Medication
The U.K. National Institute of Health and Care Excellence has endorsed the use of stereotactic radiosurgery as a treatment of trigeminal neuralgia (TN) after hearing from a patient group, promising more clinical bandwidth for these systems.
Procedures
The short answer to this question is not likely. Trigeminal neuralgia may continue to worsen, rather than improve, over time. This means that you may start out with a milder case but it can continue to progress and the pain may intensify over time. The frequency of the spells may also increase and become closer together.
What is trigeminal neuralgia, and how is it treated?
ViewMedica Error
- Clinical Trials. Patients who have tried medications and surgical options and keep experiencing debilitating pain may qualify for clinical trials to help manage trigeminal neuralgia.
- Acupuncture and Other Integrative Medicine Treatments. ...
- Caring for a Loved One with Trigeminal Neuralgia. ...
Does trigeminal neuralgia go away or get better?
Is trigeminal neuralgia serious? The condition itself is not life-threatening, but it can affect a person’s quality of life. The pain of trigeminal neuralgia can limit your ability to eat, drink, bathe, brush teeth, or be with family and friends.
What is the best painkiller for trigeminal neuralgia?
How serious is trigeminal neuralgia?

What is the most common cause of trigeminal neuralgia?
Causes of Trigeminal Neuralgia Trigeminal neuralgia usually occurs spontaneously, but is sometimes associated with facial trauma or dental procedures. The condition may be caused by a blood vessel pressing against the trigeminal nerve, also known as vascular compression.
What is the latest treatment for trigeminal neuralgia?
Currently, MVD is the closest possible cure for trigeminal neuralgia. However, it's an invasive procedure and carries a risk of potentially serious complications, such as facial numbness, hearing loss, stroke and even death in around 1 in every 200 cases.
Can trigeminal neuralgia be cured?
Although trigeminal neuralgia cannot always be cured, there are treatments available to alleviate the debilitating pain. Normally, anticonvulsive medications are the first treatment choice.
Can trigeminal neuralgia go away by itself?
The short answer to this question is not likely. Trigeminal neuralgia may continue to worsen, rather than improve, over time. This means that you may start out with a milder case but it can continue to progress and the pain may intensify over time.
What foods should you avoid if you have trigeminal neuralgia?
Very hot and very cold temperatures can irritate the nerve, causing it to misfire. In addition, the trigeminal neuralgia alcohol trigger should also be avoided....Other foods and drinks to avoid include the following:spicy foods;high-sugar foods;caffeinated drinks;junk foods and highly processed foods.
What is the best painkiller for neuralgia?
The anti-convulsant drug most commonly prescribed for trigeminal neuralgia is carbamazepine (Tegretol), which can provide at least partial pain relief for up to 80 to 90 percent of patients. Other anti-convulsants prescribed frequently for trigeminal neuralgia include: Phenytoin (Dilantin) Gabapentin (Neurontin)
What triggers neuralgia?
The pain can be caused by a blood vessel pressing down on the nerve where it meets with the brainstem. It can also be caused by multiple sclerosis, injury to the nerve, or other causes. Trigeminal neuralgia causes severe, recurrent pain in the face, usually on one side.
Does trigeminal neuralgia show on MRI?
Imaging tests such as a magnetic resonance imaging (MRI) scan can be very helpful in diagnosing trigeminal neuralgia. An MRI can help your doctor see if there is pressure on the trigeminal nerve.
Can you live a normal life with trigeminal neuralgia?
In the vast majority of those cases, they're able to help people diagnosed with the condition go on to live normal, mostly pain-free lives.
What can trigger trigeminal neuralgia?
A variety of triggers may set off the pain of trigeminal neuralgia, including:Shaving.Touching your face.Eating.Drinking.Brushing your teeth.Talking.Putting on makeup.Breeze lightly blowing over your face.More items...•
Can trigeminal neuralgia lead to stroke?
Background: There are no reports on the risk of stroke after trigeminal neuralgia (TN).
Can trigeminal neuralgia be caused by anxiety?
While stress alone doesn't cause trigeminal neuralgia, stress can aggravate the condition. There isn't a lot of understanding about how or why, but one possibility is the relationship between stress and pain. Studies have shown that chronic pain can lead to stress-induced heightened pain sensitivity.
How to treat trigeminal neuralgia?
Microvascular decompression (MVD), also known as the Jannetta procedure, is the most common surgical procedure for treating trigeminal neuralgia. In the procedure, the surgeon makes a small incision behind the ear and drills a small hole in the skull. Using microscopic visualization, the trigeminal nerve is exposed. In most cases, there is a blood vessel — typically an artery, but sometimes a vein — compressing the trigeminal nerve. By moving this blood vessel away from the nerve and interposing a padding made of Teflon felt, the pain is nearly always relieved.
What is the best anti-convulsant for trigeminal neuralgia?
The anti-convulsant drug most commonly prescribed for trigeminal neuralgia is carbamazepine (Tegretol), which can provide at least partial pain relief for up to 80 to 90 percent of patients. Other anti-convulsants prescribed frequently for trigeminal neuralgia include: 1 Phenytoin (Dilantin) 2 Gabapentin (Neurontin) 3 Lamotrigine (Lamictal) 4 Oxcarbazepine (Trileptal) 5 Topiramate (Topamax)
How long does it take for trigeminal neuralgia to respond to treatment?
Patients usually begin to respond to the treatment within four to 12 weeks post-treatment, but some patients require as much as six to 12 months for the full response. Most patients remain on full doses of their trigeminal neuralgia medication for at least three to six months after treatment.
What is the trigeminal nerve exposed to?
Using microscopic visualization, the trigeminal nerve is exposed. In most cases, there is a blood vessel — typically an artery, but sometimes a vein — compressing the trigeminal nerve. By moving this blood vessel away from the nerve and interposing a padding made of Teflon felt, the pain is nearly always relieved.
Is radiofrequency lesioning a good option for MS patients?
It is also a good option for patients with multiple sclerosis (MS), whose trigeminal neuralgia often is not caused by vascular compression .
Can you have trigeminal neuralgia surgery?
Surgery for trigeminal neuralgia is rarely attempted on patients with non-trigeminal neural gia face pain or on atypical trigeminal neuralgia, since operations for these conditions have much lower success rates and, in many cases, can make the pain worse and/or cause additional medical problems.
Is gamma knife surgery?
Gamma Knife is the least invasive surgical option for trigeminal neuralgia. In fact, it is technically not surgery at all. The Gamma Knife is a device that delivers precise, controlled beams of radiation to targets inside the skull, including the brain and associated nerves. For trigeminal neuralgia treatment, the radiation beams are aimed at the trigeminal nerve where it enters the brainstem.
Microvascular Decompression (MVD)
The most effective of all the surgical treatments for trigeminal neuralgia, microvascular decompression (MVD) is performed in a hospital, under general anesthesia, by a sub-specialized neurosurgical team. As such, MVD requires a hospital stay of anywhere between 1-3 days.
Gamma Knife Radiosurgery (GKRS)
Also called stereotactic radiosurgery, Gamma Knife radiosurgery (GKRS) is an intervention that delivers multiple radiation beams to the root of the trigeminal nerve. This approach will result in the slow formation of a lesion on your nerve that should stop the transmission of pain signals to your brain.
Percutaneous Rhizotomy
In a percutaneous rhizotomy, the medical team will use different agents to damage part of your trigeminal nerve, which should block pain signals to your brain. The intervention consists of passing a hollow needle through your cheek and guiding it to your trigeminal nerve.
Pain Stimulator Placement
The deliverance of tiny electrical impulses to the nerve is the means by which stimulator placement is used to ease pain. When you undergo this procedure, you’ll receive a shot of a local anesthetic to numb your face. Your surgeon will then insert a small electrode under your skin and connect it to an external stimulator.
Choosing the Best Treatment for Trigeminal Neuralgia
If you have facial pain, make an appointment with an expert neurosurgeon to get a correct diagnosis. Your doctor will most likely try to manage your condition with the first-line medications including Tegretol and/or Trileptal.
Conclusion
The answer to the question, “ What is the best treatment for trigeminal neuralgia ?” depends on many variables. Your doctor can evaluate you and advise the treatment that would most optimally suit your needs.
What causes trigeminal neuralgia?
The condition may be caused by a blood vessel pressing against the trigeminal nerve , also known as vascular compression.
How does a rhizotomy for trigeminal neuralgia work?
The surgeon inserts a long needle through the cheek on the affected side of the face and uses an electrical current (heat) or a chemical (glycerin or glycerol) to deaden the pain fibers of the trigeminal nerve. For those undergoing trigeminal neuralgia rhizotomy for the first time, the chemical approach is typically recommended. Those who have the procedure repeated often benefit from both the chemical and the heat treatment delivered in the same session.
What nerve is irritated in the face?
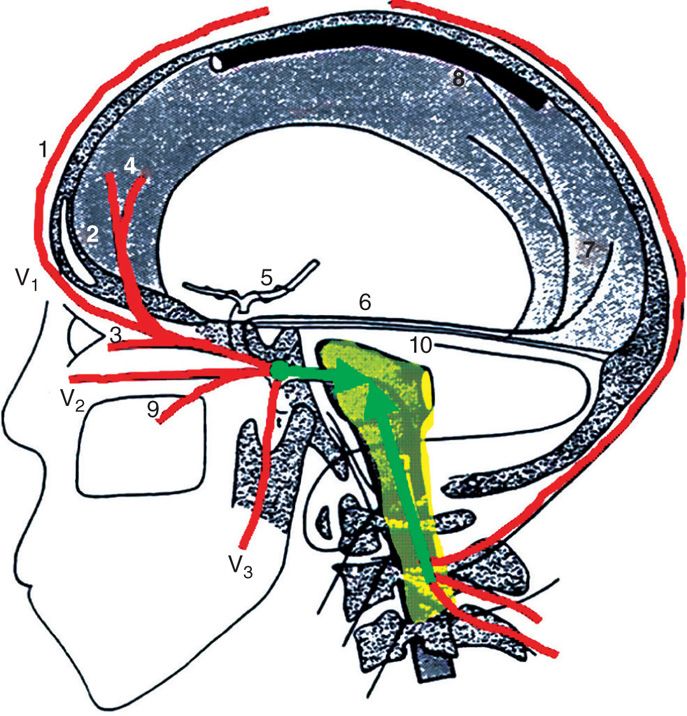
Trigeminal Neuralgia Pain. The trigeminal nerve splits off into three branches: ophthalmic, maxillary and mandibular. Each branch provides sensation to different areas of the face. Depending on which branch and which part of the nerve is irritated, trigeminal neuralgia pain can be felt anywhere in the face.
How long does a trig neuralgia pain last?
The pain travels through the face in a matter of seconds, but as the condition progresses, the pain can last minutes and even longer. Trigeminal neuralgia is sometimes known as tic douloureux, ...
Where is the pain of trigeminal neuralgia felt?
Depending on which branch and which part of the nerve is irritated, trigeminal neuralgia pain can be felt anywhere in the face. Most commonly, it is felt in the lower part of the face. The intensity of the pain is exceptional: Some people report it to be more severe than experiencing a heart attack, passing a kidney stone or even giving birth.
Is trigeminal neuralgia more common in older people?
Trigeminal neuralgia occurs more often in women than men, is more common in older people (usually 50 and older), and occurs more on the right than the left. It doesn’t usually run in families.
Can triceminal neuralgia be treated?
Trigeminal neuralgia relief is possible: Medical and surgical treatments can bring the pain under control, especially when managed by an expert physician and surgeon.
What is trigeminal neuralgia?
Trigeminal neuralgia (TN) is defined by the International Headache Society (IHS) as “unilateral disorder characterized by brief electric shock-like pains, abrupt in onset and termination, and limited to the distribution of one or more divisions of the trigeminal nerve” [International Headache Society, 2004]. The IHS suggests a classification of TN as either classic (essential or idiopathic) TN (CTN) or symptomatic TN (STN; pain indistinguishable from that of CTN, but caused by a demonstrable structural lesion other than vascular compression). The diagnosis of CTN requires the absence of a clinically evident neurological deficit. CTN starts in the second or third divisions, affecting the cheek or the chin [International Headache Society, 2004]. The ophthalmic division alone is involved in less than 5% of cases [De Simone et al.2005]. The single attack generally lasts from less than a second to a few seconds, but it may present in clusters of variable intensity with up to 2 minutes duration. In many cases it is followed by a brief refractory period during which a new stimulation is not able to evoke another attack. Between paroxysms the patient is usually pain free, but a dull background pain may persist in some cases [International Headache Society, 2004]. Growing neurosurgical data advocate the distinction of these two subtypes of TN into type 1 as defined as >50% episodic onset of TN pain and type 2 defined by >50% constant pain [Tatli et al.2008; Limonadi et al.2006]. The mechanisms associated with the development of this persistent pain are not well understood but concomitant background pain is associated with poor medical and surgical outcome [Obermann et al.2008; Sandell and Eide, 2008; Szapiro et al.1985]. Recent investigations focused on the suspected central component in the pathophysiology of TN, which could involve central allodynic mechanisms that may also engage the nociceptive neurons at thalamic and cortical level [Obermann et al.2007].
What is the name of the drug that is used for neuralgia?
Killian J.M., Fromm G.H. (1968) Carbamazepine in the treatment of neuralgia. Use of side effects. Arch Neurol19: 129–136 [PubMed] [Google Scholar]
What is repetitive transcranial magnetic stimulation?
Repetitive transcranial magnetic stimulation (rTMS) is an emerging technology that introduces the possibility of assessing whether patients with trigeminal neuropathic pain will respond to direct epidural cortical stimulation by first measuring their response to a trial of non-invasive cortical stimulation. In a study of 24 TN patients given rTMS to the motor cortex at 20 Hz daily for 5 days, pain ratings decreased by approximately 45% for 2 weeks [Khedr et al.2005]. In a different study of 12 patients with chronic intractable TN who had failed surgical treatment, 58% experienced a greater than 30% reduction in pain after receiving repetitive TMS [Lefaucheur et al.2004].
How effective is phenytoin for neuralgia?
Phenytoin has proven effective in managing neuralgia crisis in a small case series. A loading dose of 14 mg/kg applied intravenously was required to relieve the pain for 1–2 days, which is long enough for alternative oral drug therapy to kick in when initiated simultaneously [Cheshire, 2001]. Intranasal administered lidocaine 8% was effective in temporarily relieving second-division neuralgic pain [Kanai et al.2006b]. Subcutaneous sumatriptan 3 mg was shown to be superior to placebo in providing prompt and marked analgesia in 80% of patients in a double-blind, placebo-controlled study of 24 patients with refractory TN. The median duration of pain relief was 8 h [Kanai et al.2006a]. A different approach could be ganglionic local opioid analgesia (GLOA) at the superior cervical ganglion, which was evaluated retrospectively in 74 patients with neuropathic facial pain. A clinically relevant pain reduction was observed in 73% of the patients. The proportion of responders (pain reduction ≥50%) was 59% after the first blockade [Elsner et al.2006].
What are the other antiepileptic drugs?
Benefit was suggested for phenytoin, clonazepam, gabapentin, pregabalin, topiramate, levetiracetam and valproate as well as tocainide (12 mg/day) [Lindstrom and Lindblom, 1987]. In particular, the newer AEDs with less interaction with other medications and fewer side effects will be worth further investigation. As the incidence of TN increases with age [Khan, 1998], age-related physiologic changes that alter pharmacokinetics, such as reduced hepatic and renal function, blood flow decline, less predictable drug protein binding and interactions with multiple other medications required due to concomitant illness, will come increasingly into focus. Approximately 6–10% of patients cannot tolerate CBZ [Taylor et al.1981]. Multiple pharmacologic interactions and a narrow therapeutic window of tolerability further limit the use of CBZ. Promising in this regard are lamotrigine, pregabalin, gabapentin, topiramate and leve tiracetam. The newer AEDs tested within the past 2 years are topiramate, levetiracetam, gabapentin and pregabalin. Gabapentin showed adequate efficacy alone and in combination with local injections of ropivacaine used to block trigger points in TN patients. Even though only 36 patients were investigated, this combination seems safe and effective in the treatment of TN [Lemos et al.2008]. Gabapentin is initiated at 300 mg daily and may be gradually increased by 300 mg each 2–3 days as tolerated. Gabapentin has no interaction with other drugs and relatively minor side effects that may include dizziness, somnolence, headache, diarrhoea, confusion, nausea and ankle swelling. Pregabalin was tested in an open-label study including 53 patients (14 with concomitant constant facial pain) with 1-year follow-up. Pregabalin (150–600 mg/day) proved to be effective in reducing TN pain by over 50% in 74% of patients with minor efficacy reduction over the 1-year observational period. Patients without concomitant facial pain showed better response rates (32 out of 39, 82%) compared with patients with concomitant chronic facial pain (7 out of 14, 50%, p = 0.020) [Obermann et al.2008]. Topiramate (100–400 mg/day) was effective in 75% of patients in a very small sample of only eight patients [Domingues et al.2007]. A very recent pilot study investigated the efficacy and tolerability of levetiracetam in 10 patients with TN over a period of 10 weeks in an open-label prospective design. Patients were treated with up to 4000 mg daily and 40% (n = 4) reported an improvement of 50–90% [Jorns et al.2009]. Further randomized, controlled trials will have to follow to confirm these preliminary findings.
How to treat TN?
The general recommendation is to start with medical therapy and consider surgical procedures in patients who are refractory to medical treatment (Figure 1). Studies that compare medical and surgical treatment directly are still missing. Active participation in support groups may help many patients in dealing better with their disease and with suggested therapy [Zakrzewska et al.2009].
What is the effect of botulinum neurotoxin type A?
Several descriptions postulated an analgesic effect of botulinum neurotoxin type A (BoNT- A) through local release of anti-nociceptive neuropeptides such as substance P, glutamate and calcitonin-gene related peptide (CGRP) inhibiting central and possibly peripheral sensitization [Aoki, 2005]. Reports of isolated TN patients treated with BoNT-A and a small, uncontrolled clinical trial (n = 13) showed significant relief from symptoms after treatment with BoNT-A. Mean BoNT-A dose was 3.22 units/cm2administered directly into the affected facial regions subcutaneously. At 60 days follow-up the pain began to slowly return in most patients [Piovesan et al.2005].
Where is trigeminal neuralgia located?
Primary trigeminal neuralgia has been linked to the compression of the nerve, typically in the base of the head where the brain meets the spinal cord . This is usually due to contact between a healthy artery or vein and the trigeminal nerve at the base of the brain. This places pressure on the nerve as it enters the brain and causes ...
How many people are diagnosed with trigeminal neuralgia every year?
Prevalence and Incidence. It is reported that 150,000 people are diagnosed with trigeminal neuralgia (TN) every year. While the disorder can occur at any age, it is most common in people over the age of 50.
What is the pain in the lower jaw called?
Trigeminal neuralgia (TN), also known as tic douloureux, is sometimes described as the most excruciating pain known to humanity. The pain typically involves the lower face and jaw, although sometimes it affects the area around the nose and above the eye.
How many branches does the trigeminal nerve have?
Each of these nerves has three distinct branches. "Trigeminal" derives from the Latin word "tria," which means three, and "geminus," which means twin. After the trigeminal nerve leaves the brain and travels inside the skull, it divides into three smaller branches, controlling sensations throughout the face:
How to diagnose TN?
Newer scanning techniques can show if a vessel is pressing on the nerve and may even show the degree of compression. Compression due to veins is not as easily identified on these scans. Tests can help rule out other causes of facial disorders. TN usually is diagnosed based on the description of the symptoms provided by the patient, detailed patient history and clinical evaluation. There are no specific diagnostic tests for TN, so physicians must rely heavily on symptoms and history. Physicians base their diagnosis on the type pain (sudden, quick and shock-like), the location of the pain and things that trigger the pain. Physical and neurological examinations may also be done in which the doctor will touch and examine parts of your face to better understand where the pain is located.
What is the pain of TN1?
TN1 is characterized by intensely sharp, throbbing, sporadic, burning or shock-like pain around the eyes, lips, nose, jaw, forehead and scalp. TN1 can get worse resulting in more pain spells that last longer.
Can accupuncture help with trigeminal neuralgia?
The study concluded that accupuncture can be used as an alterantive treatment for trigeminal neuralgia to improve patient’s quality of life.
What causes trigeminal neuralgia?
Trigeminal neuralgia can also be caused by a tumor compressing the trigeminal nerve. Some people may experience trigeminal neuralgia due to a brain lesion or other abnormalities. In other cases, surgical injuries, stroke or facial trauma may be responsible for trigeminal neuralgia.
How does trigeminal neuralgia feel?
Trigeminal neuralgia symptoms may include one or more of these patterns: Episodes of severe, shooting or jabbing pain that may feel like an electric shock. Spontaneous attacks of pain or attacks triggered by things such as touching the face, chewing, speaking or brushing teeth. Bouts of pain lasting from a few seconds to several minutes.
What nerve causes pain in the cheek and jaw?
Constant aching, burning feeling that may occur before it evolves into the spasm-like pain of trigeminal neuralgia. Pain in areas supplied by the trigeminal nerve, including the cheek, jaw, teeth, gums, lips, or less often the eye and forehead.
What is the name of the nerve that is disrupted by blood pressure?
In trigeminal neuralgia, also called tic douloureux, the trigeminal nerve's function is disrupted. Usually, the problem is contact between a normal blood vessel — in this case, an artery or a vein — and the trigeminal nerve at the base of your brain. This contact puts pressure on the nerve and causes it to malfunction.
Can trigeminal neuralgia cause pain?
You may initially experience short, mild attacks. But trigeminal neuralgia can progress and cause longer, more-frequent bouts of searing pain. Trigeminal neuralgia affects women more often than men, and it's more likely to occur in people who are older than 50.
What is the name of the TN pain?
Medications for Trigeminal Neuralgia. Other names: Tic Doloureux; TN Pain. Trigeminal neuralgia is an extremely painful inflammation of the trigeminal nerve which causes severe lightening-like facial pain and spasm of the facial muscles on the involved side. These painful attacks may occur after lightly touching different skin areas of the face, ...
Can you have a cranial nerve attack after touching your face?
These painful attacks may occur after lightly touching different skin areas of the face, along the course of this cranial nerve. Specific medications can be very effective in reducing the rate of attacks, but surgical intervention may be necessary.