What is the best drug treatment for SVT?
They include:
- Valsalva maneuver. This is a way to increase pressure in the abdomen and chest. ...
- Carotid massage. Your healthcare provider may rub the carotid artery in your neck. ...
- Medicine. There are various kinds you can take. ...
- Electrocardioversion. This is a shock to the heart to restart a normal rhythm right away. ...
- Catheter ablation. This can help cure SVT. ...
What's the difference between SVT and PSVT?
Supraventricular tachycardia (SVT) is a fast heart rate that is starting in the atrium or upper chambers of the heart. Ventricular Tachycardia (VT) is a fast heart rate starting from the lower chambers of the heart. In general SVT is less serious than VT although both may require treatment.
What is the drug of choice for supraventricular tachycardia?
[Digoxin. The drug of choice for the in-utero treatment of paroxysmal supraventricular tachycardia]. [Article in Portuguese] Silva IS (1), Nunes C, Mimoso G, Castela E, Mesquita J. (1)Serviço de Obstetrícia, Maternidade Bissaya-Barreto, Coimbra.
How to stop an episode of supraventricular tachycardia?
You can make changes to your lifestyle to reduce your chances of having episodes, such as:
- cutting down on the amount of caffeine or alcohol you drink
- stopping or cutting back on smoking
- making sure you get enough rest
What is the best treatment for PSVT?
Catheter ablation: This outpatient procedure is used to treat or cure many types of heart arrhythmia, including PSVT. Catheter ablation is a mature technique known to be safe and effective. Therefore, it is considered a first-line therapy for PSVT.
What is first-line treatment for PSVT?
The first-line treatment in hemodynamically stable patients, vagal maneuvers, such as breath-holding and the Valsalva maneuver (ie, having the patient bear down as though having a bowel movement), slow conduction in the AV node and can potentially interrupt the reentrant circuit.
Does PSVT need to be treated?
Over time, PSVT can weaken your heart muscle. In severe cases, PSVT can lead to loss of consciousness, and it can even cause sudden cardiac arrest. If you have PSVT, see your provider regularly so they can monitor your heart health. In almost all circumstances, PSVT can be cured with catheter ablation.
What is the drug of choice for PSVT?
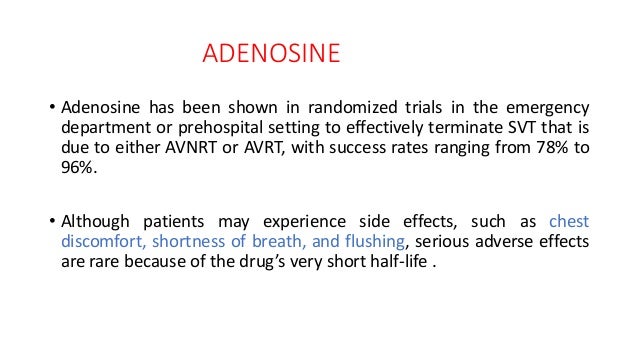
Intravenous Adenosine is the drug of choice in PSVT control in acute settings but is a very short acting agent.
Which drugs is the most preferred for the treatment of PSVT?
At this time, adenosine is the drug of choice of treatment. Verapamil and diltiazem are the most commonly used calcium channel blockers (CCBs). This review aimed to compare the efficacy of both drugs in the treatment of PSVT.
Is PSVT a serious heart condition?
PSVT is generally not life threatening. If other heart disorders are present, it can lead to congestive heart failure or angina.
What is the best medication to treat SVT?
What is the best medication for SVT?Best medications for SVTAdenocard (adenosine)AntiarrhythmicIntravenous injectionCardizem (diltiazem)Calcium-channel blockerOral or injectionCalan (verapamil)Calcium-channel blockerOral or injectionLopressor (metoprolol tartrate)Beta-blockerOral or injection3 more rows•Dec 28, 2020
Is PSVT normal?
PSVT is a fairly common type of abnormal heart rate. It can occur at any age and in people who don't have other heart conditions. The heart's sinus node typically sends electrical signals to tell the heart muscle when to contract. In PSVT, an abnormal electrical pathway causes the heart to beat faster than normal.
How long does a PSVT episode last?
Episodes can last for seconds, minutes, hours or (in rare cases) days. They may occur regularly, several times a day, or very infrequently, once or twice a year. The heart rate may be as high as 250 beats per minute, but is usually between 140 and 180 (a normal heartbeat should be 60-100 beats per minute at rest).
What is the best beta blocker for SVT?
Intravenous administration of calcium channel blockers, such as diltiazem, or beta-blockers, such as esmolol, is also commonly used for short-term SVT management.
What's the difference between PSVT and SVT?
Supraventricular tachycardia (SVT) is a rapid, regular heart rate where the heart beats anywhere from 150-250 times per minute in the atria. Another name for SVT is paroxysmal supraventricular tachycardia (PSVT). The word “paroxysmal” means occasionally or from time to time.
How to lower your pulse when you have a carotid artery?
Eyeball massage. You press gently on your eyes while they’re closed. Medication. Your doctor may prescribe drugs like ivabradine, beta-blockers, or calcium channel blockers to lower your pulse. Catheter ablation.
Is catheter ablation safe?
Catheter ablation is typically safe. But it could damage blood vessels or lead to infection.
Overview
Paroxysmal supraventricular tachycardia (PSVT) is a general term used to describe a type of arrhythmia (irregular heartbeat). Tachycardias are faster-than-normal heartbeats. If you have this condition, your heart may suddenly beat more quickly. Just as suddenly, your heart may slow down and beat at a normal rate.
Symptoms and Causes
PSVT (also called re-entry tachycardia) is a type of atrial arrhythmia. It happens when there is abnormal electrical activity in the atria. This is caused by an abnormally irritable area in the atria or by a short circuit in your heart causing electrical signals to travel around and around in a circular pattern.
Management and Treatment
Depending on your overall health and symptoms, you may not need treatment. If you have an arrhythmia, you’ll see a special type of heart doctor called a cardiologist. They may recommend you:
Prevention
You may not be able to avoid PSVT. But you can lower your risk by making smart lifestyle choices and staying healthy. To lower your risk, you should:
Living With
If you have any concerns about your heartbeat or you have symptoms of arrhythmia, talk to your provider. If you have PSVT, it’s very important to see your cardiologist regularly.
What class of drugs are used for atrioventricular reentrant PSVT?
Patients with atrioventricular reentrant PSVT should be treated with class lc drugs (propaphenone and flecainide)
What is the best drug for tachycardia?
Adenosine – drug of choice for tachycardias involving the atrioventricular node.
Do children with SVT need to be treated?
Children who have brief or infrequent bouts of SVT may not need treatment but should receive regular supervision (Mayo Clinic, 2019).
Is SVT a life threatening condition?
The outlook for children with SVT is excellent. The problem is usually not life- threatening plus the current treatments are highly effective. Successful ablation procedures lead to a cure. With no increased incidence of long term effents. https://www.mayoclinic.org/medical-professionals/cardiovascular-diseases/news/managing-pediatric-supraventricular-tachycardia/mac-20474690
What is the treatment for paroxysmal supraventricular tachycardia?
Acute management of paroxysmal supraventricular tachycardia (PSVT) includes controlling the rate and preventing hemodynamic collapse. If the patient is hypotensive or unstable, immediate cardioversion with sedation must be performed. If the patient is stable, vagal maneuvers can be used to slow the heart rate and to convert to sinus rhythm. If vagal maneuvers are not successful, adenosine can be used in increasing doses. If adenosine does not work, atrioventricular (AV) nodal blocking agents like calcium channel blockers or beta-blockers should be used, as most patients who present with PSVT have AV nodal reentrant tachycardia (AVNRT) or AV reentrant tachycardia (AVRT). These arrhythmias depend on AV nodal conduction and therefore can be terminated by transiently blocking this conduction.
Who should be consulted for patients with paroxysmal SVT, syncope, and/or preex?
A cardiologist should be consulted for patients with frequent episodes of paroxysmal SVT, syncope, and/or preexcitation syndromes. Consultation with a cardiologist should also be obtained for patients in whom medical management has failed.
What is the normal heart rate for atrioventricular nodal reentrant tachycardi?
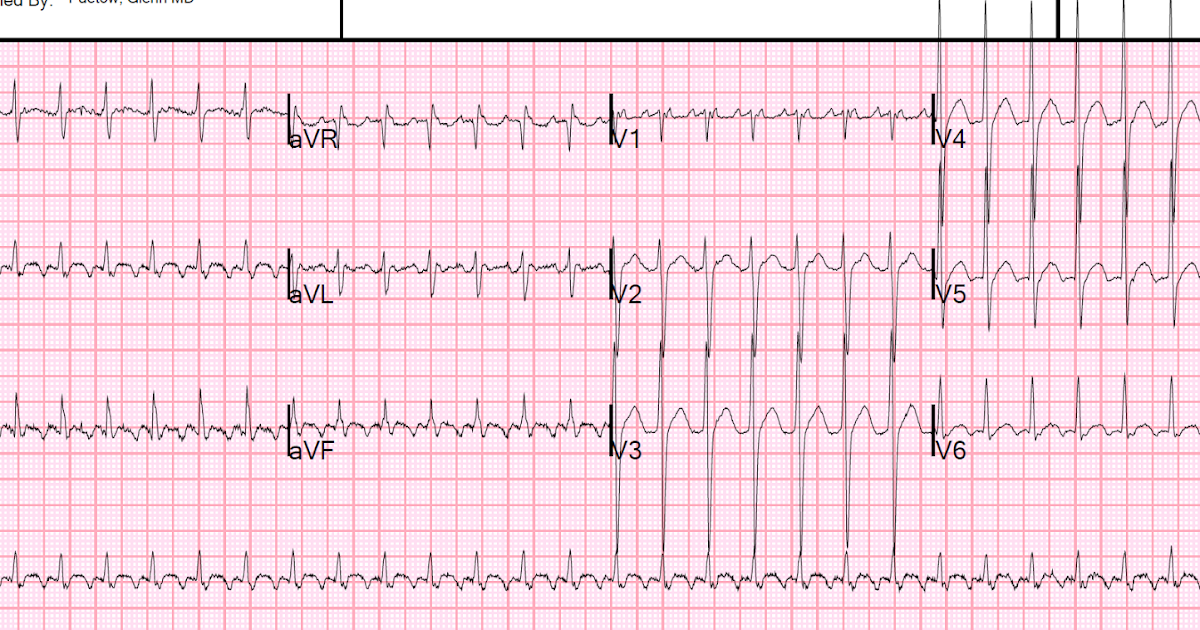
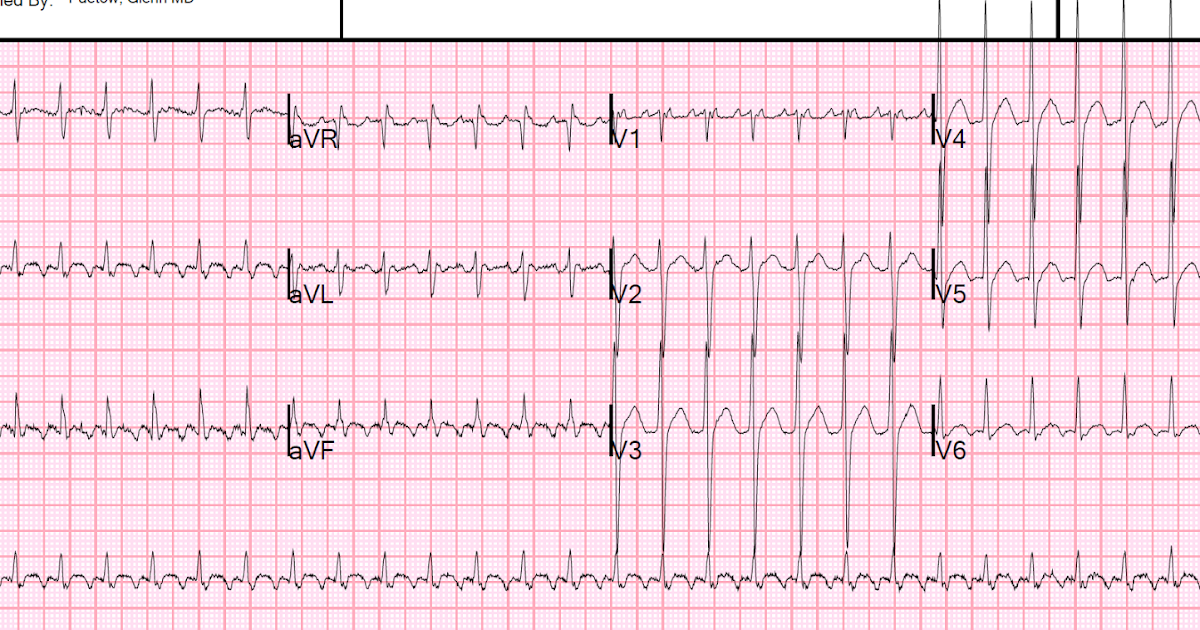
Atrioventricular nodal reentrant tachycardia. The patient's heart rate is approximately 146 bpm with a normal axis. Note the pseudo S waves in leads II, III, and aVF. Also note the pseudo R' waves in V1 and aVR. These deflections represent retrograde atrial activation.
What is the best treatment for preexcited atrial fibrillation?
Patients with preexcited atrial fibrillation should not be treated with intravenous AV nodal blocking agents, such as adenosine, beta-blockers, calcium channel blockers, and digoxin. Rather, if the patient is hemodynamically stable, intravenous procainamide should be administered. If the patient is unstable, direct current cardioversion should be performed.
How to treat atrial fibrillation?
The treatment of atrial fibrillation and atrial flutter involves controlling the ventricular rate, restoring the sinus rhythm, and preventing embolic complications. The ventricular rate is controlled with calcium channel blockers, digoxin, amiodarone, and beta-blockers. The sinus rhythm may be restored with either pharmacologic agents or electrical cardioversion. Medications such as ibutilide, propafenone, and flecainide convert atrial fibrillation and atrial flutter of short duration to sinus rhythm. Since atrial fibrillation and atrial flutter increase risk of stroke or cerebrovascular accidents, anticoagulation is usually recommended. Drugs like warfarin, as well as novel oral anticoagulant agents like dabigatran, rivaroxaban, and apixaban, may be used for anticoagulation. [ 58, 59, 60]
What is the most effective method for restoring sinus rhythm?
Electrical cardioversion is the most effective method for restoring sinus rhythm. Synchronized cardioversion starting at 50J can be used immediately in patients who are hypotensive, have pulmonary edema, have chest pain with ischemia, or are otherwise unstable.
How often should you see a patient after a radiofrequency catheter ablation?
Patients treated medically should be monitored regularly. Patients cured with radiofrequency catheter ablation are typically seen once in a follow-up examination following the procedure , then as needed for recurrent symptoms.
Why does a cold cause a PSVT?
PSVT can result because of underlying medical conditions or because of foods and medications that are ingested. Caffeine, alcohol, and over-the-counter (OTC) cold medications that contain pseudoephedrine can stimulate and irritate the heart's electrical conduction system and precipitate an episode of PSVT.
How is paroxysmal supraventricular tachycardia (PSVT) diagnosed?
The diagnosis of PSVT is based upon interpretation of the heart rate monitor and electrocardiogram.
What causes paroxysmal supraventricular tachycardia (PSVT)?
The PSVT can cause the atrium to beat more quickly than it should normally (AFib).
What is the best medication for atrial tachycardia?
Depending upon the heart rhythm, medications can be injected intravenously to reset the AV node or to decrease heart muscle excitability. Adenosine is a short-acting medication that is commonly used as a first-line drug to treat PSVT. Other treatment options for other atrial tachycardias include calcium channel blockers, beta blockers, digoxin, and amiodarone.
What is PSVT in medicine?
Paroxysmal supraventricular tachycardia (PSVT) is episodes of rapid heart rate that start in a part of the heart above the ventricles. "Paroxysmal" means from time to time.
What is a lack of accepted safety for use under medical supervision?
There is a lack of accepted safety for use under medical supervision. 2. Has a high potential for abuse. Has a currently accepted medical use in treatment in the United States or a currently accepted medical use with severe restrictions. Abuse may lead to severe psychological or physical dependence. 3.
Is abuse a low potential for abuse relative to those in Schedule 4?
Has a low potential for abuse relative to those in schedule 4. Has a currently accepted medical use in treatment in the United States. Abuse may lead to limited physical dependence or psychological dependence relative to those in schedule 4.
What are the risks of PSVT?
The following increase your risk for PSVT: Alcohol use. Caffeine use. Illicit drug use. Smoking. The cardiac conduction system is a group of specialized cardiac muscle cells in the walls of the heart that send signals to the heart muscle causing it to contract.
What causes a person to have a PSVT?
There are a number of specific causes of PSVT. It can develop when doses of the heart medicine, digitalis, are too high. It can also occur with a condition known as Wolff-Parkinson-White syndrome, which is most often seen in young people and infants . The following increase your risk for PSVT:
What is a paroxysmal supraventricular tachycardia?
Paroxysmal supraventricular tachycardia (PSVT) Paroxysmal supraventricular tachycardia (PSVT) is episodes of rapid heart rate that start in a part of the heart above the ventricles. "Paroxysmal" means from time to time. The intrinsic conduction system sets the basic rhythm of the beating heart by generating impulses which stimulate ...
Why do you need an EPS for PSVT?
An electrophysiology study (EPS) may be needed for an accurate diagnosis and to find the best treatment. Because PSVT comes and goes, to diagnose it people may need to wear a 24-hour Holter monitor. For longer periods of time, another tape of the rhythm recording device may be used.
What is the treatment for a repeat heartbeat?
Long-term treatment for people who have repeat episodes of PSVT, or who also have heart disease, may include: Cardiac ablation, a procedure used to destroy small areas in your heart that may be causing the rapid heartbeat (currently the treatment of choice for most PSVTs) Daily medicines to prevent repeat episodes.
How many BPM is normal for a child with PSVT?
In children, the heart rate tends to be very high. There may be signs of poor blood circulation such as lightheadedness. Between episodes of PSVT, the heart rate is normal (60 to 100 bpm).
Where does the heart rate start from PSVT?
The rapid heart rate from PSVT may start with events that occur in areas of the heart above the lower chambers (ventricles).
How to stop SVT?
You may be able to stop an episode of SVT by using particular movements such as holding your breath and straining as you would during a bowel movement, dunking your face in ice water, or coughing.
What is the test for SVT?
Tests to diagnosis SVT include: Electrocardiogram (ECG). During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes to your limbs. An ECG measures the timing and duration of each electrical phase in your heartbeat. Holter monitor.
What is a supraventricular tachycardia test?
This device detects abnormal heart rhythms and is implanted under the skin in the chest area. If your doctor doesn't find a heart rhythm problem during those tests, you may need other tests, such as: Stress test. For some people, supraventricular tachycardia is triggered or worsened by stress or exercise.
How to diagnose supraventricular tachycardia?
To diagnose supraventricular tachycardia, your doctor will ask questions about your symptoms and your medical history and perform a physical exam. Blood tests are usually done to check for other health conditions that could cause your symptoms, such as thyroid disease.
How does cardioversion work?
Cardioversion may be done using medications or during a heart procedure. In the procedure, a shock is delivered to your heart through paddles or patches on your chest. The current affects the electrical signals in your heart and can restore a normal rhythm. Medications.
Overview
When your heart rhythm isn’t normal or the speed of the heartbeats isn’t right, you might have an arrhythmia. There are different names for different kinds of arrhythmias, depending on where they happen in the heart and what causes the problem. Tachycardia means your heart is beating too fast.
Symptoms and Causes
A problem with your heart’s electrical signals or circuitry causes SVT, but some people may not be aware of what brings on their symptoms. Others have a clear “trigger” like stress or exercise that starts their SVT. Things that can bring about symptoms include:
Diagnosis and Tests
Your healthcare provider will most likely do an electrocardiogram (EKG or ECG). If your provider needs to study your heart for a longer amount of time, they may ask you to wear a heart monitor that records the electrical activity in your heart.
Management and Treatment
You may not need treatment. Some people may feel better after resting more, drinking less coffee or alcohol or after quitting smoking.
Prevention
If your SVT (supraventricular tachycardia) is from causes you can control, you can:
Living With
Lifestyle changes can help with SVT (supraventricular tachycardia). You can:
Management
- Acute management of paroxysmal supraventricular tachycardia (PSVT) includes controlling the rate and preventing hemodynamic collapse. If the patient is hypotensive or unstable, immediate cardioversion with sedation must be performed. If the patient is stable, vagal maneuvers can be used to slow the heart rate and to convert to sinus rhythm. If vaga...
Contraindications
- Patients with symptomatic Wolff-Parkinson-White (WPW) syndrome should not be treated with calcium channel blockers or digoxin unless the pathway is known to be of low risk (long anterograde refractory period). This is because of the potential for rapid ventricular rates should atrial fibrillation or atrial flutter occur, which can result in cardiac arrest. Patients with preexcite…
Medical uses
- Electrical cardioversion is the most effective method for restoring sinus rhythm. Synchronized cardioversion starting at 50J can be used immediately in patients who are hypotensive, have pulmonary edema, have chest pain with ischemia, or are otherwise unstable.
Prognosis
- If atrial fibrillation has been present for longer than 24-48 hours, defer cardioversion until the patient has been adequately anticoagulated to prevent thromboembolic complications. [40, 36, 50, 51, 52, 53, 54, 41]
Diet
- Dietary changes depend on underlying medical problems. Changes in physical activity depend on underlying cardiac problems and other comorbidities.
Treatment
- A cardiologist should be consulted for patients with frequent episodes of paroxysmal SVT, syncope, and/or preexcitation syndromes. Consultation with a cardiologist should also be obtained for patients in whom medical management has failed.
Benefits
- Patient transfer to a center with radiofrequency catheter ablation is reasonable if this therapy is planned. Alternatively, patients can be discharged home and scheduled for outpatient procedures. Exceptions include patients with syncope, profound symptoms, or preexcited atrial fibrillation or atrial flutter.