| Name | Dosage | |
| Levofloxacin | 250 - 750 mgs | once a day |
| Moxifloxacin | Intravenous. 400 mgs | once a day |
| Cefoperazone | 2 - 4 g (max 8 g) | at least 10 days |
| Cefuroxime | Intramuscular, intravenous. 750-1500 mgs | 3-4 times a day for 5 - 10 days and more |
What is the best antibiotic to treat strep throat?
Aug 03, 2021 · Primary prevention comprises of prompt treatment of streptococcal throat or skin infection via a single injection of benzathine penicillin or oral penicillin for 10 days after confirmation of S. pyogenes infection.
Does doxycycline treat streptococcus?
27 rows · Streptococcus Pyogenes treatment. Antibiotics are active against the Streptococcus ...
Does Bactrim cover strep pyogenes?
Group A Streptococcus (group A strep, Streptococcus pyogenes) can cause both noninvasive and invasive disease, as well as nonsuppurative sequelae. Learn more about the etiology, clinical features, diagnosis and treatment options, prognosis and complications, and prevention of some of these infections below. symptom icon. Pharyngitis (Strep Throat)
Is there no treatment for strep C?
Aug 03, 2021 · Streptococcus pyogenes is a major human-specific bacterial pathogen that causes a wide array of manifestations ranging from mild localized infections to life-threatening invasive infections. Ineffective treatment of S. pyogenes infections can result in the postinfectious sequela acute rheumatic fever and post-streptococcal glomerulonephritis. …
What antibiotic treats Streptococcus?
Doctors most often prescribe penicillin or amoxicillin (Amoxil) to treat strep throat. They are the top choices because they're safer, inexpensive, and they work well on strep bacteria.Aug 12, 2020
What causes Streptococcus pyogenes?
Strep throat is an infection of the throat and tonsils caused by a bacteria called group A streptococcus , also known as Streptococcus pyogenes. This bacteria lives in the nose and throat. You can get the infection from someone who is sick with strep A bacteria or is a carrier of it.Sep 27, 2020
Does amoxicillin treat Streptococcus pyogenes?
pyogenes, Staphylococcus aureus, or a mixed inoculum of both organisms was inserted. Oral therapy was started 4 h after infection and continued for 3 days. Both amoxicillin and amoxicillin-clavulanic acid were effective in eliminating the streptococci from the pure wound infection.
How can Streptococcus pyogenes be prevented?
To prevent strep infection:Wash your hands. Proper hand-washing is the best way to prevent all kinds of infections. ... Cover your mouth. Teach your children to cover their mouths with an elbow or tissue when they cough or sneeze.Don't share personal items. Don't share drinking glasses or eating utensils.Dec 17, 2020
Does azithromycin treat strep?
Strep throat: Azithromycin is FDA-approved to treat strep throat (also known as streptococcal pharyngitis). If you are allergic to penicillin antibiotics, which are usually the first choice of treatment for this infection, a Z-Pack may be a good option.Oct 8, 2020
Does amoxicillin treat tonsillitis?
Penicillin and amoxicillin are the antibiotics that doctors prescribe most often to adults with bacterial tonsillitis. People who are allergic to penicillin antibiotics will receive a suitable substitute.Jun 1, 2020
Does doxycycline treat strep?
Doxycycline is a broad spectrum tetracycline antibiotic effective against some streptococcus species. Whilst not first line treatment, it can be used to treat strep throat and to prevent rheumatic fever. It should be used for no less than 10 days.Sep 16, 2020
Does Augmentin cover Streptococcus?
The combination drug amoxicillin-clavulanate potassium (Augmentin) is resistant to degradation from beta-lactamase produced by copathogens that may colonize the tonsil-lopharyngeal area. Amoxicillin-clavulanate is often used to treat recurrent streptococcal pharyngitis.Apr 15, 2001
Is azithromycin an antibiotic?
Azithromycin is in a class of medications called macrolide antibiotics. It works by stopping the growth of bacteria. Antibiotics such as azithromycin will not work for colds, flu, or other viral infections.
Is there a vaccine for Streptococcus pyogenes?
The search for safe and effective vaccines to prevent Streptococcus pyogenes infections has been ongoing for decades. The fact that there is not a licensed vaccine is remarkable, considering that S. pyogenes is one of the most studied human bacterial pathogens.Feb 10, 2016
How do you get rid of streptococcus bacteria?
In the meantime, try these tips to relieve symptoms of strep throat:Get plenty of rest. Sleep helps your body fight infection. ... Drink plenty of water. ... Eat soothing foods. ... Gargle with warm salt water. ... Honey. ... Use a humidifier. ... Stay away from irritants.Dec 17, 2020
Is there a vaccine for strep throat?
There is currently no vaccine available to prevent Strep A and can only potentially be treated with antibiotics. MCRI'S Dr Josh Osowicki said given Strep A only naturally infected humans, researchers were limited in what they could learn in the lab and using animal models.May 10, 2021
What is the M protein?
As a further antigen in Streptococcus pyogenes has the M-protein. This feature allows the subdivision into serovars. The typing relies today mostly on the sequencing of the genes of the M proteins (emm genes). Currently more than 150 different emm-types are known. The M protein has an antiphagocytic effect.
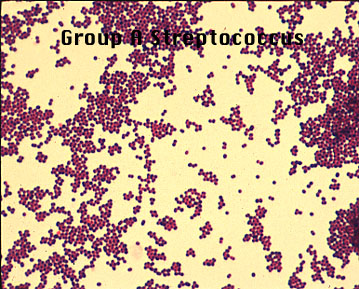
Is Streptococcus pyogenes gram positive?
Streptococcus pyogenes is one of the gram-positive cocci in chains overlap. The cell walls of streptococcal cells has some interesting features. The high content of peptidoglycan (murein layer) of carbohydrate (C polysaccharide) gives the cells a very strong structure. The C-polysaccharide antigen is effective.
What is the reservoir of streptococcus pyogenes?
Reservoir of Streptococcus pyogenes is the human. In particular, the throat is colonized, preferably in the winter months. As virulence is the M protein, which enables the propagation of the streptococci in the host only. The cell wall peptidoglycan and especially the complex of C polysaccharide exerts a tissue toxicity, which also emanates from dead cells of streptococci. They also provide a number of group A streptococcal exotoxins. The haemolysins streptolysin O and S destroy the membranes of red blood cells and other cells. Streptolysin O acts as an antigen that can be detected by measuring antibodies against this toxin (antistreptolysin titer). The pyrogenic streptococcal exotoxin (PSE) A, B, C are responsible for fever, rash, and scarlet, and enanthema in sepsis and toxic shock syndrome. They act as superantigens, causing a release of large amounts of cytokines. The enzymes streptokinase, DNAse and hyaluronidase favor the spread of infection in the tissue.
What is scarlet fever?
Scarlet fever is a special form of streptococcal pharyngitis, observed with the addition of a speckled rash of angina (and enanthema) is. A second group of diseases are infections of the skin (pyoderma, impetigo, erysipelas) dar. a very serious disease is necrotizing fasciitis, with or without the myositis.
How long does it take for a virus to incubate?
The incubation period ranges from one to three days. Among the diseases must be between acute infection and subsequent invasive disease (see below) can be distinguished.
Is penicillin a macrolide?
In penicillin allergy a macrolide antibiotic is considered. However, 8-15% of isolates are resistant to macrolides. The spectrum of activity of telithromycin (Ketek) also captures the majority of macrolide-resistant strains. Fluoroquinolones and cotrimoxazole (EUSAPRIM, COTRIM HEXAL FORTE, etc.) do not work reliably.
How is the diagnosis of streptococcal sequelae made?
The diagnosis is made by the culture test (determination of the serogroup) on blood agar plates. Are based on a currently available rapid antigen detection tests according to the Robert Koch Institute is not sensitive enough. Antibody detection assays are useful only in cases of suspected streptococcal sequelae.
What is the treatment for impetigo?
Impetigo generally requires antibiotic topical treatment or systemic antibiotics. Most people have heard of strep throat, and many have also had it. When S. pyogenes colonizes the throat, it typically induces fever, very sore throat (pharyngitis), swollen lymph nodes, and inflamed tonsils.
How many people die from rheumatic heart disease in a year?
People in undeveloped countries by far account for most cases, with an estimated 15 million people suffering from the condition. It is estimated that over 200,000 deaths occur each year, mostly in developing countries, as a result of rheumatic heart.
Where do pathogens live?
Pathogen for Many Illnesses. Bacteria: they live in our intestines, on our skin, in the soil, and in our food. In fact, without bacteria, we would not be able to live. There are a huge number of bacteria with whom we have formed a cooperative relationship, even the ones that make us sick in larger quantities.
Who is Amanda Robb?
Amanda has taught high school science for over 10 years. They have a Master's Degree in Cellular and Molecular Physiology from Tufts Medical School and a Master's of Teaching from Simmons College. They also are certified in secondary special education, biology, and physics in Massachusetts.
Can S. pyogenes cause skin infections?
pyogenes. Colonization by S. pyogenes on the skin can cause mild infections that don't even always need to be treated by antibiotics.
What is otitis media?
Otitis media is a painful ear infection resulting from the colonization by S. pyogenes in the Eustachian tubes. The route of infection can either be directly through the sinuses or following a throat infection.
How many words are in a vignette?
Each vignette is at least 500 words. Three vignettes are written. Each vignette is about a person that has a different Streptococcus pyogenes infection. Each vignette covers the symptoms, treatment, and prognosis for each patient.
What is strep pharyngitis?
Group A strep pharyngitis is an infection of the oropharynx caused by S. pyogenes. S. pyogenes are gram-positive cocci that grow in chains ( see figure 1 ). They exhibit β -hemolysis (complete hemolysis) when grown on blood agar plates. They belong to group A in the Lancefield classification system for β-hemolytic Streptococcus, and thus are called group A streptococci.
How is strep pharyngitis transmitted?
Typically transmission occurs through saliva or nasal secretions from an infected person. People with group A strep pharyngitis are much more likely to transmit the bacteria to others than asymptomatic pharyngeal carriers.
Can a RADT be positive?
Clinicians can use a positive RADT as confirmation of group A strep pharyngitis in children. However, clinicians should follow up a negative RADT in a child with symptoms of pharyngitis with a throat culture. Clinicians should have a mechanism to contact the family and initiate antibiotics if the back-up throat culture is positive.
What is the most common cause of pharyngitis in children?
Viruses are the most common cause of pharyngitis in all age groups. Experts estimate that group A strep, the most common bacterial cause, causes 20% to 30% of pharyngitis episodes in children. In comparison, experts estimate it causes approximately 5% to 15% of pharyngitis infections in adults.
How common is group A strep?
Humans are the only reservoir for group A strep. It is most common among children 5 through 15 years of age. It is rare in children younger than 3 years of age. In the United States, group A strep pharyngitis is most common during the winter and spring.
Can you take penicillin for pharyngitis?
Clinicians should not treat viral pharyngitis with antibiotics. Penicillin or amoxicillin is the antibiotic of choice to treat group A strep pharyngitis. There has never been a report of a clinical isolate of group A strep that is resistant to penicillin.
Do carriers of strep have RADT?
Asymptomatic group A strep carriers usually do not require treatment. Carriers have positive throat cultures or are RADT positive, but do not have clinical symptoms or an immunologic response to group A strep antigens on laboratory testing. Compared to people with symptomatic pharyngitis, carriers are much less likely to transmit group A strep to others. Carriers are also very unlikely to develop suppurative or nonsuppurative complications.