
Medication
Treatment for ventricular tachycardia involves managing any disease that causes the condition. These treatments may improve or prevent the abnormal heart rhythm from returning. In emergency situations, CPR, electrical defibrillation and IV medications may be needed to slow the heart rate.
Procedures
Supraventricular tachycardia, or SVT, is a type of rapid heartbeat that begins in the upper chambers of the heart. Most cases don't need to be treated. They go away on their own. But if an episode doesn't end within a few minutes, you may need to take action. You might do this on your own or with the help of a doctor.
Therapy
They include:
- Valsalva maneuver. This is a way to increase pressure in the abdomen and chest. ...
- Carotid massage. Your healthcare provider may rub the carotid artery in your neck. ...
- Medicine. There are various kinds you can take. ...
- Electrocardioversion. This is a shock to the heart to restart a normal rhythm right away. ...
- Catheter ablation. This can help cure SVT. ...
Nutrition
- Atrial or supraventricular tachycardia (SVT) begins in the upper chambers of the heart. ...
- Sinus tachycardia may be caused by a fever, anxiety, medication or recreational drugs, fright, strenuous exercise, or severe emotional distress. ...
- Ventricular tachycardia begins in the lower chambers of the heart and can be life-threatening. ...
See more
What is ventricular tachycardia and how is it treated?
Can supraventricular tachycardia be cured without surgery?
What is the best drug treatment for SVT?
How do you treat ventricular tachycardia?
What is the treatment for unstable SVT?
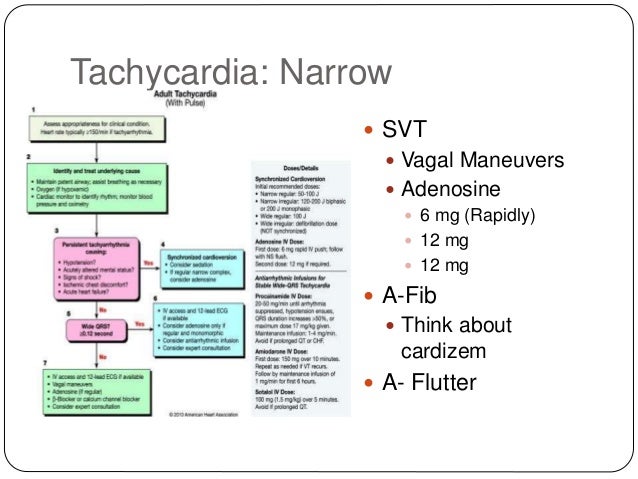
Synchronized cardioversion is recommended (moderate-quality evidence) for the termination of any hemodynamically unstable SVT. In the absence of hemodynamic compromise, SVT should be treated (moderate-quality evidence) with synchronized cardioversion when pharmacologic therapy is ineffective or contraindicated.
What is the first line treatment for stable SVT?
Vagal maneuvers are an appropriate first treatment option in patients with hemodynamically stable SVT. Studies report an approximately 25% success rate, although reported rates vary widely in the literature (6%-54%). The most commonly performed maneuvers are the Valsalva maneuver and carotid sinus massage.
What is the drug of choice for supraventricular tachycardia?
In most patients, the drug of choice for acute therapy is either adenosine or verapamil. The use of intravenous adenosine or the calcium channel blocker verapamil are considered safe and effective therapies for controlling SVTs.
Do beta-blockers cure SVT?
Medications typically used to treat SVT are: Beta Blockers: A beta blocker is a very safe medication that works by reducing the effect adrenalin has on the heart. Beta blockers are commonly used to treat high blood pressure and other common heart problems. Calcium Channel Blockers.
What triggers SVT episodes?
SVT is usually triggered by extra heartbeats (ectopic beats), which occur in all of us but may also be triggered by: some medications, including asthma medications, herbal supplements and cold remedies. drinking large amounts of caffeine or alcohol. stress or emotional upset.
What is unstable tachycardia?
An unstable tachycardia exists when cardiac output is reduced to the point of causing serious signs and symptoms. Serious signs and symptoms commonly seen with unstable tachycardia are: chest pain, signs of shock, SOA (short of air), altered mental status, weakness, fatigue, and syncope.
Which beta blocker is best for tachycardia?
Arrhythmias: bisoprolol and metoprolol succinate are often preferred. Beta-blockers are the first-line treatment for long-term symptomatic rate control in patients with a range of cardiac arrhythmias, including atrial fibrillation and ventricular tachycardia.
How is supraventricular tachycardia treated?
How is supraventricular tachycardia (SVT) treated? Your treatment for SVT depends on a few things. They include what type of SVT, how often you have episodes, and how severe your symptoms are. The goals of treatment are to prevent episodes, relieve symptoms, and prevent problems.
What is the treatment for recurring SVT?
Ongoing treatment of recurring SVT. If you have recurring episodes of SVT, you may need to take medicines, either on an as-needed basis or daily. Medicine treatment may include beta-blockers, calcium channel blockers, or other antiarrhythmic medicines.
How to tell if you have SVT?
SVT is usually treated if: 1 You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. 2 Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
What to do if your heart rate is not slowed?
If your heart rate cannot be slowed using vagal maneuvers, you may have to go to your doctor's office or the emergency room, where a fast-acting medicine can be given to slow your heart rate. If the arrhythmia does not stop and symptoms are severe, you may need a procedure called electrical cardioversion to reset your heart rhythm.
What is an electric shock to the heart called?
Other treatment. An electric shock to the heart is called electrical cardioversion. It may be needed if you are having severe symptoms of SVT and your heart rate doesn't go back to normal using vagal maneuvers or fast-acting medicines. Types.
What are the symptoms of SVT?
SVT is usually treated if: You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
How to treat sudden onset SVT?
Your doctor will teach you how to do these safely. These are things such as bearing down or putting an ice-cold wet towel on your face.
What is a supraventricular tachycardia?
Supraventricular tachycardia (SVT) is an arrhythmia initiated above the ventricles, at or above the atrioventricular (AV) node. This cardiac rhythm occurs due to improper electrical conduction within the heart that disrupts the coordination of heartbeats. Early beats occur within the atria of the heart due to improperly functioning electrical connections, resulting in a rapid heart rate such that the heart does not have enough time to fill the atria with blood before contraction of the atria. This can lead to the patient feeling dizziness or lightheadedness because the brain is not receiving adequate oxygen or blood. The onset of this dysrhythmia is typically sudden, and may be prompted by emotional or physical stress.
What Are ECG Characteristics of Supraventricular Tachycardia?
Typically characterized by having a narrow QRS complex that is less than or equal to 0.12 seconds. A wide QRS (greater than or equal to 0.12 seconds) can occur, but is less common.
What should be done before cardioversion?
Before performing cardioversion, the healthcare provider should ensure the patient has IV access and equipment is at the ready for suctioning, intubation, and measuring oxygen saturation . Contingent on the severity of the patient’s symptoms and how hemodynamically unstable they may be, sedation medication should be administered before initiating cardioversion. If all elements are in place, synchronized cardioversion should then be conducted. Recommendations specific to the cardioverter being utilized should be followed when determining appropriate settings for energy levels during shock delivery. If the patient’s cardiac rhythm remains unchanged following cardioversion, the healthcare provider or team should re-evaluate any potential underlying causes contributing to the patient’s condition. The energy level should then be increased for the next attempt at cardioversion.
What is ACLS electrical cardioversion?
The ACLS Electrical Cardioversion Algorithm provides guidance for healthcare providers performing cardioversion. A symptomatic and unstable patient with a heart rate of 150 beats per minute or more, with a cardiac rhythm such as supraventricular tachycardia, warrants synchronized cardioversion. Synchronized cardioversion coordinates shock delivery to the patient, where the device analyzes the patient’s cardiac rhythm in order to deliver a shock that is synchronized with the R wave in the QRS complex. This coordinated delivery can result in a delay before the cardioverter delivers the shock, due to the time needed for the device to analyze the patient’s cardiac rhythm.
What is the purpose of the Valsalva maneuver?
The Valsalva maneuver is an example of a vagal maneuver intended to stimulate the parasympathetic nervous system. This results in a slowing of the development of an impulse at the sinus node of the heart, which then reduces the speed of conduction at the AV node, extending the refractory period at the AV node, and decreasing the force of ventricular contractions. The Valsalva maneuver is completed by a patient modifying their breathing, where they exhale against the glottis, holding this for 10-15 seconds. The patient can do this by bearing down as if they were to have a bowel movement, blowing through a straw or syringe, or applying cold water or ice packs to their face.
Can adenosine be used for tachycardia?
If the patient with supraventricular tachycardia is symptomatic and unstable, and the ECG reading indicates a regular, narrow, QRS complex (as is common with supraventricular tachycardia), adenosine can be used in addition to synchronized cardioversion. Six milligrams of adenosine should be administered intravenously as an initial dose. If a second dose of adenosine is needed, 12 mg of adenosine may be administered intravenously. Each dose of adenosine should be given rapidly (as it is intended as a means of pharmacologic or chemical cardioversion) and followed by a normal saline flush.
Is 150 beats per minute considered a symptomatic tachycardia?
If a patient is experiencing symptomatic tachycardia with a heart rate of 150 beats per minute or more and is considered symptomatically and hemodynamically unstable, they are a candidate for cardioversion. However, patients may be symptomatic at heart rates less than 150 beats per minute, most notably if they have pre-existing cardiovascular disease or other potential risk factors or contributing causes as discussed above. Therefore, the healthcare provider must understand when cardioversion should be used, the medications indicated for cardioversion, how to properly prepare the patient for cardioversion, and how to utilize the cardioverter.
What are the signs of unstable tachycardia?
Identifying clinical stability depends on the cause of the tachycardia. Some say that cardiac-related symptoms (chest pain, shortness of breath, etc.) are significant indicators of unstable tachycardia. That is more true in the hospital setting than in the field, as more treatment options are available to hospitalized patients.
What is the primary factor to consider when considering tachycardia?
Outside of a hospital, the primary factor to consider is hemodynamic stability —that is, the stability of blood flow from the heart to the brain. When there is hemodynamically unstable tachycardia, the chambers of the heart do not have enough time to fill with blood between contractions.
Why isn't a 12-lead ECG available?
One reason not to treat tachycardia unless it's hemodynamically unstable is because of the possibility of treating a wide-complex tachycardia as ventricular tachycardia when it is not. Taking that chance when the patient is in significant danger of cardiac arrest is acceptable. ...
How fast does tachycardia get?
Below, we will discuss narrow-complex versus wide-complex tachycardia, but for now, just know that a wide-complex tachycardia gets worrisome once it's faster than 150 bpm. 2 A narrow-complex tachycardia can be a little faster, but consider it concerning if it is over 160 bpm. 3
What is considered a tachycardia?
Tachycardia is generally defined as anything faster than 100 beats per minute (bpm) when resting, but not all tachycardias are clinically significant. Without an ECG monitor, a good rule of thumb is to be concerned if the patient has a pulse rate greater than 150 bpm, or if a radial pulse is irregular, weak, or absent. 1
What is tachycardia in 2021?
Updated on May 16, 2021. Tachycardia (rapid heart rate ) is one of the more complicated dysrhythmias to treat because it has so many presentations and so many causes. This article focuses on the treatment of cardiac-related unstable tachycardia in the emergency setting by prehospital professionals.
Where is the pacemaker located in tachycardia?
Aggressively treating wide-complex tachycardia when the patient is hemodynamically stable is not worth the risk. 2. The area of the heart where the impulse originates is known as the pacemaker because whatever area generates the impulse also sets the pace of the heartbeats. The sinus node is located in the left atrium.
Overview
When your heart rhythm isn’t normal or the speed of the heartbeats isn’t right, you might have an arrhythmia. There are different names for different kinds of arrhythmias, depending on where they happen in the heart and what causes the problem. Tachycardia means your heart is beating too fast.
Symptoms and Causes
A problem with your heart’s electrical signals or circuitry causes SVT, but some people may not be aware of what brings on their symptoms. Others have a clear “trigger” like stress or exercise that starts their SVT. Things that can bring about symptoms include:
Diagnosis and Tests
Your healthcare provider will most likely do an electrocardiogram (EKG or ECG). If your provider needs to study your heart for a longer amount of time, they may ask you to wear a heart monitor that records the electrical activity in your heart.
Management and Treatment
You may not need treatment. Some people may feel better after resting more, drinking less coffee or alcohol or after quitting smoking.
Prevention
If your SVT (supraventricular tachycardia) is from causes you can control, you can:
Living With
Lifestyle changes can help with SVT (supraventricular tachycardia). You can:
What to do if you have a SVT?
If the SVT episode continues, you should go to the emergency room. There, you might be given a medicine called adenosine, which also slows the electrical impulses in the heart, or another medicine called verapamil. In rare cases, you might require an electrical shock to get your heart back into a normal rhythm.
What is the procedure for SVT?
Ablation Therapy: Ablation can be considered as a primary, first-line therapy for certain types of SVT, and it may also be considered if you often have symptoms with medical therapy. During an ablation, a small tube called a catheter is placed through a vein typically in your leg, then guided to your heart. An electrical study is done to find the area in your heart causing the electrical problems that trigger SVT. Your doctor then destroys this area either by burning or freezing that part of the heart.
What are the symptoms of SVT?
Common symptoms are palpations, dizziness, chest pain, and feeling like you are about to faint. Treatment for SVT includes drug therapies and catheter ablation. What type of therapy is best for you depends on the type of SVT you have, how often it occurs, and the degree and length of symptoms.
How to stop sudden heart failure?
The initial treatment for a sudden episode of SVT is vagal maneuvers, such as bearing down, coughing, or holding your breath. These actions can slow the electrical impulses in your heart and may stop the SVT.
Is ablation a good treatment for SVT?
Ablation is very successful in treating specific forms of SVT. However, ablation therapy does have some rare, but serious procedural risks. Be sure to talk about the procedure and its risks with your physician. Together with your health care team, you will find a treatment that is right for you. Last Edited 05/31/2018.
Can you get SVT without symptoms?
In most cases, if you experience short episodes of supraventricular tachycardia (SVT) with no symptoms, your health care professional may recommend no therapy. However, if you do have symptoms, frequent episodes, or both, then you will likely require treatment.
Does drug therapy help with SVT?
Also, the risk of side effects from drug therapy should be weighed against the risks and benefits of ablation. Drug Therapy: Patients are prescribed daily medications to help prevent SVT episodes from occurring or to slow heart rates during SVT episodes.
What is a supraventricular tachycardia?
Supraventricular tachycardias are usually narrow-complex tachycardias with a QRS interval of 100 ms or less on an electrocardiogram (ECG). Occasionally, they may show a wide QRS complex in the case of a pre-existing conduction delay, an aberrancy due to rate-related conduction delay or a bundle branch block.
When is synchronized cardioversion recommended?
Synchronized cardioversion is recommended for acute treatment in patients with hemodynamically stable SVT when pharmacologic treatment is ineffective or contraindicated ( class I recommendation, level B-NR evidence)
What does AVNRT mean on an electrocardiogram?
AVNRT = atrioventricular nodal re-entrant tachycardia, AVRT = atrioventricular re-entrant tachycardia.
What level of evidence is needed for SVT?
Patients with SVT should be educated on how to perform vagal manoeuvres for ongoing management of SVT (class I recommendation, level C-LD evidence)
What is the best treatment for a symtomatic sinus rhythm?
Oral β-blocker, diltiazem or verapamil treatment is useful for ongoing management in patients with symptomatic SVT who do not have ventricular pre-excitation during sinus rhythm (class I recommendation, level B-R evidence)
How fast does a ventricular rate vary in SVT?
Understanding the underlying mechanism is useful in understanding the clues on ECG. Ventricular rates in SVT may vary from 150 to 250 beats/min. However, the rate may be slower in older patients and in patients taking AV nodal blocking medications (i.e., calcium-channel blockers, β-blockers and digoxin).7
Is an electrophysiologic study reasonable in asymptomatic patients with pre-excitation to stratify risk for?
An electrophysiologic study is reasonable in asymptomatic patients with pre-excitation to stratify risk for arrhythmic events (class IIa recommendation, level B-NR evidence)
What is supraventricular tachycardia?
Supraventricular tachycardia (SVT) is a common cause of hospital admissions and can cause significant patient discomfort and distress. The most common SVTs include atrioventricular nodal re-entrant tachycardia, atrioventricular re-entrant tachycardia and atrial tachycardia. In many cases, the underlying mechanism can be deduced from ...
Which type of tachycardia is highly sensitive to termination with vagal manoeuvre?
Atrioventricular nodal re-entrant tachycardia and atrioventricular re-entrant tachycardia are re-entrant tachycardias involving the atrioventricular node and are therefore highly sensitive to termination with vagal manoeuvres and administration of adenosine.
How to administer adenosine challenge?
If unsuccessful, and depending on the clinical setting, an adenosine challenge can be administered via a large peripheral/central vein as a bolus immediately followed by a 10 mL rapid saline flush. Delivery to the myocardium must be swift as the half-life of adenosine is less than 10 seconds. Adenosine acts directly on the AV node Gi-coupled A1receptors, hyperpolarising the cell membrane, slowing and usually inhibiting AV nodal conduction.13This is a crucial diagnostic manoeuvre and a continuous ECG / rhythm strip should be recorded during administration. One of three responses may occur (Fig (Fig3).3). If no change is seen, either the dose/delivery of adenosine was inadequate or rarely, the diagnosis is VT in which the AV node plays no part. A sudden termination is suggestive of AVNRT or AVRT as the AV node is a critical part of the circuit in both; the mean dose of adenosine required for termination is 6 mg. The presence of P-waves with AV dissociation is diagnostic of AT; termination of AT with adenosine is unusual but favours a focal over a re-entrant mechanism.14
What is AVNRT in cardiac?
AVNRT is the most common SVT in the general population and accounts for over 60% of patients undergoing invasive cardiac electrophysiology study .5It is facilitated by the presence of two functionally distinct electrophysiological tracts of differing conduction velocities and refractory periods within the AV node: a fast pathway and a slow pathway. An atrial (or less commonly a ventricular) premature beat is required to initiate repetitive re-entry between the fast and slow pathways, manifest on the surface ECG as a narrow QRS tachycardia in the absence of bundle branch block.
Where does tachycardia originate?
Atrial tachycardia. Atrial tachycardia (AT) originates within the atrium and is oblivious to the behaviour of the AV node. On surface ECG, the P-waves appear monomorphic with a stable tachycardia cycle length, but morphologically distinct from the sinus P-wave.
Is tachycardia antegrade or retrograde?
Less commonly, antidromic tachycardia can occur where the AP conducts antegradely and the node provides the retrograde limb of the tachycardia as it re-enters the atrium from the ventricle via the His–Purkinje network; the QRS complex therefore appears broad and fully pre-excited. The P-waves are often difficult to see as they are buried in the ST segments and it can be difficult to differentiate antidromic AVRT from ventricular tachycardia (VT). The presence of pre-excitation during sinus rhythm recordings favours the former diagnosis.
Is catheter ablation recommended for tachycardia?
Catheter ablation is strongly recommended in the event of a high-risk pathway being diagnosed. Conclusion. Supraventricular tachycardia is a common cause of hospital attendance and acute admission. With close inspection of the ECG in sinus rhythm at the time of onset, offset and during tachycardia, a diagnosis can often be formulated.
What is SVT in ventricular?
SVT is a broad term for a number of tachyarrhythmias that originate above the ventricular electrical conduction system (Purkinje fibers). Classic Paroxysmal SVT has a narrow QRS complex & has a very regular rhythm. Inverted P waves are sometimes seen after the QRS complex. These are called retrograde p waves.
What voltage is used for SVT?
Unstable patients with SVT and a pulse are always treated with synchronized cardioversion. The appropriate voltage for cardioverting SVT is 50-100 J. This is what AHA recommends and also SVT converts quite readily with 50-100 J.
What is a vagal maneuver?
A: A vagal maneuver is a technique by which you attempt to increase intrathoracic pressure which stimulates the vagus nerve. This can result in slowed conduction of electrical impulses through the AV node of the heart. The following methods can be used. Cough Method: Have a patient cough forcefully.
What is the inverted wave of the heart called?
Inverted P waves are sometimes seen after the QRS complex. These are called retrograde p waves. The heart fills during diastole, and diastole is normally 2/3 the cardiac cycle. A rapid heart rate will significantly reduce the time which the ventricles have to fill.
What is the abdominal pressure method?
Abdominal Pressure Method: Press into the patient’s abdomen while they contract and resist pressing into their abdomen.
Home remedies
If you feel your heart starting to race with an SVT episode, vagal maneuvers that stimulate the vagus nerve can help control your heart rate and other important functions.
Medications
Medications can help slow down a racing heart if your SVT episodes are frequent and last long, or if they’re causing symptoms such as:
Ablation
For people with recurrent SVT, including children, ablation is considered generally safe and effective. According to a 2015 study, this is true even if you’re taking SVT medications, or you choose not to take medications in the long term.

Diagnosis
Lifestyle and Home Remedies
Alternative Medicine
Preparing For Your Appointment