
Treatment of the calcification
- Physiotherapeutic treatment. The task of physiotherapy procedures, appointed in cases of calcification of bones, joints and muscles: improve circulation and trophism of tissues, as well as relieve pain.
- Alternative treatment. ...
- Surgery. ...
| Treatment | Mechanism of Action |
|---|---|
| Osteoporosis Therapies for Treating Vascular Calcification | |
| Bisphosphonates | Inhibitor of osteoclast formation & survival; calcium phosphate crystal poison |
| Denosumab | Binds RANKL & inhibits binding to RANK |
| Osteoprotegerin | Binds RANKL & inhibits binding to RANK |
How to reverse calcification of the arteries?
In humans, bisphosphonates provide lifesaving therapy for vascular calcification in Enpp1 deficiency, 15 but have not shown any effect on coronary artery or aortic calcification in the general population. 76,77 Studies in CKD and ESRD patients are limited to small studies that suggest a beneficial effect of etidronate, 78–81 but not alendronate 82 on vascular …
What causes calcification in the vasculature?
Vascular Calcification Treatment and Prevention Doctors treat plaque-clogged blood vessels in a variety of ways, including vascular surgery and medicine. Lifestyle changes — quitting smoking, eating healthier foods, and starting to exercise — can decrease the chances of plaque and calcifications forming.
Can calcium buildup in the heart be reversed?
6 rows · Clinically, vascular calcification is now accepted as a valuable predictor of coronary heart ...
What is treatment for calcified arteries?
Mar 02, 2020 · This novel landmark study showed statistically significant attenuation of CAC and aortic valve calcification in patients with ESKD treated with long-term hemodialysis and receiving SNF472 in addition to other standard therapy targeting mineral metabolism disorder.
How is vascular calcification treated?
Accordingly, calcium-free phosphate binders, calcimimetics, and parathyroidectomy, which decrease circulating calcium levels, arrest or prevent vascular calcification, whereas active vitamin D and calcium-containing phosphate binders, which increases calcium levels, promote calcification.Sep 22, 2010
Can you reverse vascular calcification?
These data suggested that vascular calcification, once it occurs, is unlikely to be reversed. Thus, therapeutic interventions that stop and reverse calcification may be of great value to patients with ESRD with vascular disease.Feb 14, 2017
How do you get rid of calcification in the arteries?
How to Reduce Calcium Deposits in Arteries NaturallySmoking cessation will prevent further damage to the internal lining of arteries as well as complications arising from it.Eat a balanced diet composed of all essential nutrients.Exercise can decrease the buildup calcium and cholesterol inside the artery.More items...•Feb 11, 2019
How serious is vascular calcification?
Vascular calcifications are common but potentially serious. They can increase your risk of stroke and blood clots, according to Cardiovascular Research. It's important to learn what causes calcification in the body and how to treat it.Sep 20, 2018
Can calcified arteries be repaired?
There is no current treatment for hardening of the arteries, which is caused by build-up of bone-like calcium deposits, stiffening the arteries and restricting blood flow to organs and tissues.Jun 12, 2019
Can you Stent a calcified artery?
Heavily calcified coronary arteries are the bane of an interventionalist's existence, and can make stent deployment technically difficult to nearly impossible.
What vitamin removes plaque from arteries?
Niacin, or Vitamin B3, is the best agent known to raise blood levels of HDL, which helps remove cholesterol deposits from the artery walls.Nov 28, 2001
What causes vascular calcification?
Vascular calcification is associated with atherosclerosis, diabetes, certain heredity conditions, and kidney disease, especially CKD. Patients with vascular calcification are at higher risk for adverse cardiovascular events. Vascular calcification affects a wide variety of patients.
What is medial calcification?
Medial calcification is an extracellular event initiated by deposition of hydroxyapatite on elastin fibers. (1) The first step in this process is the formation of CaHPO4, which can be reduced by lowering phosphate concentrations. (2) Thiosulfate may inhibit this reaction by forming ion pairs with calcium ions.
Does calcitriol increase calcification?
Second, calcitriol and calcitriol analogues may increase medial calcification, either through direct actions on vascular smooth muscle or by raising circulating calcium levels. Lastly, smooth muscle-specific factors that promote and inhibit calcification are not addressed by this strategy.
Does hypercalciuria cause vascular calcification?
The hypercalciuria could be preventing vascular calcification through negative calcium balance , but this is unlikely without a long-term reduction in serum calcium or increase in parathyroid hormone. Not surprisingly, the serum anion gap increased with a drop in bicarbonate concentration and pH.
Does magnesium inhibit hydroxyapatite formation?
6 Magnesium also inhibits hydroxyapati te formation and could be an effective substitute for calcium in phosphate binders.
Is pyrophosphate safe for calcification?
A seemingly safe way to do this would be to use calcification inhibitors normally present in vascular smooth muscle, of which pyrophosphate is the most feasible. Although pyrophosphate prevents medial calcification in vitamin D-toxic rats,3 very high doses are required because of rapid hydrolysis to orthophosphate.
Does thiosulfate prevent calcification?
Thiosulfate completely prevented calcification in this model at a dose and interval comparable to those used in humans with CUA, thus providing a scientific basis for its clinical use. However, this is a model of large-artery calcification, not CUA, and the pathogenesis may not be the same.
Does PPI inhibit calcification?
Large doses of PPi have been shown to inhibit vascular calcification in vitamin D-toxic rats. (4) PP i is hydrolyzed by tissue-nonspecific alkaline phosphatase (TNAP) on the smooth muscle membrane, and this could be targeted by newly developed TNAP inhibitors.
What is vascular calcification?
Vascular calcifications are mineral deposits on the walls of your arteries and veins. These mineral deposits sometimes stick to fatty deposits, or plaques, that are already built up on the walls of a blood vessel.
What is calcification in blood vessels?
Vascular calcifications are mineral deposits on the walls of your arteries and veins. These mineral deposits sometimes stick to fatty deposits, or plaques, that are already built up on the walls of a blood vessel.
How to treat a clogged blood vessel?
Vascular Calcification Treatment and Prevention. Doctors treat plaque-clogged blood vessels in a variety of ways, including vascular surgery and medicine. Lifestyle changes — quitting smoking, eating healthier foods, and starting to exercise — can decrease the chances of plaque and calcifications forming. If you take calcium supplements, your ...
What is UPMC heart and vascular?
The UPMC Heart and Vascular Institute has long been a leader in cardiovascular care, with a rich history in clinical research and innovation. As one of the first heart transplant centers in the country and as the developer of one of the first heart-assist devices, UPMC has contributed to advancing the field of cardiovascular medicine.
What is calcification in breast?
In the body, calcification is actually part of the aging process. Calcifications accumulate in the vessels, heart, or valves as calcium travels through the bloodstream.
Where does calcification occur?
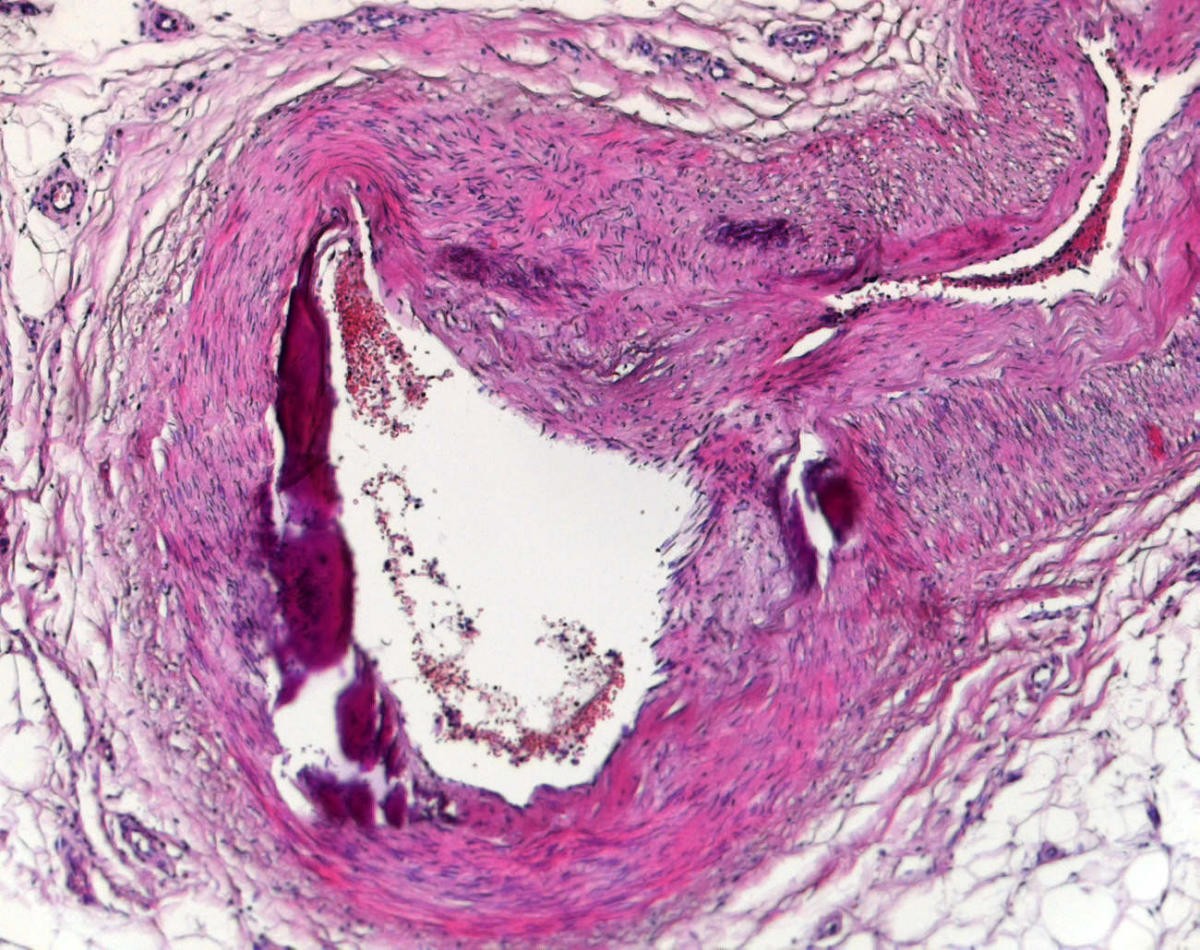
Calcifications can occur in the intimal (inside) or medial (middle layer) part of the blood vessel. Each location has different associated risks. Medial calcifications, for example, are most often associated with kidney disease, diabetes, hypertension, and advanced age.
Can vascular calcification cause stroke?
You may not always notice symptoms of vascular calcification. If vascular calcification causes arteries to harden, the heart will have to work harder to pump blood. Eventually, you might develop symptoms of peripheral artery disease (PAD) or stroke.
What is a CUA?
Calcific Uremic Arteriolopathy. Calcific uremic arteriolopathy (CUA), formerly known as calciphylaxis, is a severely morbid and life-threatening form of medial vascular calcification that leads to cutaneous necrosis and panniculitis.
How does aortic calcification affect heart failure?
Aortic calcification promotes congestive heart failure by eroding compliance and elastance. The hemodynamic demands of the cardiovascular system require that the aorta store energy in its elastance during systole and release it during diastole, which minimizes cardiac work and is the basis for balloon counterpulsation. This function, known as Windkessel physiology, is reflected in the high density of elastin in the arch, where mechanical energy is highest. Its loss is detectable as increased arterial pulse wave velocity in calcified arteries, resulting in thoracic summation of reflected and orthograde pressure waves, thereby increasing systolic and pulse pressures. It also increases cardiac work, promoting heart failure, left ventricular hypertrophy, and diastolic dysfunction, independently of atherosclerosis, aging, or diabetes. The link between aortic rigidity and heart failure is most evident in the hypertensive cardiomyopathy observed in patients with idiopathic infantile arterial calcification and in animal models with aortic banding.
What is the most extensive vascular calcification?
91 The most extensive vascular calcification is found in patients with arterial medial calcification, a highly characteristic feature of type 2 diabetes mellitus 92 and chronic kidney disease. 93 Arterial medial calcification was once considered benign because it was neither stenotic nor thrombogenic. It is now recognized that arterial medial calcification is associated with higher cardiovascular mortality and risk of amputation in type 2 diabetes mellitus 94,95 and in end-stage kidney disease. 96 There is growing evidence for heterogeneous mechanisms within the category of medial calcification. For example, hydroxyapatite is the predominant mineral in diabetic arterial medial calcification , but in vitamin D toxicity, it is whitlockite. 97
What are the factors that contribute to bone vascular interactions?
Some possible contributors to bone-vascular interactions include osteopontin, fibroblast growth factor (FGF)-23, phosphate/PTH, and vitamin D. Osteopontin release from bone may represent a major component of the bone-vascular axis.
What is the aortic valve?
The aortic valve der ives from embryonic neural crest cells, which are regulated by Wnt signaling. This ontogenetic history of aortic valve cells may influence their responses to mechanical and metabolic stress and account for differences between the 2 types of valves.
What is the most common form of calcific vasculopathy?
Atherosclerotic calcification, the most common form of calcific vasculopathy, appears to result from induction of osteogenic differentiation in subpopulations of vascular cells by inflammatory factors, such as modified lipoproteins and cytokines, that are found in atheromatous components of plaque.
Is vascular calcification a predictor of heart disease?
Clinically, vascular calcification is now accepted as a valuable predictor of coronary heart disease. 153 Achieving control over this process requires understanding mechanisms in the context of a tightly controlled regulatory network, with multiple, nested feedback loops and cross talk between organ systems, in the realm of control theory. Thus, treatments for osteoporosis such as calcitriol, estradiol, bisphosphonates, calcium supplements, and intermittent PTH are likely to affect vascular calcification, and, conversely, many treatments for cardiovascular disease such as statins, antioxidants, hormone replacement therapy, angiotensin-converting enzyme inhibitors, fish oils, and calcium channel blockers may affect bone health. As we develop and use treatments for cardiovascular and skeletal diseases, we must give serious consideration to the implications for the organ at the other end of the bone-vascular axis.
What are the symptoms of calcification?
At times, any of these symptoms can be severe: Bone pain. Bone spurs (occasionally visible as lumps under your skin) Breast mass or lump. Eye irritation or decreased vision.
What is calcification in musculoskeletal disease?
Calcification can be part of a normal healing response to musculoskeletal injuries. Calcifications are often found in arteries affected by arteriosclerosis (hardening of the arteries), in benign and malignant breast processes, at sites of bone or cartilage injury, and sometimes within cancers.
What does a calcification on a mammogram mean?
Calcifications that are apparent on mammograms may signal the presence of breast cancer, or they may occur with benign breast disease.
What is calcification in the body?
What is calcification? Calcification is a gradual accumulation of calcium in an area of your body tissue. Most of the calcium absorbed by your body ends up in your bones and teeth, where it is most needed.
Why is my calcium level abnormal?
Sometimes blood calcium levels become abnormal, signaling the presence of a metabolic disorder in which your body’s ability to use or regulate the level of calcium is compromised. Seek immediate medical care (call 911) for serious symptoms, such as severe headache, severe bone pain, or sudden abdominal, pelvic, or lower back pain.
Is calcification a serious condition?
In some cases, calcification can be part of a serious condition that should be immediately evaluated in an emergency setting. Seek immediate medical care (call 911) if you, or someone you are with, have complications of calcification, including kidney stones, Paget’s disease (abnormal bone tissue loss and reformation), pineal gland tumors, or severe hypercalcemia (excess calcium in the blood), and experience any of these serious symptoms including:
Can calcification be detected on X-rays?
Instead, calcification is most frequently discovered on X-rays, including mammograms, for example. Some calcification is normal, but even disease-related calcification may not cause symptoms that you will detect. You may, however, feel the effects of the underlying disorder or process that results in calcification.
What does vascular calcification mean?
Vascular calcification is the pathological deposition of mineral in the vascular system. It has a variety of forms, including intimal calcification and medial calcification, but can also be found in the valves of the heart.
Can atherosclerosis be cured?
Bits of plaque can break loose and cause blood clots that may lead to heart attack or stroke. There is currently no cure for atherosclerosis, but the condition can be slowed with statin drugs and dietary changes.
What are the long term effects of atherosclerosis?
Over time, plaque hardens and narrows your arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body. Atherosclerosis can lead to serious problems, including heart attack, stroke, or even death.
What is the main cause of atherosclerosis?
Development of atherosclerosis If you have too many cholesterol particles in your blood, cholesterol may accumulate on your artery walls. Eventually, deposits called plaques may form. The deposits may narrow — or block — your arteries. These plaques can also burst, causing a blood clot to form.
How does atherosclerosis affect older adults?
But as you get older they might harden, as plaque — made up of cholesterol, fat, calcium, and fibrous tissue — builds up within them, narrowing the vessels. This process, called atherosclerosis, puts you at risk for heart attacks, strokes, and peripheral artery disease.
What does atherosclerosis mainly affect?
This fatty buildup can cause partial or complete blockage of blood flow through an artery. Atherosclerosis mainly affects medium-sized arteries, such as the coronary (heart), carotid (neck), cerebral (brain) and renal (kidney) arteries. It can also be found in the aorta, which is the largest artery in the body.
What is the end stage of atherosclerosis?
The last stage of atherosclerosis occurs when the plaque breaks open, exposing the cholesterol and tissue underneath. Blood clots form in response to this rupture and cause symptoms of a heart attack and unstable angina.
