Medication
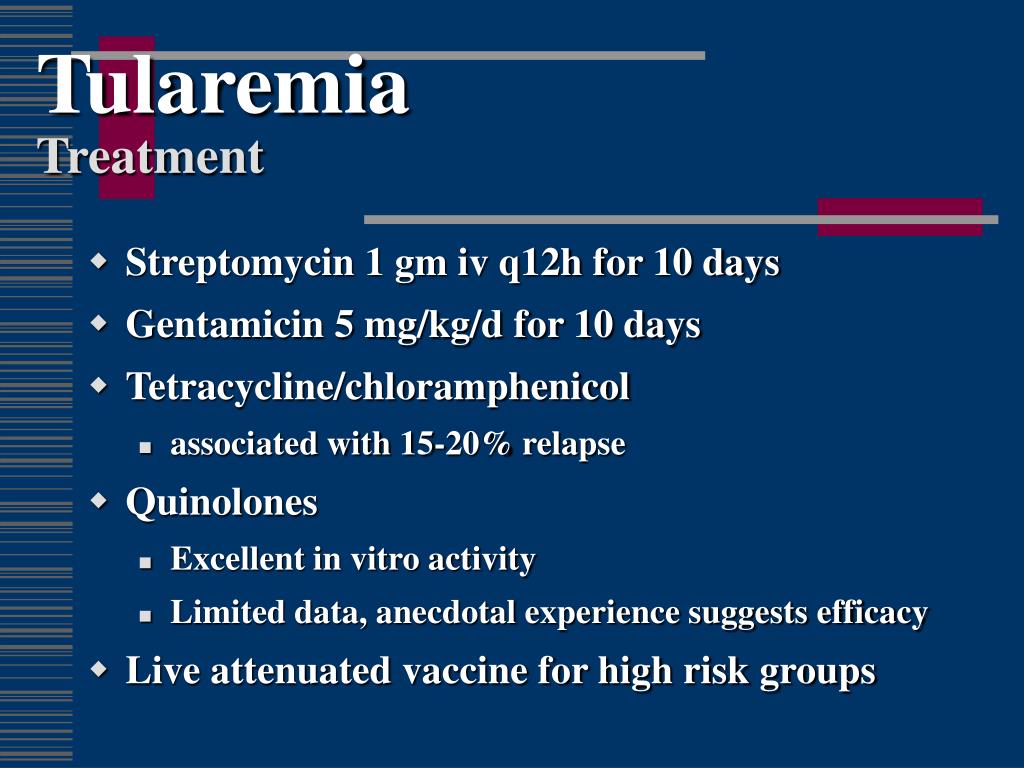
Dec 13, 2018 · Antibiotics used to treat tularemia include streptomycin, gentamicin, doxycycline, and ciprofloxacin. Treatment usually lasts 10 to 21 days depending on the stage of illness and the medication used. Although symptoms may last for several …
How can severe tularemia be treated?
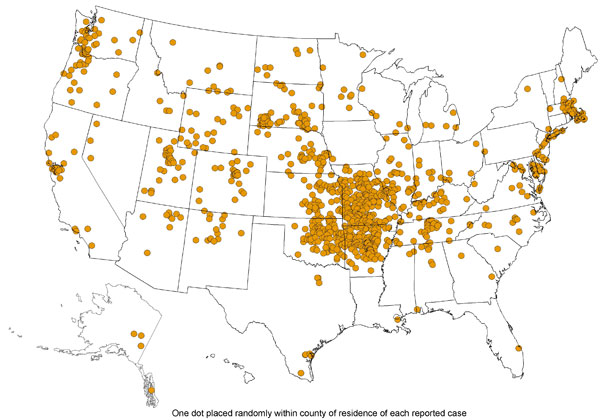
Dec 13, 2018 · Tularemia can be life-threatening, but most infections can be treated successfully with antibiotics. Steps to prevent tularemia include: Using insect repellent; Wearing gloves when handling sick or dead animals; Avoiding mowing over dead animals; In the United States, naturally occurring infections have been reported from all states except Hawaii.
Can tularemia be cured with antibiotics?
Apr 04, 2018 · TularemiaTreatment & Postexposure Prophylaxis. Treatment (from Abstract of “Consensus Statement: Tularemia as a Biological Weapon: Medical and Public Health Management”) Concise, bulleted summary of recommendations from the Working Group on Civilian Biodefense.
How to treat tularemia?
Limitations in both culture and serologic testing have led to substantial research into new diagnostic techniques and their clinical application, with PCR testing as the best example. This review focuses on the utility of culture, PCR and serologic testing for tularemia. In addition, we also review the evidence to support different therapeutic options for tularemia, highlighting …
How to avoid tularemia?
Sep 05, 2018 · Approach Considerations Inpatient care. Treatment for patients with tularemia includes supportive and general medical care for manifestations... Surgical care. Surgical care is not needed in tularemia management unless an ulcerative lesion develops a superinfection... Consultations. Consider ...
What is the best treatment for tularemia?
The antibiotic gentamicin is typically the treatment of choice for tularemia. Streptomycin is also effective, but can be hard to get and may have more side effects than other antibiotics.Nov 6, 2020
What antibiotics treat tularemia?
The tetracycline class (such as doxycycline) or fluoroquinolone class (such as ciprofloxacin) of antibiotics are taken orally. Streptomycin or gentamicin are also effective against tularemia, and are given by injection into a muscle or vein.
What are the signs and symptoms of tularemia?
The signs and symptoms in people can vary. Illness generally starts with symptoms such as a fever, chills, and swollen lymph nodes. Symptoms may also include skin or mouth ulcers, diarrhea, muscle aches, joint pain, cough, and weakness.
Can tularemia go away on its own?
Fever may be high, and may go away for a short time only to return. Untreated, the fever usually lasts about four weeks. Other symptoms depend on the type of tularemia.
How long does it take to recover from tularemia?
Treatment usually lasts 10 to 21 days depending on the stage of illness and the medication used. Although symptoms may last for several weeks, most patients completely recover.
How long can you have tularemia?
Most people exposed to tularemia who become sick generally do so within three to five days, although it can take as long as 21 days. There are several types of tularemia, and which type you get depends on how and where the bacteria enter the body. Each type of tularemia has its own set of symptoms.Nov 6, 2020
How contagious is tularemia?
Tularemia is not known to be spread from person to person. People who have tularemia do not need to be isolated. People who have been exposed to the tularemia bacteria should be treated as soon as possible. The disease can be fatal if it is not treated with the right antibiotics.
What tick causes tularemia?
Ticks that transmit tularemia to humans include the dog tick (Dermacentor variabilis), the wood tick (D. andersoni), and the lone star tick (Amblyomma americanum). Other transmission routes include deer fly bite, inhalation, ingestion, and through skin contact with infected animals.
Can you eat the meat of an animal with tularemia?
Can I Eat The Meat? Meat from animals that die of tularemia should not be consumed by humans. Normal cooking temperatures will kill bacteria in the meat. Management of tularemia is not practical or feasible in wild animals.
What is the most common clinical presentation of tularemia?
Ulceroglandular This is the most common form of tularemia and usually occurs following a tick or deer fly bite or after handing of an infected animal. A skin ulcer appears at the site where the bacteria entered the body. The ulcer is accompanied by swelling of regional lymph glands, usually in the armpit or groin.
Are there long term effects of tularemia?
Answer. When treated promptly, tularemia seldom has long-term effects. If it is untreated or if treatment is delayed, the infection may affect any part of the body, causing: Lung problems, such as pneumonia.
How do they test for tularemia?
A blood sample is needed . The sample is sent to a laboratory where it is examined for francisella antibodies using a method called serology. This method checks if your body has produced substances called antibodies to a specific foreign substance ( antigen ), in this case F tularensis.May 10, 2019
What is the best treatment for tularemia?
Tularemia can be effectively treated with antibiotics given by injection directly into a muscle or vein. The antibiotic gentamicin is typically the treatment of choice for tularemia. Streptomycin is also effective, but can be hard to get and may have more side effects than other antibiotics.
How to diagnose tularemia?
Tularemia can usually be diagnosed through blood tests. One test looks for antibodies to the bacteria, and that test won't show that you've had the infection until several weeks later. You may also have a chest X-ray to look for signs of pneumonia.
What antibiotics are used for tularemia?
Depending on the type of tularemia being treated, doctors may prescribe oral antibiotics such as doxycycline (Oracea, Vibramycin, others) or ciprofloxacin (Cipro) instead. You'll also receive therapy for any complications such as meningitis or pneumonia.
Is tularemia difficult to diagnose?
Because it's rare and because it shares symptoms with other diseases, tularemia may be difficult to diagnose. If you've participated in any activities that increase your risk, such as hunting rabbit, let your doctor know.
What is the best treatment for tularemia?
Streptomycin is considered the drug of choice (DOC) to treat tularemia. Less experience has been reported with other aminoglycosides; gentamicin and amikacin are effective, have been used successfully, and are more generally available.
How to prevent tick bites?
Tick bites can be prevented by avoiding tick-infested areas, wearing trousers and long-sleeved shirts, and using tick repellants and by frequent inspection of the body and clothing for evidence of ticks. Ticks should be promptly removed by grasping the tick near the mouthparts and pulling upward. Care should be taken to not squeeze ...
Is ceftriaxone a third generation?
Ceftriaxone, a third-generation cephalosporin, has been examined in the treatment of tularemia and, although it was found to have good in vitro MICs (minimal inhibitory concentrations), a number of therapeutic failures occurred. [ 62, 63] Prophylaxis.
Is tularemia a reportable disease?
Tularemia is currently a reportable disease in the United States. Contact your local public health department if you suspect a case of tularemia. Contact local or federal law enforcement agencies and the Centers for Disease Control and Prevention if multiple cases occur, which would suggest biologic or terrorist attack.
What are the risks of tularemia?
Inhaling a fine mist or spray (aerosol) or dust particles containing the bacteria. People who work outdoors or pursue outdoor activities such as hunting, trapping, hiking, or camping are at greater risk of contracting tularemia.
Why is it so hard to diagnose tularemia?
It may be difficult to diagnose tularemia because its symptoms may look like those of other infections. Your doctor will conduct a physical exam and ask questions about your medical history. You should tell your doctor about any possible exposure to infected animals or insect bites.
Why do rabbits have red eyes?
Hunters who skin and dress meat from rabbits or other animals may be prone to eye infections. Inflammation of the membrane of the eye ( conjunctivitis) may cause eye pain, redness, and itching. Swollen lymph glands also may occur. Pneumonic: This is a very serious form of tularemia and may be life-threatening.
What is tularemia in animals?
Tularemia is an infection caused by Francisella tularensis bacteria. While wild animals often die after being infected, people who are treated quickly can recover. Symptoms include fever, rash, and a feeling of being unwell. Appointments 216.444.6503. Appointments & Locations. Contact Us. Overview.
How can tularemia be transmitted to humans?
The main ways that tularemia can be transmitted to humans include: Being bitten by ticks, horse flies, deerflies, or mosquitoes. Handling live or dead animals infected with tularemia or their fluids or tissues. Eating food or drinking water that is contaminated.
What is the disease of a rabbit called?
Tularemia is a rare and highly infectious disease caused by Francisella tularensis bacteria. It is also called rabbit fever or deer fly fever. The bacteria can infect a wide range of animals, including rabbits and hares, beavers, muskrats, squirrels, and mice, and transmit the disease to people. Cases of tularemia have occurred in household pets, ...
How long does it take for tularemia to show?
Usually, it takes from three to five days after infection before symptoms appear, but it might take up to two to three weeks. Symptoms of tularemia may include: Skin ulcer or rash.
What is tularemia?
Tularemia is an illness caused by the bacteria Francisella tularensis. It is also called deer-fly fever or rabbit fever. The bacteria that cause tularemia are often found in animals, such as rodents, birds, reptiles, and fish. The bacteria can survive for weeks at low temperatures in water, moist soil, hay, and straw.
How is tularemia spread?
Tularemia is not spread from person to person. You may become infected through any of the following:
What are the risks of tularemia?
Tularemia can cause damage to your eyes and skin. You may have inflammation in your lungs and around your heart. You may get a lung or bone infection. You are also at risk for meningitis, and the infection may spread to your brain. Tularemia may become life-threatening.
How can I prevent tularemia?
Cook meat thoroughly before you eat it. This is especially important when you eat meat from hunting.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.