What are the treatment options for chorioamnionitis?
If your doctor diagnoses chorioamnionitis, he or she may treat you with antibiotics to help treat the infection. However, often the treatment is to deliver the fetus. If the newborn has an infection, he or she will be given antibiotics as well.
Should we treat asymptomatic infants with maternal chorioamnionitis with empirical antibiotics?
Apr 01, 2019 · Maternal chorioamnionitis is diagnosed by the obstetric team and is treated with intravenous broad-spectrum antibiotics. An in-house neonatal hospitalist is available 24 hours per day to attend all high-risk deliveries, including those infants who were exposed to …
Is there a role for research in neonatal chorioamnionitis?
The optimal antibiotic regimen for treatment of clinical chorioamnionitis has not been well-studied and current recommendations are based largely on clinical consensus . Intravenous administration of ampicillin every 6 hours and gentamicin every 8–24 hours until delivery is …
What are the long-term effects of chorioamnionitis in infants?
What Are the Treatment Options? As chorioamnionitis is a serious infection, it needs immediate treatment. Antibiotics are the most common treatment to keep the infection under control. …
What is the treatment for chorioamnionitis?
How is neonatal infection treated?
What is the drug of choice for the treatment of neonatal sepsis?
Why are broad-spectrum antibiotics used for chorioamnionitis?
Can gentamicin and ampicillin be given together?
Ampicillin may reduce the effects of gentamicin if they are mixed in the same IV container or line. When used together, they typically should be administered separately.
Which antibiotics is considered safe to use in neonates?
What is ampicillin used for in newborns?
What does ampicillin cover?
Why is ampicillin used for neonatal sepsis?
What is a Chorio baby?
Is chorioamnionitis an indication for C section?
Can UTI cause chorioamnionitis?
What is the term for an infection of the chorion?
Keywords: Chorioamnionitis, infection, pregnancy, management. Definition. Chorioamnionitis or intraamniotic infection is an acute inflammation of the membranes and chorion of the placenta, typically due to ascending polymicrobial bacterial infection in the setting of membrane rupture.
Where are mycoplasmas found?
While genital mycoplasmas are found in the lower genital tract (vagina and/or cervix) of over 70% of women, their presence in the upper genital tract (uterus or fallopian tubes) and chorioamnion of pregnant women is rare (<5%) in the absence of labor or membrane rupture [41,43].
How to diagnose chorioamnionitis?
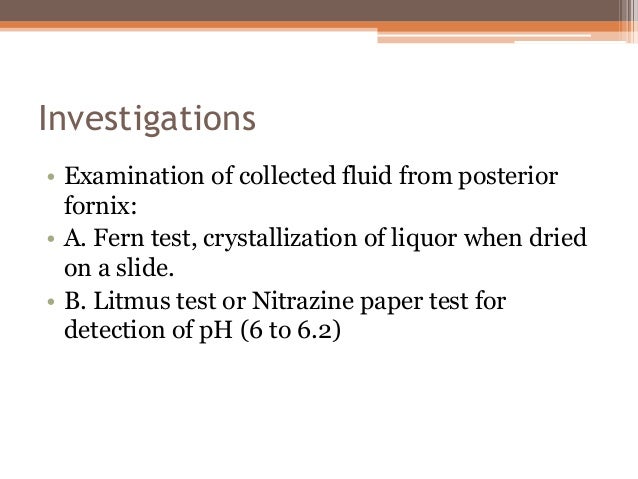
The most common way to diagnose chorioamnionitis is through a physical evaluation to check for the signs and symptoms. Your doctor may order blood culture and urine tests as well. These tests check for the presence of bacteria in your body.
What happens during labor?
You get a lot of vaginal exams during labor. You have a sexually transmitted infection . You have a separate vaginal, urinary, or placental infection. You’re having your first child. You’re having another child and you experienced chorioamnionitis during your first pregnancy. You get epidural anesthesia during labor.
What causes chorioamnionitis in the vagina?
What Causes Chorioamnionitis? Maternal infection is the primary reason for developing chorioamnionitis, and it usually develops in the mother’s vaginal area. The bacteria that causes this kind of serious maternal infection includes anaerobic bacteria, E. coli and group B streptococci.
How to prevent chorioamnionitis?
The best way to prevent chorioamnionitis is to understand the risk factors and make sure you discuss them with your doctor prior to labor and delivery. Risk factors include: Young maternal age, generally less than 21 years old. First pregnancy. Prolonged rupture of membranes (> 18 hours) A long, stressful labor.
What are the symptoms of chorioamnionitis?
The most common symptoms are: Other symptoms may include: Fetal tachycardia. Maternal leukocytosis.
Is chorioamnionitis dangerous?
Chorioamnionitis can be serious. Infants may develop sepsis as a result of the infection, which can be extremely dangerous. A diagnosis of neonatal sepsis is generally made based upon the following symptoms: Weak cries, poor sucking and fatigue. Pulmonary problems, such as respiratory distress, apnea, and cyanosis.
Can chorioamnionitis be seen in the mother?
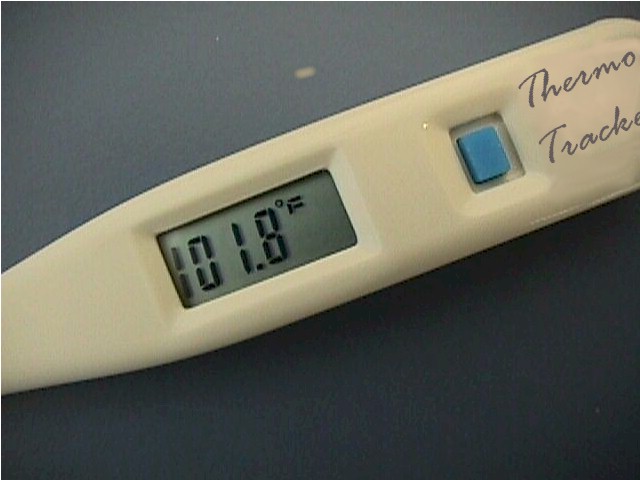
Sometimes there are few or no outward symptoms in the mother. For this reason physicians generally diagnose chorioamnionitis by checking for an increased heart rate in both mom and baby. However, according to the National Institutes of Health (NIH), maternal fever is one of the most prominent indications of chorioamnionitis. Mothers typically have a recurring fever of over 100 F, which is considered abnormal during pregnancy.
Can chorioamnionitis be treated with antibiotics?
In most cases, the mother is given antibiotics, and if needed, the infant may be prescribed antibiotics as well.
Can antibiotics cause chorioamnionitis?
If an infection or chorioamnionitis is caught immediately and the infant is given antibiotics, the infant will usually not have any long-term effects due to chorioamnionitis. However, if the infection is not immediately caught, the child’s side-effects could include: