
Treatment for ulcerative colitis can include medicine, changes in your diet, or surgery. These treatments won't cure your ulcerative colitis, unless you have surgery that removes the colon and rectum, which is considered curative, but they can help ease your symptoms.
Can We really cure ulcerative colitis?
Apr 10, 2022 · Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning . In most people, this is achieved by taking medication such as: aminosalicylates corticosteroids immunosuppressants Mild to moderate flare-ups can usually be treated at home.
What are the natural remedies for ulcerative colitis?
Medications and certain lifestyle changes can help reduce the intensity and frequency of UC flares. Currently, surgery to remove the colon is the only full …
Will natural remedies ease ulcerative colitis?
Oct 08, 2021 · These medications, including Azulfidine (sulfasalazine) and Asacol HD , are used to treat mild-to-moderate ulcerative colitis flares and can also be used as a maintenance treatment while in remission. Corticosteroids: These medications, including prednisone and Entocort EC , also help to suppress immune system inflammation. They are used only as a …
Is there any permanent cure for ulcerative colitis?
Feb 25, 2021 · Aminosalicylates work best for mild-to-moderate UC, and they can help prevent flare-ups. The American Gastroenterological Association (AGA) strongly recommends that adults with extensive...
How would a flare up of ulcerative colitis be treated?
Your doctor may prescribe suppositories and enemas. Some drugs, like corticosteroids and “5-ASAs,” can quickly get your UC inflammation under control. For day-to-day care, you might take 5-ASAs and meds that curb your immune system, such as azathioprine or 6-MP. Sometimes doctors also prescribe “biologic” drugs for UC.Nov 1, 2021
How do you get rid of a colitis flare fast?
Managing flare-upsKeep a food journal. Write down everything you eat and drink to identify items that may trigger your flare-ups. ... Limit your fiber intake. ... Eat smaller meals. ... Exercise. ... Reduce stress. ... Speak with your doctor.
What is the most common treatment for ulcerative colitis?
The proctocolectomy and ileoanal pouch (also called J-pouch surgery) is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy — a procedure that removes your colon and rectum.Apr 23, 2020
How long does it take for an ulcerative colitis flare up to clear?
Articles On When Ulcerative Colitis Treatment Stops Working Flare-ups might take days or weeks. Remission might last for months or even years. You may go from a mild flare-up to a severe one and back again. Or, it may get more advanced and spread to other parts of your colon.Nov 1, 2021
What to eat to stop a colitis flare up?
low fiber fruits (like bananas, honeydew melon, and cooked fruits) lean protein (such as seafood, chicken, eggs, and firm tofu) refined grains (including oatmeal, white rice, and sourdough bread) cooked vegetables without seeds or skins (such as asparagus tips, potatoes, and cucumbers)Apr 28, 2021
How do you calm inflamed intestines?
If a person has recovered from a flare of intestinal or colonic inflammation, they could eat the following foods to help keep inflammation lowered:Fiber. ... Omega-3 fatty acids. ... Natural foods. ... Dairy and lactose products. ... Added fats. ... Eat protein. ... Drink enough fluids.Apr 15, 2021
What medications should be avoided with ulcerative colitis?
A person with UC should avoid taking:Nonsteroidal anti-inflammatory drugs (NSAIDs) NSAIDs are common medications that people use to relieve pain, inflammation, and fevers. ... Some antibiotics. Doctors use antibiotics to treat diseases that bacteria cause. ... Some ingredients in supplements. ... Some live vaccines. ... Other medications.Aug 16, 2021
What is the safest medication for ulcerative colitis?
In cases of mild-to-moderate disease severity, mesalamine is preferred as it is the safest available drug for the management of UC with a 0.2% risk of interstitial nephritis.Apr 29, 2019
What are the side effects of mesalamine?
Side effects of mesalamine include:abdominal pain.abdominal discomfort.headache.gas (flatulence)nausea.fatigue.a general feeling of discomfort.weakness.More items...
When should you go to the hospital for ulcerative colitis?
Call your healthcare provider immediately if you notice your loved one is having more than six bowel movements per day that include a lot of blood, accompanied by any one of the following: a fast heart rate, a fever, a low temperature, and signs of anemia (such as feeling tired and shortness of breath).Jul 26, 2021
When does ulcerative colitis require hospitalization?
Ulcerative colitis is an inflammatory bowel disease that can be life-threatening when the symptoms flare up. You need ulcerative colitis hospitalization if you have more than six bowel movements per day, blood in your stool, high temperature and heart rate, and severe abdominal pain.Nov 30, 2021
How do I know if my ulcerative colitis is flaring?
Most people with ulcerative colitis (UC) have periods of active symptoms, and these are known as flares, or flare-ups....Symptomsabdominal pain.urgent, painful bowel movements.tiredness.dehydration.fever.bloody bowel movements.diarrhea, which often includes pus.Sep 21, 2020
How to get rid of ulcerative colitis?
Manage stress. While stress doesn't cause ulcerative colitis, it may make your symptoms worse and may trigger flare-ups. Exercise may help reduce tension and keep your bowels functioning well. Focus on activities you like, such as biking, walking, yoga and swimming .
What is ulcerative colitis flare up?
An ulcerative colitis flare-up is the return of symptoms after a period of remission. This may involve diarrhea, abdominal pain and cramping, rectal pain and bleeding, fatigue, and urgent bowel movements. Although you may feel helpless against these fluctuations, changes in your diet and lifestyle may help control your symptoms and lengthen ...
What foods can you eat to help ulcerative colitis?
However, if you have ulcerative colitis, these foods may make your symptoms worse. Steer clear of nuts, seeds, corn and popcorn, and see if you notice a difference in your symptoms.
Can eating dairy cause ulcerative colitis?
Skip the dairy aisle. There's no firm evidence that diet causes ulcerative colitis. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up. Dairy foods are one possible culprit. Try limiting or eliminating milk, yogurt, cheese, ice cream and other dairy products.
What is it called when you have no symptoms?
This period of minimal or no symptoms is called remission . People with ulcerative colitis often have certain triggers that can cause flare-ups of the disease. The key to dealing with a flare is knowing what caused it and how to fix it.
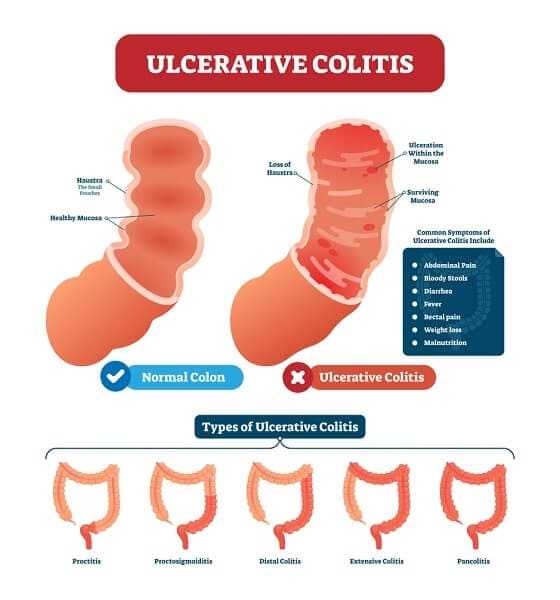
What is ulcerative colitis?
When to see a doctor. Takeaway. Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD). It causes inflammation and sores, called ulcers, in your large intestine. Symptoms of ulcerative colitis typically get worse over time, but they also may disappear for a short or long interval. This period of minimal or no symptoms is called ...
How to stop UC flares?
How to stop flares. You can’t completely prevent flares without surgery, but you can work to manage them and reduce symptoms when they occur. Medications and certain lifestyle changes can help reduce the intensity and frequency of UC flares. Currently, surgery to remove the colon is the only full cure for UC.
How long do flares last?
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment. Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
What is the procedure called when you still need to pass stool?
The procedure is called a proctocolectomy. Because you still need to pass stool, the surgeon will perform either an ileostomy or create an ileoanal reservoir. In an ileostomy, your surgeon attaches the end of your small intestine, called the ileum, to a hole in your abdomen to make an opening.
What is UC flare?
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity. Medication, your lifestyle, diet, and other factors may contribute to flare-ups.
How to manage UC flare ups?
Diet tips during a flare. A healthy diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, it’s important to identify and limit these foods.
Warning Signs of a Flare
Flares often are acute, meaning they come on suddenly. They can last from days to weeks. Between flare-ups, you may experience weeks, months, or years of remission. 1
What Triggers Flare-Ups
Many different factors can play a role in bringing on symptoms of a flare. Even if you have been avoiding potential triggers, you can still experience a flare.
How to Manage Ulcerative Colitis
Medications, diet, and other lifestyle changes can help decrease the severity and frequency of flare-ups. 4
Preventing Flare-Ups
Medications, diet, stress, and other lifestyle factors can contribute to worsening symptoms during a flare-up. 2
Summary
Ulcerative colitis can have periods of few to no symptoms and flare-ups with symptoms. What triggers a flare can vary for each person. During a flare, symptoms may include abdominal pain, diarrhea, fatigue, or bloody stool. You can use medication, diet, and lifestyle changes to help manage symptoms during a flare.
A Word From Verywell
While you can’t always prevent UC flare-ups, there is much you can do to decrease the chances of them occurring. Taking your medications as prescribed, maintaining a healthy lifestyle, and avoiding your triggers can help prevent or reduce symptoms during flare-ups.
How do biosimilars work?
Like biologics, these drugs target immune system proteins that contribute to inflammation. Biosimilars work in the same way as biologics, but they may cost much less. Four letters are added to the end of the name to help distinguish the biosimilar drug from the original biologic.
When was Infliximab approved?
infliximab-abda (Renflexis), FDA approved in May 2017. infliximab-axxq (Avsola), FDA approved in December 2019. infliximab-dyyb (Inflectra), FDA approved in April 2016. The Remicade biosimilars are the only ones currently available for purchase in the United States.
What is the best medicine for UC?
Aminosalicylates (5-ASA drugs) This group of drugs contains the ingredient 5-aminosalicylic acid (5-ASA). They include: When you take these drugs by mouth or as an enema, they help bring down inflammation in your intestine. Aminosalicylates work best for mild-to-moderate UC, and they can help prevent flare-ups.
What is TNF blocker?
Anti-TNF drugs block tumor necrosis factor (TNF), an immune system protein that triggers inflammation. TNF blockers can help people with moderate-to-severe UC whose symptoms haven’t improved while they were taking other medications.
What is stem cell therapy?
Stem cell therapy. Stem cells are the young cells that grow into all of the various cells and tissues in our bodies. They have the potential to heal all kinds of damage if we harness and use them correctly. In UC, stem cells may alter the immune system in a way that helps bring down inflammation and heal damage.
What is a fecal transplant?
A fecal transplant, or stool transplant, is an experimental technique that places healthy bacteria from a donor’s stool into the colon of someone with UC. The idea may sound unappealing, but the good bacteria help heal damage from UC and restore a healthy balance of germs in the gut.
What is the name of the drug that blocks the enzyme JAK?
Tofacitinib (Xeljanz) belongs to a class of medications known as Janus kinase (JAK) inhibitors. These drugs block the enzyme JAK, which activates cells of the immune system to produce inflammation.
What is flare up in GI tract?
A flare-up is the return or worsening of your symptoms. With inflammatory bowel diseases (IBD), like ulcerative colitis (UC) or Crohn’s disease, specific symptoms will depend on which condition you have and the part of your gastrointestinal (GI) tract that’s inflamed. This inflammation can lead to a symptom flare-up.
What causes flare ups in the body?
These are possible factors that could worsen symptoms and influence a flare: 1 Missing, skipping, or taking the wrong dose of medication —Flare-ups can result from not taking medications as prescribed. If you’re taking your medication as prescribed and still experience flares, talk to your doctor about possibly changing the dose, frequency, or medication. 2 Nonsteroidal anti-inflammatory drugs (NSAIDs) —Aspirin, naproxen, and ibuprofen are medications that could worsen returning symptoms and lead to inflammation. 3 Antibiotics —Used for treating bacterial infections, they also change the bacteria in the intestine. These changes to the bacteria may cause diarrhea or inflammation. Tell your doctor if you’re taking antibiotics and experience a UC flare-up. 4 Smoking —Cigarettes not only raise the risk of developing UC, but they can also trigger flares. 5 Stress —Whether it be emotional or physical, stress doesn’t cause UC, but it can affect symptoms. 6 Foods that irritate your GI tract —There’s no evidence that food can cause or cure UC, nor is there any evidence that it can cause a flare. But during a flare-up, food can affect your symptoms, and every person with UC is different when it comes to foods or drinks that may aggravate symptoms.
What to say when you have UC?
When you have UC, you may be thinking, “Will my condition flare up?” “What can I do when it does?” “How will I cope?” You’re not alone in those thoughts. Here, you’ll find helpful info that can help answer some of those questions you may be asking yourself.
Can colitis get worse over time?
Ulcerative colitis is chronic—over time, your symptoms can change, or get worse. When you’re experiencing a flare-up, it’s necessary to talk to your doctor; be precise about any differences in your symptoms or changes to your condition over time. How much of your time is your UC impacting?
Can food cause UC?
Foods that irritate your GI tract —There’s no evidence that food can cause or cure UC, nor is there any evidence that it can cause a flare. But during a flare-up, food can affect your symptoms, and every person with UC is different when it comes to foods or drinks that may aggravate symptoms.
Can antibiotics cause diarrhea?
Antibiotics —Used for treating bacterial infections, they also change the bacteria in the intestine. These changes to the bacteria may cause diarrhea or inflammation. Tell your doctor if you’re taking antibiotics and experience a UC flare-up.
How to heal ulcerative colitis?
In addition to this moderate exercise triggers the release of specific chemicals called myokines that promote healing from inflammatory-related damage. Yoga is a specific exercise that takes care of the digestive system and provides relief for many ulcerative colitis symptoms. Stress Reduction: Stress and anxiety are intricately linked ...
How to keep ulcerative colitis under control?
By relaxing, eating right, and exercising more , you can keep inflammation under control. The best defense against inflammation lies in the microbiome of your gut. By keeping gut flora numbers in balance, your gut stays healthy, you stay comfortable, and ulcerative colitis is no longer a worry.
How to maintain bacterial balance and a healthy gut?
The easiest way to maintain bacterial balance and a healthy gut is with daily supplements of probiotics or probiotic foods. Dietary Changes: A balanced diet is recommended for everyone.
Why does ulcerative colitis cause inflammation?
While genetics and diet contribute to the development of ulcerative colitis and exacerbate symptoms, the true cause is unknown. A faulty immune system response leads to widespread inflammation, which irritates and damages the gut lining. Over time, the damage caused can increase your risk of serious diseases and death.
What is the best supplement for ulcerative colitis?
Omega-3 fatty acids are powerful antioxidants and anti-inflammatory agents, making them an ideal weapon to have in your ulcerative colitis arsenal. Supplemental Support: Herbal supplements and remedies have been shown to relieve ulcerative colitis symptoms as well as promote healing of inflamed intestinal walls.
What happens if ulcerative colitis is left untreated?
If ulcerative colitis is left untreated, more serious diseases and complications can develop.
What foods can I eat to help with ulcerative colitis?
Green tea and several fresh fruits and vegetables like broccoli, blueberries, ginger, strawberries, and spinach are also good for controlling inflammation. Acidic fruits, like citrus fruits, increase inflammation and acid in the gut so should be avoided with ulcerative colitis, even if they are generally healthy otherwise.
Symptoms
Roughly half of people with ulcerative colitis report experiencing mild symptoms. 4 Possible symptoms include: 5
Natural Remedies for Ulcerative Colitis
There are some studies that suggest the use of natural remedies like dietary supplements, yoga, exercise, and dietary modifications may be beneficial for people with ulcerative colitis.
Summary
There is no cure for ulcerative colitis, but there are a number of treatment options available. Treatments include surgery, dietary modifications, and medications. There is some evidence to suggest natural remedies like yoga, omega-3 fatty acids, and some herbs may be beneficial for people with ulcerative colitis.
A Word From Verywell
When you're experiencing a UC flare-up, it's difficult to not search everywhere for answers. However, it is important to tread with caution when trying new home remedies. Always check with your doctor to make sure that changing your routine or consuming something new will not interfere with your current treatment regimen.
What to eat when you have ulcerative colitis?
Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help. 1. Applesauce: Since your gastrointestinal system is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, ...
What to eat during a colitis flare?
Avoiding certain foods is only half the battle. Here’s how to get the nutrients you need during an ulcerative colitis flare. Soft, canned fruit is a good food to eat during a flare-up. Jeff Wasserman/Stocksy. If you have ulcerative colitis, you may already know which foods worsen your flares.
What to eat if you don't like salmon?
If you don’t like salmon, you can eat tuna, shrimp, or other fish that are high in omega-3 fatty acids.
What foods are not irritating?
Also, soft fruits like canned pears or peaches may not be irritating, says Shannon Szeles, RDN, of York, Pennsylvania. 3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K.
Is curcumin good for colitis?
A meta-analysis published in November 2019 in the Annals of Gastroenterology found that taking curcumin along with an anti-inflammatory was better for treating ulcerative colitis than only taking an anti-inflammatory medication.
Is yogurt good for lactose intolerant people?
4. Probiotics: If you’re not lactose intolerant, yogurt can provide you with some protein and probiotics, which are live bacteria that may help the digestive system. Be sure to buy yogurt that says live and active cultures on the label, Szeles says. Avoid yogurt that contains large chunks of fruit, which could be hard to digest. “It’s fine if yogurt has fruit that’s soft, seedless, and blended in,” Szeles adds. Probiotic supplements are also an option if you are lactose intolerant.
Is turmeric good for ulcerative colitis?
8. Water, sports drinks, and fruit juice: The diarrhea that often occurs during an ulcerative colitis ...

Diagnosis
Treatment
- Ulcerative colitis treatment usually involves either drug therapy or surgery. Several categories of drugs may be effective in treating ulcerative colitis. The type you take will depend on the severity of your condition. The drugs that work well for some people may not work for others, so it may take time to find a medication that helps you. In addi...
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups. There's no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up. It can be helpfu…
Alternative Medicine
- Many people with digestive disorders have used some form of complementary and alternative medicine (CAM). However, there are few well-designed studies showing the safety and effectiveness of complementary and alternative medicine. Although research is limited, there is some evidence that adding probiotics along with other medications may be helpful, but this has …
Preparing For Your Appointment
- Symptoms of ulcerative colitis may first prompt you to visit your primary care doctor. Your doctor may recommend you see a specialist who treats digestive diseases (gastroenterologist). Because appointments can be brief, and there's often a lot of information to discuss, it's a good idea to be well prepared. Here's some information to help you get ready, and what to expect from your doct…