The Transdiagnostic Treatment Enhanced cognitive behavior therapy (CBT-E) is a transdiagnostic treatment for eating disorder psychopathology rather than for a particular eating disorder diagnosis. It is derived from the transdiagnostic theory outlined above, which highlights the maintaining processes that need to be addressed in treatment.
Full Answer
What is the transdiagnostic view of eating disorders?
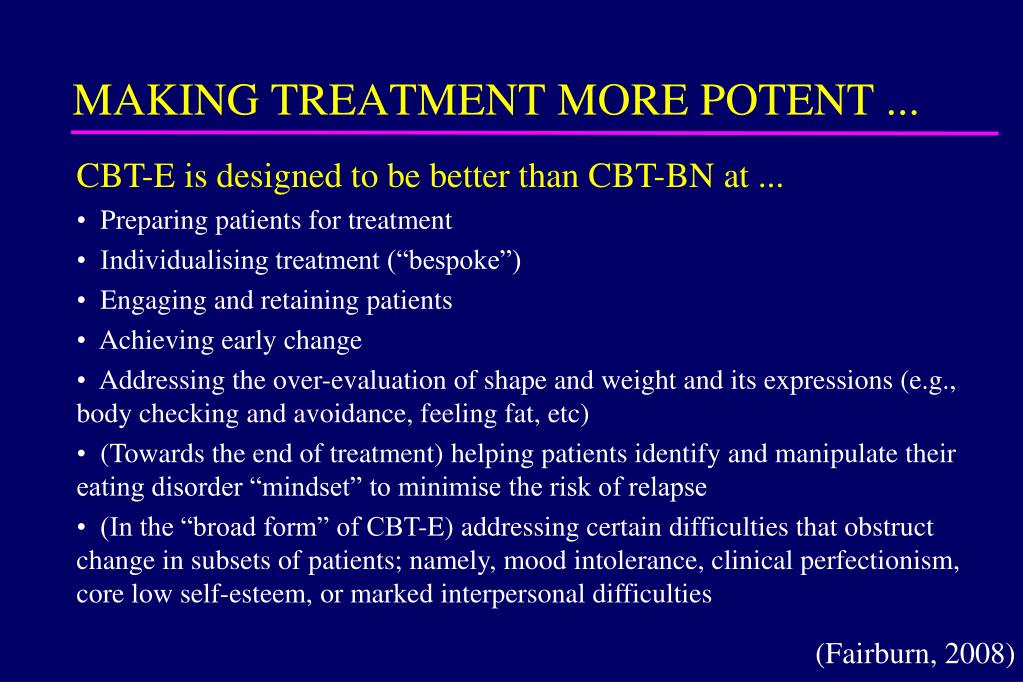
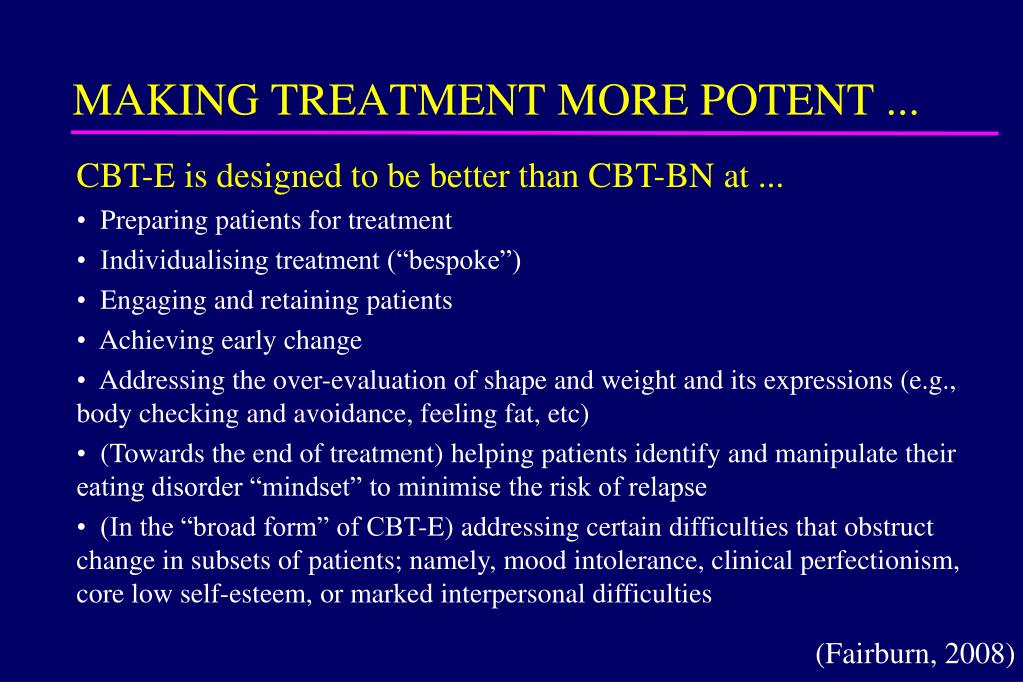
Hence the Centre for Research on Eating Disorders at Oxford (CREDO) team reconceptualised the existing evidence-based form of CBT for bulimia nervosa and adapted it to make it suitable for all forms of eating disorders. The result was the development of a new transdiagnostic cognitive behavioural treatment called Enhanced CBT (CBT-E).
How are eating disorders classified and treated?
A transdiagnostic approach is ideal in the treatment of eating disorders, as it recognizes the complexity of this population. A transdiagnostic approach cuts across DSM-5 disorders, and targets core mechanisms, not specific disorders, while providing a unifying case conceptualization to the treatment of complex clients.
What is a transdiagnostic approach?
Abstract. Categorical models dominate the eating disorder field, but the tandem use of categorical and dimensional models has been proposed. A transdiagnostic dimensional model, number of lifetime eating disorder behaviors (LEDB), was examined with respect to (1) its relationship to a variety of indicators of the individual's functioning, (2) the degree to which it …
What is CBT for eating disorders?
Jan 01, 2017 · Enhanced cognitive behavior therapy (CBT-E) is a transdiagnostic treatment for eating disorder psychopathology rather than for a particular eating disorder diagnosis. It is derived from the transdiagnostic theory outlined above, which highlights the maintaining processes that need to be addressed in treatment.
What is the Transdiagnostic theory?
What is Fairburns Transdiagnostic model?
How is EDNOS treated?
- Medical stabilization.
- Decreased purgative behavior.
- Nutritional stabilization.
- Normalized eating.
- Pattern of weight rehabilitation, if necessary.
- Development of positive coping skills.
- Family education.
- Development of a recovery plan.
How do you deal with OSFED?
Is EDNOS real?
What is an example of EDNOS?
What does EDNOS look like?
Ednos consists of cycles of restricting food, then bingeing, followed by purging after feelings of shame and guilt. An obsessive nature and over awareness is common surrounding food, weight, and calorie control, where restricting and avoiding meals is another of the many symptoms.
Is OSFED serious?
What causes OSFED?
What does OSFED stand for?
How does eating disorder treatment work?
Treatment is guided by a personalized formulation of the patient’s difficulties, constructed at the beginning of treatment and revised as necessary as treatment progresses. It uses a number of well-specified strategies and procedures designed to target and disrupt the mechanisms maintaining the patient’s disorder. This generally involves encouraging patients to make changes in the way they behave and then helping them to understand and reflect on the effects and implications of these changes. In this way, they learn to decenter from their eating problems and eventually to identify their eating disorder mindset and learn to control and manipulate it.
What are the current methods of classifying eating disorders?
In this chapter, we argue for an alternative transdiagnostic approach, which might better reflect clinical reality. The transdiagnostic treatment derived from this theory is described in outline together with its numerous extensions and variations. Evidence supporting both the theory and the treatment is presented, and future directions for research are identified.
What is CBT E?
Enhanced cognitive behavior therapy (CBT-E) is a transdiagnostic treatment for eating disorder psychopathology rather than for a particular eating disorder diagnosis. It is derived from the transdiagnostic theory outlined above, which highlights the maintaining processes that need to be addressed in treatment. It is a treatment for patients with an eating disorder of clinical severity and was originally designed as an individual treatment for adult outpatients irrespective of gender with a body mass index (BMI)1 between 15.0 and 40.0. It has subsequently been adapted for use with younger patients and for more intensive use in outpatient, day patient and inpatient settings (including patients with a BMI below 15.0). Management of patients with a BMI over 40.0 has been addressed elsewhere ( de Zwaan, 2010 ).
What is cognitive behavioral therapy?
Subsequently the cognitive behavioral account of the maintenance of bulimia nervosa was enhanced and extended in two major respects: It was extended to cover all eating disorders and to embrace four additional maintaining processes that , in certain patients, interact with the core eating disorder maintaining mechanisms and constitute obstacles to change ( Cooper and Fairburn, 2011, Fairburn et al., 2003 ).
What is the cognitive behavioral view of eating disorders?
According to the cognitive behavioral view, it is the distinctive scheme of self-evaluation shared by patients with eating disorders that is of central importance in maintaining these disorders. Other clinical features can be understood as stemming directly from this “core psychopathology ,” including the extreme weight-control behavior (e.g., strict dieting, self-induced vomiting, laxative and diuretic misuse, and driven exercising), the various forms of body weight and shape checking and avoidance, and the preoccupation with thoughts about eating, weight, and shape. The one prominent feature that is not obviously a direct expression of the core psychopathology is binge eating, which occurs in many patients with eating disorders whatever their DSM diagnosis. The cognitive behavioral theory proposes that binge eating is largely maintained by attempts to adhere to extreme dietary rules. Patients’ tendency to react in a negative and extreme (often, dichotomous) fashion to the almost inevitable breaking of these rules results in even minor dietary slips being interpreted as evidence of poor self-control and personal weakness. The response to this perceived lack of self-control is a temporary abandonment of efforts to restrict eating, and thus these attempts are repeatedly interrupted by episodes of binge eating. This binge eating maintains the core psychopathology by intensifying patients’ concerns about their ability to control their eating, shape, and weight and encourages further dietary restraint, thereby increasing the risk of further binge eating. Three further processes also contribute to and maintain binge eating. First, life difficulties and associated mood changes increase the likelihood that patients will break their dietary rules. Second, since binge eating temporarily ameliorates such mood states and distracts patients from thinking about their difficulties, it can become a way of coping with these difficulties. Third, if the binge eating is followed by compensatory vomiting or laxative misuse, this also maintains binge eating because patients’ mistaken belief in the effectiveness of such “purging” in preventing energy absorption removes a major deterrent to binge eating.
Is binge eating disorder a clinical condition?
As was the case with earlier versions of the diagnostic criteria, the DSM-5 regards anorexia nervosa, bulimia nervosa and binge eating disorder as distinct clinical states and, as such, suggests that each requires its own form of treatment.
Is binge eating disorder a serious disorder?
The eating disorders, anorexia nervosa, bulimia nervosa, binge eating disorder, and their variants are serious disorders that are accompanied by significant impairment in physical and psychological functioning as well as in quality of life. They typically begin in adolescence and may run a chronic course; once established they are difficult to treat. They are less common among men than women and represent a significant source of morbidity among adolescent girls and young women in particular. Both anorexia nervosa and bulimia nervosa are associated with increased mortality, and binge eating disorder is associated with an increased risk of obesity. Despite the existence of evidence supported specialist interventions for eating disorders, there is a well-documented unmet need for treatment. Eating disorders are often undetected and even when they come to attention they may not receive appropriate treatment.
What is a soft transdiagnostic approach?
What we shall call here “soft” transdiagnostic approaches preserve the underly ing diagnostic classification while seeking to elucidate processes or develop interventions that have relevance to one or more of the diagnoses as traditionally formulated. In contrast, more radical, “hard” transdiagnostic approaches dispense with the diagnostic system altogether, seeking to replace it with alternative frames of reference that characterize mental ill health in new ways.
What are the advantages of diagnostic taxonomies?
A much-vaunted advantage of diagnostic taxonomies is facilitated clinical assessment, management and intervention. This has led, within the domain of psychological interventions which is our primary focus here, to the establishment of an evidence-base for a plethora of single-disorder-focused treatment approaches. These are then endorsed by diagnostically organized guidelines such as those compiled by the United Kingdom’s National Institute for Health and Care Excellence (NICE; Pilling, Whittington, Taylor, & Kendrick, 2011). Comorbid conditions are generally either glossed over, or minimally treated within these intervention packages and there little attention is paid to symptoms that fall outside of the diagnostic rubric. However, the majority of mental health treatments of all types actually appear to be effective across broad ranges of clinical populations, for example drugs such as selective serotonin reuptake inhibitors (SSRIs) and benzodiazepines, and psychological protocols such as cognitive-behavior therapy (CBT), or extinction-based approaches for anxiety-related difficulties. There is thus a mismatch between the clinical reality on the ground and the nature and scope of the recommended interventions. As a result, much of real-world clinical practice eschews the diagnosis-led treatment evidence base, preferring instead eclectic combinations of treatment elements tailored to the presentation and formulation of individual clients. This pragmatic approach enables goodness-of-fit matching of interventions to specific vulnerabilities and processes relevant to the individual, and provides a flexible treatment model that can be applied across a range of presentations including, critically, complex formulations, comorbidity, and subsyndromal or prodromal symptoms.
What are the three intellectual domains of diagnostics?
These diverse concerns about the diagnostic approach stem somewhat independently from research and scholarship across the three intellectual domains of classification and nosology, basic biopsychosocial research, and clinical science . Perhaps unsurprisingly, therefore, the alternative transdiagnostic approaches that abnegate the traditional psychiatric paradigm have also evolved and matured somewhat separately in each of these spheres, as we highlight below.
How is diagnostic taxonomy generated?
The established diagnostic taxonomy has been generated through consensual decision-making by groups of experts under the auspices of learned bodies (Blashfield, 1984). Although this “authoritative” approach (Krueger et al., 2018) relies on some empirical data (e.g., the DSMfield trials; Regier, Narrow, et al., 2013), this is secondary to the influence of expertise, tradition and politics. An alternative approach to the ex cathedradiagnostic manuals is fully empirical, focusing on the quantitative structure of signs, symptoms, and behaviors associated with mental health and distress, and deriving classification frameworks based on the resultant data.
What is the primary function of diagnostics?
A primary function of any diagnostic system should be to facilitate our understanding of a complex problem space by organizing central, recurrent patterns into discrete categories. The data on heterogeneity cast doubt on whether this pragmatic aim of the psychiatric paradigm has even come close to being realized.
How many symptom profiles are there for MDD?
Indeed, when we account for all of the subsymptoms and directional qualifiers, there are 16,400 different symptom profiles that all qualify as MDD (Fried & Nesse, 2015). Such heterogeneity is orders of magnitude greater for complex criteria-based diagnoses such as posttraumatic stress disorder where there are 636,120 permutations that qualify for the diagnosis (Galatzer-Levy & Bryant, 2013).
What is a formal diagnosis?
Formal diagnoses of different disorders typically comprise a number of criteria—clusters of conceptually similar symptoms that are heuristically grouped together. Most criteria contain more than one symptom and one or more of these symptoms would need to be present for the criterion to be met. Typically, the overall diagnosis then further depends on a specified number of criteria being satisfied. Even for diagnoses where criteria are not explicitly offered, diagnoses normatively require only a subset of symptoms from a larger set to be present. This polythetic checklist approach means that individuals receiving the same diagnosis can present with very different symptoms such that each diagnostic category incorporates built in heterogeneity.
