an initial episode of pericarditis ranges from 15 to 30%, and may increase to 50% after a first recurrence in patients not treated with colchicine, particularly if treated with corticosteroids [15].
When should low dose corticosteroids be considered?
Low-dose corticosteroids should be considered in cases of contraindications/failure of aspirin/NSAIDs and colchicine, and when an infectious cause has been excluded, or when there is a specific indication such as autoimmune disease. Serum CRP guides the treatment length and response to therapy. Topic (s):
Can pericardial effusions recur?
Purulent pericardial effusions are likely to recur [1]. Surgical drainage with construction of a window is often needed. In patients with thick, purulent effusions and dense adhesions, extensive pericardiectomy may be required to achieve adequate drainage and to prevent the development of constriction. Early surgical drainage may also help prevent late constriction. Intrapericardial streptokinase has been administered to selected patients with purulent or loculated effusions and may obviate the need for a window [9]. The prognosis of bacterial pericarditis is poor with survival in the range of 30%, even in modern series [3].
Is pericarditis a disease?
Bacterial pericarditis is relatively uncommon in clinical practice in developed countries with a low prevalence of TB. Tuberculous pericarditis is the most common form all over the world and the most common cause of pericardial diseases in developing countries [1].
Is pericarditis a prognosis?
Most patients with acute pericarditis (generally those with presumed viral or idiopathic pericarditis) have a good long-term prognosis [6]. Cardiac tamponade rarely occurs in patients with acute idiopathic pericarditis, and is more common in patients with a specific underlying aetiology, such as malignancy, TB or purulent pericarditis. The risk of developing constriction can be classified as low (1%) for idiopathic and presumed viral pericarditis, intermediate (2-5%) for autoimmune, immune-mediated and neoplastic aetiologies, and high (20-30%) for bacterial aetiologies, especially with TB and purulent pericarditis. Approximately 15-30% of patients with idiopathic acute pericarditis who are not treated with colchicine will develop either recurrent or incessant disease, while colchicine may halve the recurrence rate. The proposed triage of acute pericarditis according to epidemiological background and predictors of poor prognosis is presented in Figure 1 [3].
Is pericarditis a self-limiting disease?
Acute pericarditis is a self-limiting disease without significant complications or recurrences in 70% to 90% of patients. If the laboratory data support the clinical diagnosis, symptomatic treatment with aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) with gastroprotection should be initiated. Colchicine is recommended first-line therapy ...
Can corticosteroids be used for pericarditis?
Corticosteroids are not recommended as first-line therapy for acute peri carditis as they appear to encourage recurrences. Serum CRP should be considered to guide the treatment length and assess the response to therapy. Evaluation of response to anti-inflammatory therapy is recommended after one week.
What is the best pain reliever for pericarditis?
This can minimize pain and inflammation until the pericarditis subsides. Anti-inflammatory pain relievers such as aspirin and ibuprofen are most often used to ease the discomfort of pericarditis.
How do you know if you have pericarditis?
Most pericarditis attacks come on quickly and do not usually last long. The most common symptom is a sharp, stabbing chest pain that may be in the middle or left side of your chest. The pain may also be in one or both shoulders or feel like a heart attack.
What is the swelling of the pericardium?
Pericarditis is swelling or inflammation of the pericardium, which is the two thin sac-like layers of tissue surrounding the heart. The pericardium holds the heart in place and helps it function properly. [1]
What to do if you have a severe pain?
Take prednisone. If your pain is especially severe, your doctor may prescribe you prednisone, which is a steroid medication. [12] X Trustworthy Source National Heart, Lung, and Blood Institute Research and education center within the National Institutes of Health Go to source.
Does pericarditis cause chest pain?
Pericarditis usually causes chest pain, which may be sharp, when these two layers rub against each other. The pain of pericarditis often begins suddenly and doesn’t last long. [2] In most cases, pericarditis is mild and clears up on its own.
What is pericarditis management?
● In cases of pericarditis due to an identifiable cause (eg, bacterial infection or malignancy), management is focused upon the underlying disorder and, if necessary, drainage of an associated pericardial effusion. (See 'Treatment' above.)
What are the risk factors for recurrent pericarditis?
Risk factors for recurrent pericarditis include lack of response to nonsteroidal anti-inflammatory drugs, the need for corticosteroid therapy, and creation of a pericardial window. The pathogenesis, course, and treatment of recurrent pericarditis are discussed separately. (See "Recurrent pericarditis" .)
What percentage of patients with pericarditis are not treated with colchicine?
Approximately 15 to 30 percent of patients with idiopathic acute pericarditis who are not treated with colchicine develop either recurrent or incessant disease. Immune mechanisms appear to be of primary importance in the majority of cases, and the term "chronic autoreactive" pericarditis has been used.
What is the pericardium made of?
The pericardium is a fibroelastic sac made up of visceral and parietal layers separated by a (potential) space, the pericardial cavity. In healthy individuals, the pericardial cavity contains 15 to 50 mL of an ultrafiltrate of plasma. Diseases of the pericardium present clinically in one of several ways:
Can glucocorticoids be used for pericarditis?
Glucocorticoids — Glucocorticoids should be used for initial treatment of acute pericarditis only in patients with contraindications to NSAIDs, or for specific indications (ie, systemic inflammatory diseases, pregnancy, and possibly renal failure), and should be used at the lowest effective dose.
Does colchicine help with pericarditis?
While the majority of patients have prompt resolution of symptoms without recurrent pericarditis when treated with NSAIDS alone, colchicine, when used as an adjunct to NSAID therapy, reduces symptoms, decreases the rate of recurrent pericarditis, and is generally well tolerated.
Can you take NSAIDs with aspirin?
The use of NSAIDs other than aspirin should be avoided, since anti-inflammatory therapy may impair scar formation [ 19 ]. Aspirin may also be the first choice in patients who require concomitant antiplatelet therapy for any reason. With either regimen, gastrointestinal protection should be provided.
How long does it take for pericarditis to recur?
Finally, the recurrent form of pericarditis is a recurrence after the first episode of pericarditis and a symptom free interval of 4 to 6 weeks or longer, 10 such as the patient in our clinical vignette. The primary aim of treatment is the resolution of pain and inflammation and consists ...
How long does pericarditis last?
The incessant form occurs when symptoms last for about 4-6 weeks but less than 3 months without remission. The chronic form occurs once symptoms exceed three months. Finally, the recurrent form of pericarditis is a recurrence after ...
What is the most common etiology of pericarditis?
In the developed world, the most common etiology is idiopathic or viral, 7 whereas in the developing world tuberculosis is the leading cause. 8 The diagnosis of pericarditis is based on a constellation of clinical symptoms, physical exam, ECG changes, laboratory abnormalities, and imaging findings.
How to heal pericarditis?
Any form of stress on the body, including intense physical exercise, can make your pericarditis flare up. If you’ve been diagnosed with pericarditis you should make sure that you get plenty of rest in order to allow your body to heal. Get at least seven to nine hours of sleep at night and relax during the day.
What is the best home remedy for pericarditis?
Bentonite clay is another great home remedy for pericarditis that helps by building up your body’s defense against viruses and other infections. This helps to improve your overall health and reduce inflammation, thus protecting your heart from pericarditis.
How to treat pericarditis with coconut oil?
Oregano oil helps to protect your body from viruses, bacterial and fungal infections which might otherwise make your pericarditis worse. mix two drops of oregano oil with a teaspoon of coconut oil and consume once a day.
How to treat pericarditis with apple cider vinegar?
Add a tablespoon of apple cider vinegar to a glass of water and drink it before each meal (or whenever your experience a pericarditis attack). This will help to reduce your chest pain and other symptoms.
What age is pericarditis most common?
Age and gender are common risk factors for developing pericarditis as its most common in men between the ages of sixteen and sixty. It’s also more common in people with a history of heart disease or bacterial/viral infection.
What causes chest pain?
Another heart condition that can cause chest pain is called pericarditis. Luckily, home remedies for pericarditis do exist and can help. Pericarditis can cause are sharp pains in your chest and make it difficult to breathe. Pericarditis is caused by inflammation of the sac that holds the heart and is found in around 5 percent ...
How to protect your heart from pericarditis?
Consuming the extract from grapefruit seeds is another great way to protect your heart from pericarditis. Try consuming just a small amount each day and you should notice your condition start to improve.
Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Preparing For Your Appointment
Keywords
- Treatment for pericarditis depends on the cause and the severity of the symptoms. Mild pericarditis may get better without treatment.
Introduction
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
General Recommendations, Physical Activity and Lifestyle Changes
- For mild pericarditis, rest and over-the-counter pain medications — taken as directed by your care provider — may be all that's needed. While you recover, avoid strenuous physical activity and competitive sports. Such activity can trigger pericarditis symptoms. Ask your health care provider how long you need to rest.
Prognosis
- You're likely to start by seeing a primary care provider or an emergency room doctor. You may be referred to a doctor trained in heart conditions (cardiologist). Here's some information to help you prepare for your appointment.
Pharmacologic Therapy For Acute Pericarditis
Management of Incessant and Recurrent Pericarditis
Management of Specific Forms of Acute Pericarditis
Conclusion