
Medication
- sit comfortably in your seat and lie back as much as possible
- wear loose-fitting clothing
- make sure you have plenty of leg room
- drink water regularly
- take regular breaks from sitting
- bend and straighten your legs, feet and toes every 30 minutes while seated
- press the balls of your feet down hard against the floor every so often
- wear flight socks
Procedures
Results: For a selected group of patients with acute, symptomatic pulmonary embolism, home treatment is as safe and effective as hospital treatment. PESI (Pulmonary Embolism Severity Index) and Hestia criteria have the best documented clinical utility for selection of patients for home treatment. Interpretation: The Hestia criteria represent a pragmatic approach to selection of patients who can be treated at home for pulmonary embolism, and they can be applied without taking other formal ...
Therapy
Pulmonary embolism (PE) is a common and potentially deadly form of venous thromboembolic disease. It is the third most common cause of cardiovascular death and is associated with multiple inherited and acquired risk factors as well as advanced age.
Nutrition
Thrombolytic treatment accelerates the dissolution of thrombus in acute pulmonary thromboembolism (PTE) and is potentially a lifesaving treatment. High-risk PTE is the clearest indication for this therapy, and its use in intermediate-risk cases is still controversial.
See more
How to diagnose and treat pulmonary embolism?
Can patients with pulmonary embolism be treated at home?
Is pulmonary embolism a deadly disease?
Is thrombolytic therapy effective for pulmonary embolism?

Which is the treatment of choice for pulmonary embolism?
Blood thinners (anticoagulants). Heparin is a frequently used anticoagulant that can be given through the vein or injected under the skin. It acts quickly and is often overlapped for several days with an oral anticoagulant, such as warfarin, until it becomes effective, which can take days.
What is the first stage of treatment for pulmonary embolism?
A first step in treating most embolisms is to treat shock and provide oxygen therapy. Anticoagulant medications, such as heparin, enoxaparin, or warfarin are usually given to help thin the blood and prevent further clotting.
How do they treat pulmonary embolism in hospital?
Depending on your medical condition, treatment options may include anticoagulant (blood-thinner) medications, thrombolytic therapy, compression stockings, and sometimes surgery or interventional procedures to improve blood flow and reduce the risk of future blood clots.
How serious is acute pulmonary embolism?
An acute pulmonary embolism can be life-threatening, so people who experience these symptoms should seek immediate medical attention. The condition can also lead to pulmonary hypertension, which is high blood pressure in the lungs and right side of the heart.
How long does it take a pulmonary embolism to dissolve?
A DVT or pulmonary embolism can take weeks or months to totally dissolve. Even a surface clot, which is a very minor issue, can take weeks to go away. If you have a DVT or pulmonary embolism, you typically get more and more relief as the clot gets smaller.
What is the survival rate of a pulmonary embolism?
A pulmonary embolism (PE) is a blood clot in the lungs, which can be serious and potentially lead to death. When left untreated, the mortality rate is up to 30% but when treated early, the mortality rate is 8%. Acute onset of pulmonary embolism can cause people to die suddenly 10% of the time.
Can you make a full recovery from pulmonary embolism?
Most people will make a full recovery after a pulmonary embolism and do not experience long-term complications. However, some people develop: post-thrombotic syndrome, which causes swelling, pain, and skin discoloration.
How urgent is a pulmonary embolism?
A pulmonary embolism (PE) is the most serious form of venous disease. It happens when a blood clot from deep within the body breaks free and travels to the lung. PE is a medical emergency that requires immediate attention.
Should I be in hospital with a pulmonary embolism?
A blood clot in the lungs is called a pulmonary embolism or PE. This requires immediate medical attention since it can cause death.
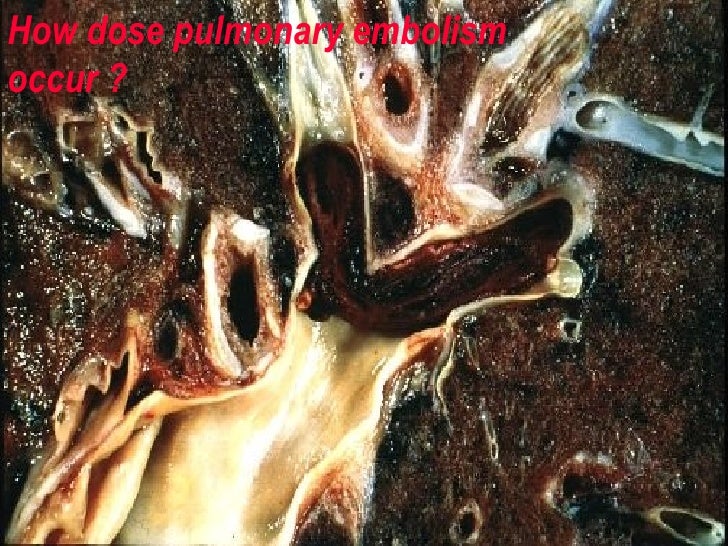
How do you get acute pulmonary embolism?
In most cases, pulmonary embolism is caused by blood clots that travel to the lungs from deep veins in the legs or, rarely, from veins in other parts of the body (deep vein thrombosis). Because the clots block blood flow to the lungs, pulmonary embolism can be life-threatening.
Which of the following patients is at the highest risk for a pulmonary embolism?
People at risk for PE are those who: Have been inactive or immobile for long periods of time. Have certain inherited conditions, such as blood clotting disorders or factor V Leiden. Are having surgery or have broken a bone (the risk is higher weeks following a surgery or injury).
What are the symptoms of acute pulmonary embolism?
What are the symptoms of a pulmonary embolism?Sudden shortness of breath (most common)Chest pain (usually worse with breathing)A feeling of anxiety.A feeling of dizziness, lightheadedness, or fainting.Irregular heartbeat.Palpitations (heart racing)Coughing and/or coughing up blood.Sweating.More items...
What is the best treatment for acute PE?
Anticoagulation therapy is the primary treatment option for most patients with acute PE. The utilization of factor Xa antagonists and direct thrombin inhibitors, collectively termed Novel Oral Anticoagulants (NOACs) are likely to increase as they become incorporated into societal guidelines as first line therapy. 38 Adoption of these newer agents may mitigate the major limitation of VKA therapy, frequently found in studies of VTE/PE to have sub-therapeutic INRs in a significant number of patients. 50 Low molecular weight heparin is superior to unfractionated heparin in both treatment and thrombo-prophylaxis in cancer patients. 27,51 This is reflected in the recommendations made by the American College of Chest Physicians who recommend the use of low molecular weight heparin on the basis of the strength of evidence available. 38 The importance of prompt initiation of anticoagulation cannot be over emphasized; objective assessment of bleeding risk, set in the context of the risk of choosing not to use anticoagulation, should prevent overly conservative practices founded upon theoretical concerns over bleeding.
What are the key considerations for endovascular care?
Three key considerations should be factored into the decision to proceed with an endovascular approach : 1) disease severity and acuity; 2) likelihood of a major adverse bleeding event; and 3) patient-specific considerations.
How long should antiplatelet therapy be after a stenting?
There are no comparative studies or societal recommendations to suggest the type, dose and duration of anticoagulation therapy or antiplatelet therapy following catheter based endovascular therapies with or without angioplasty and stenting. Current recommendations suggest therapy based on VTE stratification: 1) VTE associated with reversible risk factor or "provoked" DVT (at least 3 months); 2) unprovoked or recurrent VTE (6 to 12 months); and 3) VTE in the setting of cancer (indefinitely with LMWH). Similarly, no guidelines exist for the type or duration of antiplatelet therapy in this setting. We have adopted an empiric approach to anticoagulation and antiplatelet therapy in patients who have undergone CDT and/or venous stenting. Following the completion of CDT for either acute DVT or PE we resume anticoagulation with unfractionated heparin soon after puncture site hemostasis has been achieved. We then transition patients onto NOAC or VKA therapy, following a patient-centered discussion. Patients who have undergone stenting are also commenced on low dose aspirin and clopidogrel. We adopt this aggressive approach especially in patients with chronic VTE who have high rates of re-thrombosis and often require further intervention in up to 40% of cases within 4 years. 87 Finally, in patients with LE-DVT we utilize compression bandages until there is resolution of acute swelling and then switch to knee-high compression stockings with 30-40 mmHg pressure. Patients are followed up at regular intervals following discharge, at which time clinical assessment is made for disease recurrence, changes in quality of life as well as continued careful review of their bleeding risk on anticoagulation therapy.
How many people die from venous thromboembolic disease annually?
Venous thromboembolic disease (VTE) is estimated to occur in at least 1 to 2 persons per 1000 population annually, manifesting as deep vein thrombosis (DVT), pulmonary embolism (PE) or in combination. 1-3 It is the cause of over 100,000 deaths annually and is the most preventable cause of death in hospitalized patients in the United States. 4 Despite treatment with anticoagulant therapy, a significant proportion of survivors of acute DVT or PE are at risk of suffering from the disabling sequelae such as the post thrombotic syndrome (PTS), recurrent VTE or chronic thromboembolic pulmonary hypertension (CTEPH). 1,5 Given the limitations of medical therapy, promising endovascular treatment modalities have evolved over the past two decades in an effort to mitigate the acute and chronic disability from VTE. 6,7 The purpose of this review is to discuss the rationale and evidence for an endovascular treatment approach for high-risk acute DVT and PE patients.
Is VTE a cause of mortality?
VTE is increasingly recognized as a cause of significant morbidity and mortality in the United States. An interventional approach to managing both acute LE-iliofemoral DVT and massive and submassive PE has great promise. There remains a paucity of robust long-term evidence, particularly addressing safety outcomes in therapies utilizing drugs and delivery systems that can result in bleeding complications. A highly individualized approach encompassing patient selection, type of therapy, operator and hospital level of experience should be followed to maximize the benefits of an interventional strategy as well as minimize the risk of harm.
What is PE in pulmonary thromboembolism?
PE usually occurs when a part of this thrombus breaks off and enters the pulmonary circulation. Very rarely, PE can occur from the embolization of other materials into the pulmonary circulation such as air, fat, or tumor cells.[1] The spectrum of PE and DVT combined is referred to as venous thromboembolism (VTE).
What is PE in pulmonary artery?
Pulmonary embolism (PE) occurs when there is a disruption to the flow of blood in the pulmonary artery or its branches by a thrombus that originated somewhere else. In deep vein thrombosis (DVT), a thrombus develops within the deep veins, most commonly in the lower extremities.
Why is the case fatality rate of PE decreasing?
It is important to note that the case-fatality rates of PE have been decreasing; this might be from the improvement in diagnostic modalities and initiation of early intervention and therapies. Pathophysiology. Pulmonary embolism occurs when clots break off and embolize into the pulmonary circulation.
What is the right ventricle pressure overload?
Thus, the levels of natriuretic peptides in blood reflect the severity of RV dysfunction in acute PE. [24] Troponin.
How long does it take for a PE patient to get anticoagulant?
First, all patients with PE should receive three or more than three months of anticoagulant treatment. Second, after the anticoagulant treatment is stopped, the risk of recurrence is expected to be similar if anticoagulants are stopped after 3-6 months compared with longer treatment periods (e.g., 12-24 months).
What is the primary cause of death in severe PE?
Right ventricle (RV) failure due to acute pressure overload is the primary cause of death in severe PE. Given the above pathophysiological considerations, clinical symptoms, and signs of overt RV failure and hemodynamic instability, are indicative of a high risk of early (in-hospital or 30 day) mortality.
What is PVR in PE?
In PE, pulmonary vascular resistance (PVR) increases due to the mechanical obstruction of the vascular bed with thrombus and hypoxic vasoconstriction. Pulmonary artery pressure (PAP) increases if thromboemboli occludes greater than 30% to 50% of the total cross-sectional area of the pulmonary arterial bed.
How to treat pulmonary embolism?
How Pulmonary Embolism Is Treated. Treatment is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death. Blood thinners or anticoagulants are the most common treatment for a blood clot in the lung. While hospitalized an injection is used, but ...
How long after pulmonary embolism can you breathe?
If you continue to have breathing difficulty 6 months after a pulmonary embolism you should talk to your doctor and get tested for CTEPH. Your physician may complete a "hypercoagulability" evaluation on you at some point after your diagnosis. This could include blood tests looking for a genetic cause of your DVT.
What is a clot dissolver?
Clot dissolvers called thrombolytics are a medication reserved for life-threatening situations because they can cause sudden and severe bleeding. For a very large, life-threatening clot, doctors may suggest removing it via a thin, flexible tube (catheter) threaded through your blood vessels.
How long do you have to take blood thinners?
Patients will normally have to take medications regularly for an indefinite amount of time, usually at least 3 months.
Can blood thinners dissolve blood clots?
It is important to note that blood thinners won’t dissolve the blood clot. In most cases, the hope is your body will eventually dissolve the clot on its own. If it doesn’t, more drastic measures may need to be taken.
Can pulmonary embolism be life threatening?
Managing Pulmonary Embolism. While a pulmonary embolism can be life-threatening, most patients survive and need to learn how to live with the risk of recurrence.
Epidemiology
Prognosis
Contraindications
Uses
Specialist to consult
Treatment
- Pulmonary embolism can be difficult to diagnose, especially in people who have underlying heart or lung disease. For that reason, your doctor will likely discuss your medical history, do a physical exam, and order one or more of the following tests.
Criticism
Medical uses