Explore
tinea cruris is best treated by homeopathic medicines like sulphur 30, rhustox 30, dulcamara 30 depending on the symptoms pertaining to the disease as per the modalities and areas of involvement.
What is the best medicine for tinea?
- Griseofulvin (Grifulvin V, Gris-PEG)
- Terbinafine
- Itraconazole (Onmel, Sporanox)
- Fluconazole (Diflucan)
What is the best oral antifungal medication for tinea capitis?
Tinea Pedis Treatment Guidelines
- Treat the fungus The most effective topical medicine we have to treat tinea pedis is known as terbinafine. ...
- Improve your natural tinea defence Tinea thrives in the extremes. In moist or dry skin as well as warm, dark, enclosed places. ...
- Disinfect other tinea reservoirs
Is there a natural treatment for tinea pedis?
Yes, Naturasil for Tinea Versicolor really Works!
- Made with High-Quality Botanicals, Essential Oils & Premium Volcanic Sulfur
- Removes Discoloration & Heals Your Skin Quickly!
- NO SLS, EDTA, TEA, DEA, or MEA
- Safe for Sensitive Skin!
- Made in the USA in a registered FDA Facility
- Remember to get in the sun afterward to bring the coloration back to your skin!
What soap is good for tinea versicolor?

What's the best treatment for tinea cruris?
Abstract. After clinical diagnosis and microscopic confirmation, tinea cruris is best treated with a topical allylamine or an azole antifungal (strength of recommendation: A, based on multiple randomized controlled trials [RCTs]).
How can I permanently cure tinea cruris at home?
Apple cider vinegar has strong antifungal properties, so it may help treat ringworm when applied topically to the affected area. To use it, soak a cotton ball in undiluted apple cider vinegar and brush the cotton ball over your skin. Do this three times per day.
What is tinea cruris caused by?
Tinea cruris, also known as jock itch, is an infection involving the genital, pubic, perineal, and perianal skin caused by pathogenic fungi known as dermatophytes.
Is tinea cruris serious?
Although often uncomfortable and bothersome, jock itch usually isn't serious. Treatment may involve keeping the groin area clean and dry and applying topical antifungal medications to the affected skin.
Which soap is best for fungal infection?
Soaps play an important role in the treatment of skin infections. Aactaril is a medicated soap, designed for the effective management of common, superficial bacterial and fungal infections of the skin.
What is the strongest medicine for jock itch?
Medicated shampoos that contain ketoconazole or selenium sulfide are a good, strong treatment for jock itch symptoms. They're available by prescription from your doctor or over the counter.
Is tinea cruris permanent?
Prognosis of Jock Itch Jock itch usually doesn't go away on its own, but it can be easily treated and cured. Jock itch usually responds promptly to treatment. It is often less severe than other tinea infections, such as athlete's foot, but may last a long time.
What is the strongest antifungal medication?
1. Among the six systemic antifungals tested, fluconazole, griseofulvine, itraconazole, ketoconazole, terbinafine, and voriconazole, the allylamine terbinafine was the most potent agent.
Which cream is best for fungal infection?
Antifungal creams, liquids or sprays (also called topical antifungals) These are used to treat fungal infections of the skin, scalp and nails. They include clotrimazole, econazole, ketoconazole, miconazole, tioconazole, terbinafine, and amorolfine. They come in various different brand names.
Is tinea cruris curable?
Clinical cure of an uncomplicated tinea cruris infection usually can be achieved using topical antifungal agents of the imidazole or allylamine family.
How do you test for tinea cruris?
Microscopic examination of a potassium hydroxide (KOH) wet mount of scales is diagnostic in tinea cruris. The procedure for KOH wet mount is as follows: Clean the area with 70% alcohol. Collect scales from the margin of the lesion; use a scalpel or the edge of a glass slide for this purpose.
What cream is best for groin rash?
Most cases of jock itch can be treated with over-the-counter medicines. “You can use a topical antifungal cream, like Gold Bond medicated powder, Tinactin or Lamisil ointment,” says Dr. Modi. “If those don't work, you can go to your doctor and get prescription-strength lotion of a similar anti-fungal powder or cream.”
How to avoid tinea cruris?
Tinea cruris can be avoided by practicing good skincare hygiene by keeping the groin clean and dry. The general and preventive measures below will assist in averting the itching condition:
How often does Tinea cruris clear up?
Tinea cruris clears up in 80–90 percent of instances with proper treatment. Recurrence, on the other hand, is common, particularly if predisposing factors are not addressed or antifungal treatment is discontinued before mycological cure. If you spot a case of Tinea cruris or observe any change on your skin, consult a dermatologist immediately. SkyMD has the best team of dermatologists. Ask our dermatologists any questions you have regarding skin infections or conditions and get immediate answers from our experts. You do not need to book a prior appointment. Simply visit our app, fill in the necessary details and consult with a qualified dermatologist through video call or chat, whatever suits you.
What are the risk factors for Tinea cruris?
Male genitalia, heat, dampness, humidity, obesity, excessive sweating, exercise, a weaker immune system, tight clothing and underwear, and athlete's foot infection or other fungal infections on the body are also risk factors. Tinea cruris can lead to the following complications:
Where does Tinea cruris start?
Tinea cruris is a rash that usually starts in the inguinal (groin) skin fold on one side and can progress to involve both sides forming a symmetrical rash.
What is the best antifungal cream for tinea?
Antifungal creams can be purchased in pharmacies or obtained through a prescription. Terbinafine, clotrimazole, econazole, ketoconazole, and miconazole are examples of different drugs that can be used for tinea. These lotions are effective at removing fungus from the skin.
What is the red streak on the groin called?
Catch sight of a red streak (called lymphangitis) that extends from the groin.
Can Tinea cruris be contagious?
Although the majority of cases of Tinea cruris are not contagious, infection s can spread by physical or sexual contact, sharing swimsuits, or sharing towels. Through close skin contact, it is possible to spread fungal jock itch to others. Because of their overall health, activities, possible compromised immune state, exposure history, and other predisposing skin diseases like eczema, some people are simply more prone to acquiring jock itch. Tinea cruris may also be seen in people who have coexisting athlete's foot (tinea pedis).
What is the best isolation media for dermatophytosis?
Culture and antifungal sensitivity:[22] Sabouraud dextrose agar (SDA, 4% peptone, 1% glucose, agar, water) is the most commonly used isolation media for dermatophytosis and serves as the medium on which most morphologic descriptions are based. Development of colony takes 7–14 days. Modified SDA, with addition of gentamicin, chloramphenicol and cycloheximide is more selective for dermatophytes as chroramphenicol inhibits the growth of saprophytic fungus. Dermatophyte test medium is an alternative to isolation media that contain pH indicator phenol red. It is incubated at room temperature for 5–14 days. Dermatophytes utilize the protein resulting in excess ammonium ion and alkaline environment which turn the medium from yellow to bright red.
Can hyphae be detected over an annular patch?
It provides in vivoimaging of the epidermis and superficial dermis at cellular level resolution and can be used to detect cutaneous fungi and parasitic infestations.[27] Branching fungal hyphae can be detected over an erythematous annular scaly patch. Advantage of the test being noninvasive and in a retrospective analysis of the test by Friedman et al. sensitivity was found to be 100%.
How to treat tinea cruris?
Patient education should focus on non-pharmacologic measures to treat and prevent recurrences of tinea cruris. Loose-fitting, non-restrictive garments should be encouraged, and clothing should not be donned until the underlying skin is completely dried.[3] Because autoinfection originating from tinea pedis may occur, patients should avoid walking barefoot, and protective footwear should be used in public facilities. [3][13] Identification and treatment of potentially infected contacts, whether human or animal, should be undertaken.[13] Self-treatment with over-the-counter antifungals and steroids should be discouraged as this may result in resistant or chronic infections and can hinder a clinician's ability to make an accurate and timely diagnosis. [4]
What causes tinea cruris?
Tinea cruris is caused by dermatophytes belonging to three genera, Trichophyton, Epidermophyton, and Microsporum. [5] Trichophyton rubrumhas been isolated most commonly and remains the most frequent cause of tinea cruris worldwide; however, most studies do recognize the increasing prevalence of Trichophyton mentagrophytes and other organisms in certain regions. [1][2][3][4][7] Several risk factors have been identified that predispose an individual to tinea cruris, including excessive perspiration, occlusive clothing, improper hygiene, diabetes mellitus, immunocompromise, and lower socioeconomic status. [1][2][3][6]
What percentage of people have tinea cruris?
Cutaneous mycoses, including tinea cruris, affect 20 to 25 percent of the world's population. [3][10]Developing and tropical countries have an increased prevalence of dermatophyte infections secondary to high temperatures and increased humidity. [1][11]In the United States, there have been an estimated 29.4 million cases of superficial fungal infections and over 51 million reported physician visits.[6] Adolescent and adult males comprise the majority of patients seen for tinea cruris and are affected by the disorder with increased frequency. [1][2][11]Worldwide increases in the occurrence of dermatophytoses and the discovery of recalcitrant infections have caused global concern. [3][4][5][9]
What are the complications of tinea cruris?
Failure of therapy and recurrence are the most likely complications of tinea cruris. They have been attributed to reinfection from close contacts, autoinfection from separate body locations, infection by uncommon species such as zoonoses, misdiagnosis, drug resistance, and non-adherence to the management plan.[3] Steroid use may suppress the physical signs of tinea cruris, making the diagnosis more difficult. Also, chronic application can result in skin atrophy and telangiectasias.[4] Secondary bacterial infection is another potential complication of tinea cruris.[3] Majocchi’s granuloma is an uncommon complication of cutaneous fungal infections in which dermatophytes disseminate into the subcutaneous tissue secondary to skin breakdown, immunosuppression, or topical steroid use resulting in a deep, inflammatory disease. [3][20] A dermatophytid reaction may result in an allergic response at a separate location from the original tinea site. [21]
What antifungal is used for dermatophytoses?
Antifungals utilized in treating dermatophytoses, including tinea cruris, target the synthesis of ergosterol, a vital component of fungal plasma membranes.[4] Management strategies are similar worldwide; however, some countries have specific guidelines based on their region's fungal profile.[6] Topical therapies are effective and usually preferred. [2][4][6] Allylamines (terbinafine, butenafine, naftifine) and azoles (clotrimazole, miconazole, sulconazole, oxiconazole, econazole, ketoconazole) are the mainstays of topical treatment regimens. They are generally prescribed once or twice daily for two to four weeks. [1][3][6]
Can tinea cruris be diagnosed?
In most cases, tinea cruris can be diagnosed clinically; however, several tests exist to investigate a rash of the groin with unknown etiology. [1][2][3]Potassium hydroxide (KOH) preparations, skin biopsy with periodic acid-Schiff (PAS) stain, and fungal cultures on Sabouraud’s agar media can be utilized when the diagnosis is in question or the case of recurrent or recalcitrant episodes. [1][2][3]
Can topical steroids be used for tinea cruris?
Current management principles and guidelines label them as mistreatment; however, continued investigations of their utility are underway. If a practitioner believes topical steroids may benefit a patient, close supervision should be maintained throughout the treatment course with continued consideration of known adverse event potential for the individual and public health outcomes.
How to prevent tinea cruris?
To prevent recurrences of tinea cruris, concurrent fungal infections such as athlete's foot need to be treated. Also advised are measures to avoid moisture build-up including keeping the groin region dry, avoiding tight clothing and losing weight if obese. People with athletes foot or tinea cruris can prevent spread by not lending their towels to others.
How to treat a groin infection?
Treatment is with topical antifungal medications and is particularly effective if symptoms have recent onset. Prevention of recurrences include treating concurrent fungal infections and taking measures to avoid moisture build-up including keeping the groin region dry, avoiding tight clothing and losing weight if obese.
What is the name of the fungal infection in the groin?
Treat any fungal infections of feet or nails. Tinea cruris , also known as jock itch, is a common type of contagious, superficial fungal infection of the groin region, which occurs predominantly but not exclusively in men and in hot-humid climates.
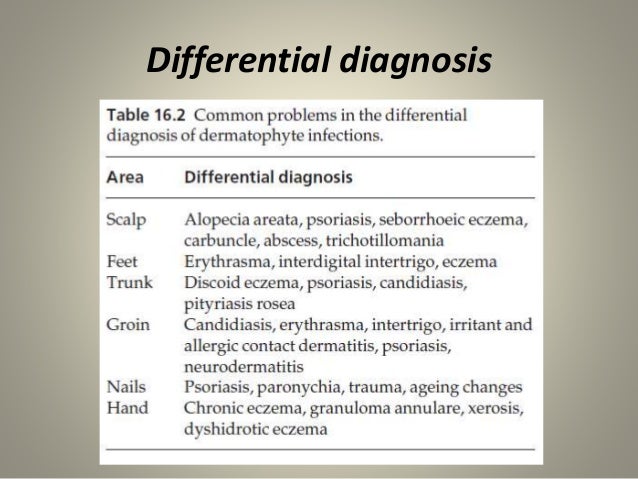
What tests can be done for seborrhoeic dermatitis?
Tests may include microscopy and culture of skin scrapings.
Is Tinea cruris common in children?
Tinea cruris is common in hot-humid climates and is the second most common clinical presentation for dermatophytosis. It is uncommon in children.
Can you use topical steroids in addition to antifungal?
The benefits of the use of topical steroids in addition to an antifung al is unclear. There might be a greater cure rate but no guidelines currently recommend its addition. The effect of Whitfield's ointment is also unclear, but when given, it is prescribed at half strength.
Is Tinea cruris life threatening?
Tinea cruris is not life threatening and treatment is effective, particularly if the symptoms have not been present for long. However, recurrence may occur. The intense itch may lead to lichenification and secondary bacterial infection. Irritant and allergic contact dermatitis may be caused by applied medications.