WHOLESALE ACQUISITION COST (WAC) The Wholesale Acquisition Cost (WAC), also known as the list price, for a 4-week supply of MAVYRET is $13,200.00 as of January 2020. WAC may not reflect the price paid for patients.
How much does hepatitis C treatment cost?
2010 wholesale acquisition costs: 41,803: The total treatment cost input was a function of the regimen used for each genotype in the given year weighted by the prevalence of each genotype. Regimen list prices were identified in RED BOOK. 21 2012 wholesale acquisition costs: 97,196 2014 wholesale acquisition costs: 106,360 2016 wholesale acquisition costs: 68,753
Who pays for HCV treatment?
Jun 01, 2018 · Hepatitis C virus (HCV) is transmitted by exposure to blood or other bodily fluids that contain HCV. Approximately 3.5 million Americans have chronic hepatitis C. About 19,000 of these people die ...
What are the new drugs available to treat hepatitis C?
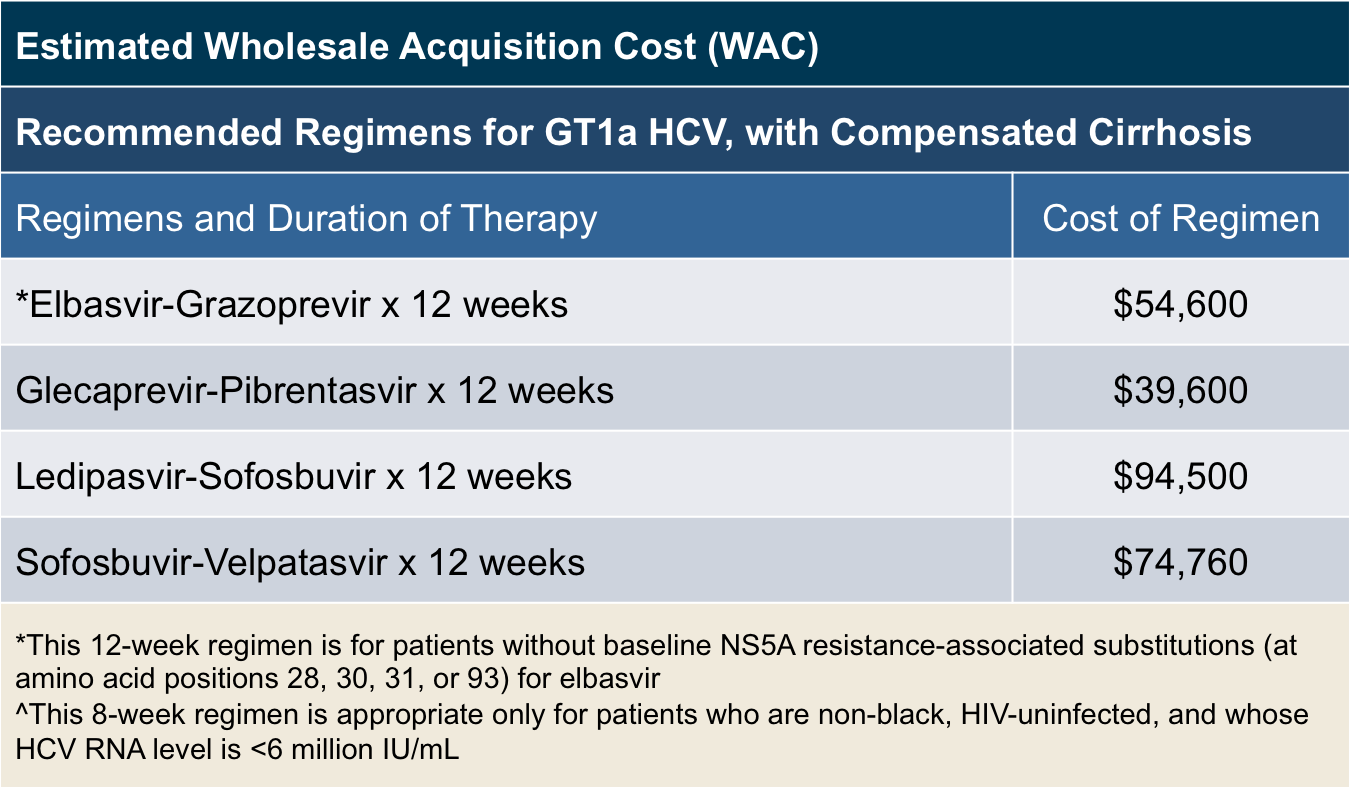
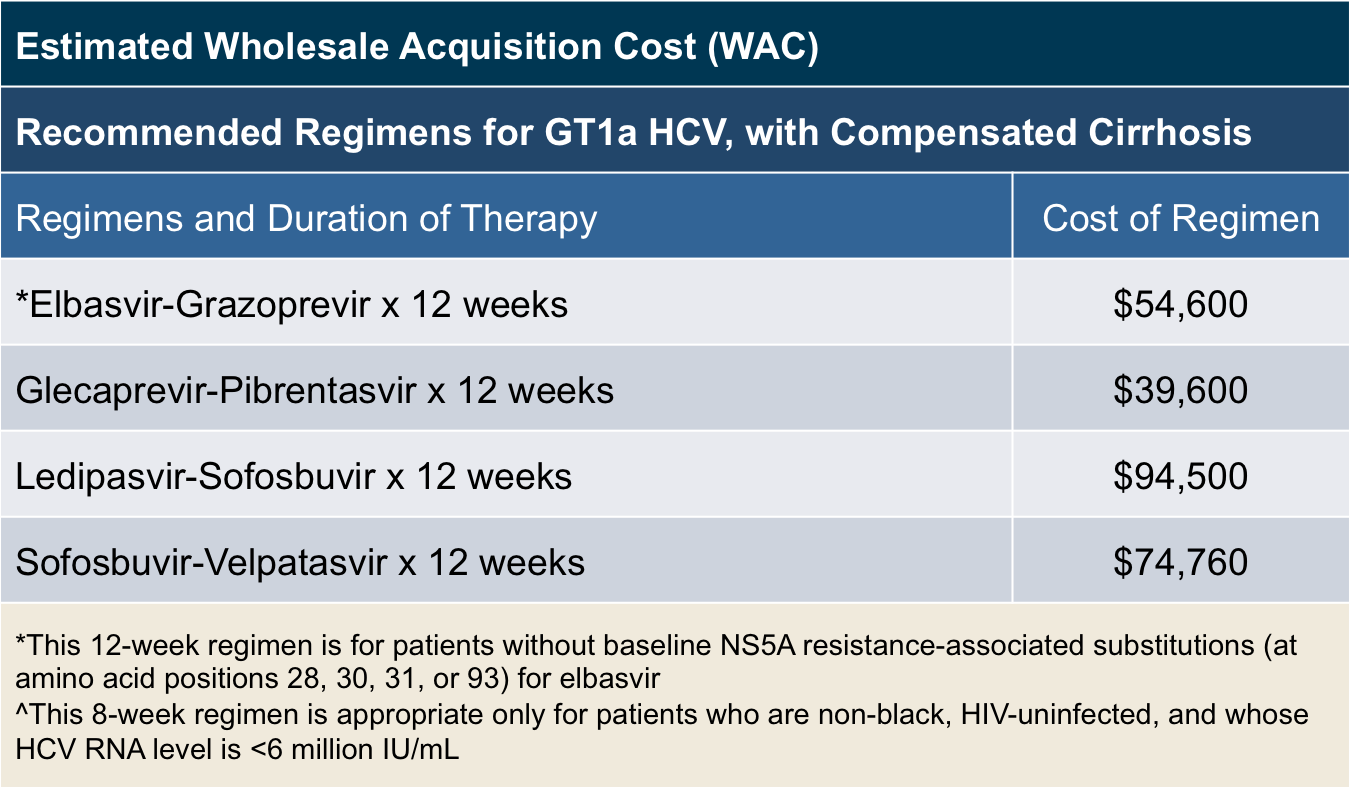
Estimated wholesale acquisition costs for common DAA treatment regimens can range from around $25,000 –$100,000 for the course. 5 Although pharmaceutical companies offer medication assistance limited programs, many patients are not able to easily access or qualify for this assistance. Despite the high cost of treatment, several
Should Medicare-Medicaid partnerships pay for hepatitis C treatment?
May 20, 2021 · Costs of DAA treatment were based on the wholesale acquisition price of glecaprevir/pibrentasvir (Mavyret; AbbVie): $26,400 to $39,600 for an 8- to 12-week treatment course ( Table 1 [ part A and...
How much does Sovaldi cost in America?
Official Answer. The wholesale cost of Sovaldi is $1000 per 400mg tablet. A 12-week treatment course of Sovaldi costs around $84,000 and a 24-week course, $168,00.Apr 23, 2020
How much does it cost to get rid of hep C?
The Cost of Hepatitis C Treatment Harvoni cost even more -- $94,500 for a 12-week course, though some patients may be cured after only eight weeks, or $63,000. Gilead's newer offering, Epclusa, goes for just over $74,000. The gamechanger in the market may be Mavyret, which costs $26,500 for treatment.Sep 30, 2019
How much is Sovaldi in Canada?
Sovaldi sells for about $1,000 a pill in the U.S., while a generic version costs only $4 a pill in India. Canada pays $55,000 for a course of treatment.Jul 19, 2017
How much does maverick for hep C cost?
Abbvie has priced Mavyret at $13,200 per month, or $26,400 per treatment course, before discounts. Although this is still expensive, Macyret is priced significantly lower than other hepatitis C treatments.Aug 23, 2017
How can I get hep C treatment for free?
Patient assistance programs (PAPs) offer free hepatitis C drugs to lower-income people who are uninsured or underinsured, and who do not qualify for insurance programs such as Medicaid or Medicare.
Is hep C treatment covered by insurance?
Luckily, hep C treatment is covered by most insurance plans, so for many people, the cheapest way of getting it will be through insurance (although you'll probably need prior authorization). If your hep C treatment is not covered by your insurance, ask your doctor about an appeal.Jan 27, 2019
Why is Sovaldi so cheap in India?
The newspaper says that current treatments for the disease in India run about $6,000 and require a 24- to 48-week course of injectables that come with serious side effects. So Sovaldi will be cheaper and easier to administer, with fewer side effects and the ability to cure many of the cases.
How much does hep C treatment cost in Canada?
That cure is a combination of antiretroviral drugs called Sofosbuvir and Daclatasvir. According to Hill's research, the price charged by pharmaceutical manufacturers in Canada for 12-week course of treatment is about $68,000 US.Nov 7, 2017
Is Hep C treatment covered by OHIP?
The Ontario government says it will cover the cost of medication for all hepatitis C patients, regardless of the severity of the disease, a move that's being touted as a game-changing decision by health professionals in the field.Mar 5, 2018
How much does Maviret cost?
GLECAPREVIR + PIBRENTASVIRCode & PrescriberMedicinal Product Pack (Name, form & strength and pack size)General Patient Charge11354NGLECAPREVIR + PIBRENTASVIR glecaprevir 100 mg + pibrentasvir 40 mg tablet, 84 (PI, CMI)$42.50Available brandsMaviret
Is MAVYRET a generic?
No. There is currently no therapeutically equivalent version of Mavyret available in the United States. Note: Fraudulent online pharmacies may attempt to sell an illegal generic version of Mavyret. These medications may be counterfeit and potentially unsafe.Mar 10, 2022
How much does hep C treatment cost UK?
A 12-week course of treatment with elbasvir-grazoprevir usually costs £36,500 per patient, but the NHS will pay less than this as the company has offered a confidential discount. Taken once daily, the tablet could treat around 4,000 patients in the first year, alongside other options already available for hepatitis C.
How much does it cost to cure hepatitis C?
According to the Pharmacy Times, the cost of treatment can be as low as $54,600 for the 12-week course and the entry to the market of new, cheaper drugs is likely to continue to bring the cost of hepatitis C treatments down.
How much does Sovaldi cost?
Sofosbuvir (Sovaldi): This medication costs $1,000 per 400 mg pill. The total cost for a 12-week course is around $84,000, and doctors will typically prescribe it with other medicines, such as simeprevir. Ombitasvir-paritaprevir-ritonavir and dasabuvir (Viekira Pak): The cost for this medication is $83,319 for a 12-week treatment course.
Is hepatitis C treatment successful?
Recent innovations in hepatitis C treatment mean that treatment is usually successful. However, for some people, the costs of these medications can be prohibitive. While prices may decrease in the future, there are currently no guarantees.
Is hepatitis C a direct-acting drug?
In 2014, the United States Food and Drug Administration (FDA) approved drug treatment s called direct-acting antiviral medications that were available in oral form only to treat hepatitis C, according to the journal Open Forum Infectious Diseases . Several medications to treat hepatitis C have met FDA approval since then.
How to pay for HCV?
If you’re concerned about paying for HCV medications, remember that you aren’t alone as you seek treatment. There are people and organizations that can help you, including the following: 1 Your doctor. They can help you by ordering and documenting the tests you’ll need so you can qualify to get your medications, especially if you’re working with a liver or infection specialist. 2 Most drug manufacturers. There are patient assistance programs that offer free or reduced-cost medications for people who meet their criteria. 3 Patient advocacy groups. These groups provide assistance with all aspects of HCV treatment. For instance, if your insurer denies treatment, you can appeal the decision with help from one of these groups. Your doctor can also help in this situation.
How many people die from hepatitis C each year?
Americans have chronic hepatitis C. About 19,000 of these people die each year from cirrhosis or liver cancer. Fortunately, recent advancements in the fight against this virus have changed the outlook for people with HCV. New drugs have transformed the disease from one that can, at best, be controlled to one that can be cured for most people who ...
What is the liver infection?
Hepatitis C is a viral infection that attacks the liver. Infection with hepatitis C can lead to serious liver disease, including cirrhosis and cancer. Hepatitis C virus (HCV) is transmitted by exposure to blood or other bodily fluids that contain HCV.
What is a direct acting antiviral?
of people who take them, depending on the type of HCV infection and treatment exposure. These new drugs are called direct-acting antivirals (DAAs). The U.S. Food and Drug Administration (FDA) approved the first of these medications for HCV treatment in 2011. Several more medications have been approved since that time.
Is generic medicine cheaper than brand name?
It also means there are no generic versions of these drugs yet. Generics are typically much cheaper than brand- name versions. The FDA determines how long this period of exclusivity will last. During this time, the pharmaceutical companies have a lot of freedom in establishing prices.
What are the criteria for liver disease?
These criteria may be based on: the severity of liver disease. whether the person avoids alcohol and drug use. whether the drug’s prescribed by a doctor who specializes in liver diseases. the life expectancy of the person seeking treatment. whether less expensive treatments could be used first.
Can hepatitis C be treated with drugs?
Today there are several drug options available that can cure hepatitis C infection — that’s the great news. What’s less great is the high cost of these drugs. However, there are many options you can explore to find help paying for these medications.
What is the cure rate for hepatitis C?
Direct-acting antivirals (DAAs) are associated with cure rates above 95% for hepatitis C virus (HCV). 1 However, the exorbitant costs of DAAs historically have made access prohibitive for many patients.
What is the semi infectious disease model?
The semi-infectious disease model assessed the cost-effectiveness of HCV outcomes based on increased treatment probabilities under the total coverage scenario, compared with 2 scenarios reflecting the current payer model with standard coverage for all beneficiaries or prioritized coverage for all high-risk beneficiaries ( Figure 1 ). In the latter alternative, the 60% of patients with chronic HCV who had a liver fibrosis score of 2 or higher, as opposed to a fibrosis score of 0 or 1, received DAAs first, before lower-risk patients, in order to better manage budget impact. 15
Why is Maryland not a direct acting agent for Medicare?
Objectives: Most Medicaid beneficiaries with hepatitis C virus (HCV) are not treated with direct-acting agents because of budget constraints, but they experience costly complications after becoming Medicare eligible. Maryland’s “total coverage” proposal could receive a credit from Medicare to offset Medicaid investments in treatments ...
Is DAA coverage for HCV?
Providing total coverage for DAA medications for all patients with HCV is systematically complex and may not be economically viable for state Medicaid programs that face some of the highest rates of HCV among payers. Joint Medicaid-Medicare coverage provides an efficient solution to treat all patients now to reduce harm caused by chronic infection in the United States. Recent price reductions for HCV treatments improve the outlook on affordability at the system level, as the $26,400-plus price tag still makes it inaccessible to individual Medicaid enrollees. Furthermore, the long-term costs of untreated HCV typically borne by Medicare are offset under this concept. The Maryland TCOC model gives Medicare the option of crediting Medicaid for spending money today that it will save on health care costs in the future. This is an approach to resolve the mismatch between investing today and getting future returns.
Is expanded coverage for hepatitis C cost effective?
Expanded coverage under a joint partnership by Medicare and Medicaid to treat all prevalent cases of hepatitis C virus (HCV) appears to be cost-effective by saving money and improving patient outcomes.
What is cost effectiveness analysis?
Cost-effectiveness analysis (CEA) compares the relative costs and outcomes of 2 or more interventions. CEA explicitly recognizes budget limitations for healthcare spending and seeks to maximize public health benefits within those budgetary constraints. The core question that CEA addresses is whether to invest limited healthcare dollars in a new treatment/therapy or use that money to invest in another healthcare intervention that would provide better outcomes for the same monetary investment. The focus of CEA is, therefore, not simply cost or saving money but health benefits. It assumes that all available resources will be spent and provides a framework for prioritizing among available treatment options by formally assessing the comparative costs and health benefits accrued from a new treatment relative to current treatment.
What is the time horizon for CEA?
From a societal perspective, CEA uses a lifetime time horizon, meaning it considers lifetime costs and benefits, including those that occur in the distant future. Business budget planning, however, typically assumes a 1-year to 5-year perspective.
What does private insurance do?
Private insurance companies often have separate pharmacy and medical budgets, and use PBMs or directly negotiate drug pricing with pharmaceutical companies. Insurance companies determine formulary placement, which impacts the choice of regimens and out-of-pocket expenses for patients.
Is life expectancy a measure of benefit?
Life expectancy is a valuable measure of benefit but considering only mortality benefits fails to recognize the value of treatments that improve quality of life. The quality-adjusted life-year (QALY) provides a measure that integrates both longevity and quality of life and is the preferred outcome for CEA.
Is an intervention cost effective?
An intervention that is cost-effective is not necessarily affordable. Affordability refers to whether a payer has sufficient resources in its annual budget to pay for a new therapy for all who might need or want it within that year . Several characteristics of CEA limit its ability to speak to the budgetary impact of interventions being implemented in the real world.
Is HCV cost effective?
There is no formula that provides a good means of integrating the concerns of value and affordability. When new HCV therapies are deemed cost-effective, it indicates that these therapies provide good benefit for the resources invested and providing such therapy to more people would be a good long-term investment.
Is routine HCV testing cost effective?
Generally, routine HC V testing is cost-effective because the incidence and prevalence of HCV remain high in people who inject drugs with a notable rising prevalence in young adults who may not readily report their stigmatized risk behaviors.
