
Treatment of superficial vein thrombosis There is a range of treatments for superficial vein thrombosis. Options include warm compresses and NSAID Nonsteroidal anti-inflammatory drugs are a drug class that reduce pain, decrease fever, prevent blood clots and, in higher doses, decrease inflammation. Side effects depend on the specific drug, but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack a…Nonsteroidal anti-inflammatory drug
How do I treat superficial vein thrombosis?
How I treat isolated distal deep vein thrombosis (IDDVT)
- Case 1: M.P.B.
- Case 2: R.P.
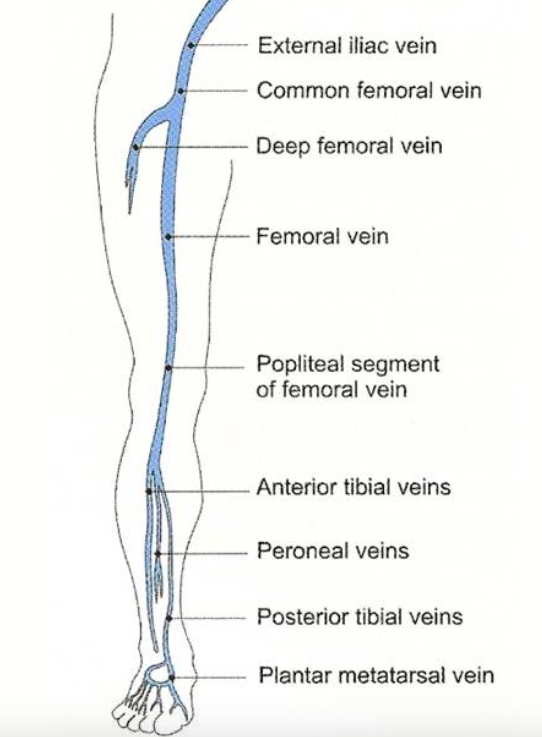
- The “distal” or “calf” deep veins
- Diagnosis of proximal and distal DVT
- Epidemiology
- Natural history and clinical relevance of IDDVT
- Personal views
Can deep vein thrombosis be cured?
To help prevent swelling associated with deep vein thrombosis, wear them on your legs from your feet to about the level of your knees. You should wear these stockings during the day for at least two years, if possible.
Is there a cure for deep vein thrombosis (DVT)?
While DVT may be a serious health condition, it can be treated. 1. Ginger Apart from being an excellent healing spice, ginger plays an important role in treating deep vein thrombosis. It is an effective medicine to break down the fibrins that cause DVT and further helps in smooth movement of blood.
What is the best treatment for phlebitis?
- Use a warm washcloth to apply heat to the involved area several times daily.
- Elevate your leg.
- Use a nonsteroidal anti-inflammatory drug, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others), if recommended by your doctor.
How do you treat superficial venous thrombosis?
For superficial thrombophlebitis, your doctor might recommend applying heat to the painful area, elevating the affected leg, using an over-the-counter nonsteroidal anti-inflammatory drug (NSAID) and possibly wearing compression stockings. The condition usually improves on its own.
Do superficial blood clots need to be treated?
Most bouts of superficial thrombophlebitis last for 3-4 weeks. If they are associated with varicose veins, they are likely to return (recur). No treatment may be needed if the symptoms are mild.
How long treat for superficial vein thrombosis?
There are multiple reasons for considering anticoagulants as a treatment option in patients with acute SVT. The most common indication is the presence of or increased risk of associated acute DVT/pulmonary embolism due to the location of SVT. In such cases, prophylaxis for about four weeks is often recommended.
How do you treat upper limb DVT?
DVT-UE is treated by anticoagulation, with heparin at first and then with oral anticoagulants. Direct oral anticoagulants are now being increasingly used. The thrombus is often not totally eradicated. Anticoagulation is generally continued as maintenance treatment for 3–6 months.
Should I worry about a superficial blood clot?
Blood clots in veins close to the skin's surface usually are not serious and often can be treated at home. Sometimes superficial thrombophlebitis spreads to a deeper vein (deep vein thrombosis, or DVT). These deeper clots can be serious, even life-threatening.
Is superficial vein thrombosis serious?
Unlike deep vein thrombosis, or DVT, a superficial venous thrombosis is less likely to cause serious complications but it can still cause pain and discomfort. Blood clots and VTE are common, with millions of hospital patients experiencing this complication following procedures.
Does superficial thrombophlebitis require anticoagulation?
Anticoagulants are usually not indicated in superficial thrombophlebitis unless the process extends into the deep venous system or persistent inflammation is present in an affected area.
Can a superficial blood clot be surgically removed?
Surgical removal of the varicosities with excision of the thrombosed veins is currently our preferred treatment for superficial thrombophlebitis in otherwise healthy patients.
Can I exercise with superficial thrombophlebitis?
Treatments generally include analgesics, elastic compression, anti-inflammatory agents, exercise and ambulation, and, in some cases, local or systemic anticoagulants. It is better to avoid bed rest and reduced mobility.
How is upper extremity DVT diagnosed?
Duplex ultrasonography is the best initial evaluation because it is noninvasive and has a high sensitivity and specificity. Other imaging options for confirming the diagnosis include venous angiography and magnetic resonance angiography.
What causes upper extremity DVT?
Compression is caused by repetitive motion of the upper extremity which, in the setting of anatomic abnormalities, such as hypertrophied scalene muscles, congenital presence of cervical ribs, and subclavius ligaments, place these individuals at a higher risk of UEDVT.
How common are upper extremity blood clots?
Upper extremity DVT (UEDVT) can appear in your neck or arms and travel to your lungs. This type of DVT can also lead to a PE. About 10 percent of all DVTs occur in the upper extremity. UEDVTs affect about 3 out of every 100,000 people.
How to treat superficial vein thrombosis?
There is a range of treatments for superficial vein thrombosis. Options include warm compresses and NSAID medications or anticoagulation. There is no one rule to help decide which treatment will suite a particular patient. The factors that dictate which treatment to use for any particular patient are the extent of the clot, assessment of recurrence rates with and without treatment, patient preference, the risk of progression to deep vein thrombosis and the amount of inflammation. It is not completely clear whether superficial vein thrombosis progresses to deep vein thrombosis. It is not even clear which untreated superficial clot will result in poor long-term outcomes. But in some patients that can happen. There are data, for example, that superficial vein thrombosis may sometimes progress to deep vein thrombosis or to pulmonary embolism. Therefore, there is still more to learn about when to treat.
What is the treatment for deep vein thrombosis?
Symptoms include pain and redness over the effected area. Treatment options include warm compresses and NSAID medications or anticoagulation. Read on to learn about diagnosis and management.
What is the difference between superficial veins and deep veins?
The deep veins of the legs (or arms) are large veins that form from the conjunction of superficial veins that drain into them. As an analogy, one might look at a deep vein thrombosis as a traffic jam in a main road, while a superficial vein thrombosis is just traffic on a side street. Thus, superficial veins are usually smaller, ...
What is the medical term for a clot in the superficial veins of the legs?
He also holds a specialty in Medicine from the Hadassah Hebrew University Medical School. Superficial vein thrombosis involves clots forming in superficial veins in the legs. This is different than deep vein thrombosis. If inflammation is also present, it is called thrombo-phlebitis.
Why are veins a risk factor?
Varicose veins are also a risk factor because of pooling of blood in the varicosities. A very important risk factor for superficial vein thrombosis is a previous clot. Essentially this means that any previous venous thrombotic event may predispose to another clot.
How to tell if a vein is superficial?
Symptoms and imaging studies guide the diagnosis of superficial vein thrombosis. Typical symptoms include redness, pain and swelling of the involved vein, most commonly in the leg. The involved vein can be in the lower leg, bellow the knee or it can extend all the way up to the thigh. Sometimes the vein can actually be palpated ...
Why do blood clots occur?
e. pregnancy, prolonged flight, post surgical state, varicose veins) are risks for superficial vein thrombosis. Cancer is a specific cause for blood clots.
What is superficial venous thrombosis?
Superficial venous thrombosis (SVT) or superficial thrombophlebitis is characterized by thrombi within superficial veins, with partial involvement or occlusion of the lumen and inflammatory reaction along the course of the vein. Clinical diagnosis tends to be straightforward, but supplementary tests and examinations are needed to confirm thrombosis extension and possible thromboembolic complications. SVT can be associated with deep venous thrombosis in 6 to 40% of cases, with asymptomatic pulmonary embolism (PE) in 20 to 33%, and with symptomatic PE in 2 to 13%. Despite the morbidity and complications, there are currently no Brazilian guidelines for SVT. These guidelines cover the most important issues related to SVT definition, terminology, and etiology, and set out recommendations for diagnosis and treatment.
What is superficial thrombophlebitis?
Superficial thrombophlebitis, or superficial venous thrombosis (SVT), is characterized by formation of thrombi inside superficial veins, with involvement or occlusion of the lumen and inflammatory reaction along the venous path. It is more common in the lower limbs and affects from 3 to 11% of the general population.1Conn et al.2reported prevalence of 123,000 cases/year in the United States. Clinically, SVT presents as a palpable cord and a firm area that is hot and inflamed and follows the path of a superficial vein.3It can be associated with immunological syndromes (Trousseau, Lemièrre, or Mondor syndromes) or with inflammatory diseases such as thromboangiitis obliterans or thrombophilia, it can be caused by traumas or by injection of irritants, or it may be a complication of lower limb varicose veins.3
What causes SVT in the saphenous vein?
It is also common for SVT to occur after damage to the intima caused by intravenous injection or infusion of solutions for therapeutic or diagnostic purposes, or even after mechanical injuries such as those that can occur during catheterization and hemodynamic procedures. Nowadays, many endovascular procedures are used for therapeutic purposes, primarily in the saphenous veins, to treat varicose veins, and SVT is one of the possible complications of laser, radio frequency, and even some sclerosants. Drugs, such as certain chemotherapy agents or hypertonic glucose, can often cause SVT.24
What causes SVT?
Etiopathogenesis of SVT is related to Virchow’s triad. The most common cause is varicose veins, because of their dilatation and tortuosity, which predisposes to stasis, inflammation, and thrombosis. Superficial venous thrombosis can also occur in patients who do not have varicosities, but have malignant diseases or diseases associated with thrombophilia, or in people who take estrogens, although the evidence for the last of these is not very well defined.20Some authors classify SVT into two subclasses: related or unrelated to varicose veins.4In approximately 60 to 70% of cases, SVT involves the great saphenous vein and when this is not varicose, involvement may be associated with cancer, in 5 to 13% of cases, or thrombophilia, in more than 50% of cases.7,21-23
What is needed to confirm thromboembolic extension?
Clinical diagnosis tends to be straightforward, but supplementary tests and examinations are needed to confirm thrombosis extension and possible thromboembolic complications. Several types of treatments are currently available, but in general they are supported by scant scientific evidence. Existing guidelines identify options with a greater degree of consensus, some clinical and some surgical.4-7
Should thrombophilia be tested for SVT?
Consensus statements suggest that tests for thrombophilias should not be ordered for all patients with SVT,5,22even though genetic thrombophilias are an important element in predisposition for SVT, in extension of the process from the superficial system to the deep system, and also in recurrence.28,33,34Thrombophilias should only be investigated in patients with unexplained SVT in non-varicose veins (after ruling out occult tumors) and/or those in whom thrombosis continues to progress despite the appropriate anticoagulation.22Many authors consider that testing for thrombophilia in non-selected patients with DVT has no clinical value. In the 2010 British Society for Haematology consensus,35recommendations were summarized as: a) who should be tested; b) who should not be tested; and c) people for whom no valid recommendation can be made with regard to the benefits of thrombophilia testing, because of a lack of evidence.
Is superficial venous thrombosis a benign disease?
Traditionally, the disease has been called phlebitis or superficial thrombophlebitis. However, some authors consider that superficial venous thrombosis is a more appropriate term, because inflammation and infection are not part of the primary disease. This term is also more likely to avoid incorrect administration of antibiotics and the misconception that this is a benign disease.4,19We therefore recommend using the term “superficial venous thrombosis” for this disease (Evidence level 5).
What is the diagnosis of SVT?
Diagnosis. Diagnosis of SVT is usually clinical, especially when tender and inflamed veins can be identified. 2, 8 Vascular ultrasound is often performed to confirm the diagnosis and to rule out coexisting DVT or other pathologies—eg, arterial thrombosis, pseudoaneurysm, and venous incompetence, among others.
What are the risk factors for SVT?
7 The patient had several risk factors, including intravenous line, age over 60 years, prior history of SVT, and duration of the procedure over 45 minutes. In addition, the lateral decubitus position with an axillary roll likely caused external pressure on the proximal arm that impaired venous outflow, established intravascular stasis, and ultimately predisposed her to thrombosis. Avoiding intravenous lines and pressure cuffs in the extremity in downward position, alternative choice of positioning, use of compression devices or garments, or prophylactic pre- and postoperative anticoagulation in high-risk patients may minimize the risk for both DVT and SVT. Finally, recurrent episodes of SVT, often termed migratory thrombophlebitis, should be investigated for possible underlying malignancy—eg, Trousseau’s syndrome.
Is SVT a self-limiting condition?
SVT of the upper extremity is usually a self-limiting condition. 7 Herein, we present a patient with extensive thrombosis of cephalic and basilic veins, resulting in acute venous congestion mimicking DVT and acute carpal tunnel syndrome.
Is superficial vein thrombosis a disease?
Superficial vein thrombosis has traditionally been considered a disease of the lower extremity. Less frequently it can affect the breast, chest wall, penis, or upper extremity. Cases involving upper extremities are usually associated with intravascular access, and the vast majority remain self-limiting.
Is a syphilis a disease of the lower extremity?
Traditionally, it has been considered a disease of the lower extremity. 1 Less frequently, it can affect the breast, chest wall, penis, or upper extremity. 2–6 Cases involving upper extremities are primarily associated with intravascular access and usually remain self-limiting.
Can a SVT be severe?
Upper extremity SVT can present with severe symptoms when cephalic and basilic veins are involved. Bedside ultrasound performed by a surgeon is an excellent tool that can provide immediate answers and prevent unnecessary delays in treatment. Despite immediate treatment, symptoms of SVT can persist for months, substantially affecting patients’ recovery and satisfaction.
Is ultrasonography accurate for SVT?
Clinical diagnosis may not be accurate, and ultrasonography is currently indicated for both confirmation and evaluation of SVT extension. Treatment aims are symptom relief and prevention of venous thromboembolism (VTE) in relation to the thrombotic burden.
Is superficial vein thrombosis a self-limiting disease?
Superficial vein thrombosis (SVT) is less well studied than deep vein thrombosis (DVT), because it has been considered to be a minor, self-limiting disease that is easily diagnosed on clinical grounds and that requires only symptomatic relief.
Is superficial vein thrombosis the same as deep vein thrombosis?
Superficial vein thrombosis (SVT) is less well studied than deep vein thrombosis (DVT), because it has been considered to be a minor, self-limiting disease that is easily diagnosed on clinical grounds and that requires only symptomatic relief. The most frequently involved sites of the superficial vein system are the lower limbs, especially the saphenous veins, mostly in relation to varicosities. Lower-limb SVT shares the same risk factors as DVT; it can propagate into the deep veins, and have a complicated course with pulmonary embolism. Clinical diagnosis may not be accurate, and ultrasonography is currently indicated for both confirmation and evaluation of SVT extension. Treatment aims are symptom relief and prevention of venous thromboembolism (VTE) in relation to the thrombotic burden. SVT of the long saphenous vein within 3 cm of the saphenofemoral junction (SFJ) is considered to be equivalent to a DVT, and thus deserving of therapeutic anticoagulation. Less severe forms of lower-limb SVT not involving the SFJ have been included in randomized clinical trials of surgery, compression hosiery, non-steroidal anti-inflammatory drugs, unfractionated heparin, and low molecular weight heparins, with inconclusive results. The largest randomized clinical trial available, on 3004 patients with lower-limb SVT not involving the SFJ, showed that fondaparinux 2.5 mg once daily for 6 weeks is more effective than placebo in reducing the risk of the composite of death from any cause and symptomatic VTE (0.9% versus 5.9%). Further studies are needed to define the optimal management strategies for SVT of the lower limbs and other sites, such as the upper limbs.
Where is a superficial venous thrombosis?
Superficial venous thrombosis is a blood clot in a superficial vein of the upper or lower extremities or, less commonly, in one or more veins of the chest or breast (Mondor disease).
What is the diagnosis of deep venous thrombosis above the knee?
Patients with superficial venous thrombosis above the knee have an increased risk of deep venous thrombosis (DVT) and should probably have ultrasonography.
What is the name of the venous thrombosis that causes chest pain?
Superficial Venous Thrombosis. Varicose Veins. Test your knowledge. Angina Pectoris. Angina pectoris is usually described as chest discomfort rather than as chest “pain.”. The symptoms of angina pectoris may be a vague, barely troublesome ache or may rapidly become a severe, intense precordial crushing sensation.
Is superficial venous thrombosis a harbinger of pancreatic cancer?
Migratory superficial venous thrombosis, which develops, resolves, and recurs in normal veins of the arms, legs, and torso at various times, is a possible harbinger of pancreatic cancer and other adenocarcinomas (Trousseau syndrome). Diagnosis is based on history and physical examination.
Is fondaparinux good for superficial venous thrombosis?
In patients with extensive superficial venous thrombosis, anticoagulation (eg, with low molecular weight heparin, fondaparinux ) is often beneficial. The optimal regimen and duration are unknown, but most experts recommend using either low molecular weight heparin (eg, enoxaparin 40 mg subcutaneously once a day or fonda parinux 2.5 mg subcutaneously once a day) and treating for about 1 month.
How to diagnose DVT in the upper extremity?
The best way to confirm a diagnosis is with compression duplex ultrasonography. This test has a sensitivity of 97% and specificity of 96% for the determination of DVT in the upper extremity and is often the test of choice. However, several other imaging modalities including magnetic resonance and computed tomographic venography are superior to ultrasonography, but their clinical use may be limited by high costs, radiation exposure, and/or availability. The sensitivity of compression duplex ultrasonography is 97%, which is lower than magnetic resonance venography (100%). However, it is non-invasive, less expensive and widely available, thus remains the test of choice to diagnose upper extremity DVT. Laboratory studies are not required for diagnosis, but a coagulation assay can be ordered in patients suspected of having a hypercoagulable condition. In patients with a low suspicion of upper extremity DVT, a d-dimer test can help rule it out. A patient with upper extremity DVT complicated by PE may present with chest pain and shortness of breath. ECG should be performed because it will most commonly demonstrate sinus tachycardia. [9][10][11]
What is the primary form of DVT?
There are 2 forms of upper extremity DVT: primary and secondary. The primary form is known as Paget-Schroetter syndrome (PSS) and typically occurs in the dominant arm of younger athletic patients involved in activities requiring excessive and repeated motion of the upper extremities such as wrestling, swimming, gymnastics, and sports involving repetitive ball throwing (i.e., football, baseball, and basketball). The secondary form occurs most commonly in patients with central venous catheterization or patients with malignancy. [5][6][7][8]
What percentage of DVTs are Pss?
The majority of patients have a central line, while PSS accounts for only 10% to 20% of cases. The rate of upper extremity DVT in all patients with central catheterization is between 14% to 23%. PE occurs in up to 6% of DVTs affecting the upper extremities compared to 15% to 30% in the lower extremities. Post-thrombotic syndrome occurs in less than 5% of DVTs in the upper extremities compared to greater than 50% in the lower extremities.
What is the prognosis of DVT?
The prognosis differs between primary and secondary forms. Patients with the primary form (PSS) of upper extremity DVT are typically young and healthy , while those with secondary forms are often previously hospitalized and may have significant co-morbidities such as cancer. In a large database study, overall 3-month mortality in patients with DVT in the upper extremity was 11%. In a sub-group analysis of patients with cancer, the mortality rate was as high as 28%. Complications such as PE and post-thrombotic syndrome can also occur. PE occurs in up to 6% of cases and occurs most often in secondary forms of upper extremity DVT. Post-thrombotic syndrome occurs in less than 5% of upper extremity DVT and can result in persistent limb swelling, pain, and heaviness. However, in patients with PSS, the post-thrombotic syndrome can occur in as high as 45% of cases. If this continues untreated, it can result in skin discoloration and collateralization. Investigations are underway to determine if compression therapy may help prevent and/or treat the post-thrombotic syndrome.
What are the symptoms of DVT?
The majority of patients present only with limb swelling and arm discomfort. The onset and duration of limb swelling along with any previous history of DVT should be obtained. Patients may also complain of arm heaviness. The physical exam may also reveal limb erythema with visible veins across the chest and upper extremity (Urschel’s sign). Personal and family history of hypercoagulable disorders are relevant as well as if any prior central venous catheterization has been attempted. In the primary form (PSS), patients will present with a sudden onset of severe limb pain and swelling often in the dominant arm. These patients are younger and often participate in activities requiring excessive and repeated motions of the upper extremity (e.g., baseball pitcher). In all patients, distal pulses should be assessed. Limbs appearing pale, cool and mottled are at risk of ischemia. Any motor or sensory deficit should be noted, as these require emergency intervention.
How many DVTs are associated with PE?
PE occurs in up to 6% of DVTs affecting the upper extremities compared to 15% to 30% in the lower extremities. Post-thrombotic syndrome occurs in less than 5% of DVTs in the upper extremities compared to greater than 50% in the lower extremities. Pathophysiology.
How long does it take for a heparin line to be removed?
If the line is not needed, it should be removed but only after completion of 3 to 5 days of anticoagulation therapy. In the hospital, patients can be bridged to warfarin with unfractionated heparin. Patients should continue on warfarin for 3 to 6 months after diagnosis.
What is the best treatment for thrombophlebitis?
For the superficial, localized, mildly tender area of thrombophlebitis that occurs in a varicose vein, treatment with mild analgesics, such as aspirin, and the use of some type of elastic support usually are sufficient. Patients are encouraged to continue their usual daily activities.
What is the prevalence of DVT and PE?
A meta-analysis of the prevalence of DVT and PE in patients with superficial vein thrombosis found a weighted mean prevalence of 18.1% for DVT and 6.9% for PE in patient with superficial thrombophlebitis. The authors concluded that in selected patients with superficial thrombophlebitis, screening for DVT or PE may be warranted. [ 30]
What happens if you dangle your leg without bandages?
In the early phases of superficial thrombophlebitis in the leg, dangling the extremity without external support from stockings or elastic bandages leads to leg swelling and increased pain.
What is gradient compression?
Gradient compression stockings are an often-overlooked adjunctive therapy that is both benign and effective. These highly elastic stockings provide a gradient of compression that is highest at the toes (at least 30-40 mm Hg) and gradually decreases to the level of the thigh. This amount of compression reduces capacitive venous volume by approximately 70% and increases the measured velocity of blood flow in the deep veins by a factor of 5 or more. Gradient compression hose also have been shown to increase local and regional intrinsic fibrinolytic activity.
Why is puncture less effective in the first week after onset of symptoms?
Puncture and evacuation is less effective in the first week after the onset of symptoms, because the vessel wall is thickened and the coagulum itself is more cohesive during the early phase of phlebitis.
Is Fondaparinux good for superficial thrombophlebitis?
The investigators found fondaparinux to be a good option for treatment of superficial thrombophlebitis and prevention of some of its associated complications. [ 26]
Can saphenous thrombophlebitis be treated?
Surgical treatment may also be considered for patients with saphenous thrombophlebitis. This is most often considered if the process extends upward toward the femoral or popliteal vein despite anticoagulation or in a patient with a contraindication to systemic anticoagulation.
What causes superficial thrombophlebitis?
Superficial thrombophlebitis can be caused by an injury to the arm or leg; having an intravenous (IV) line; or the cause may not be known.Potential risk factors are the same as for those who have deep vein thrombosis (DVT), and include: An inherited (family) condition that increases your risk of blood clots.
What is a thromboembolic clot?
What is thrombophlebitis? Thrombophlebitis means there is a blood clot in the vein (thrombosis or thromboembolism) that causes swelling and pain. Superficial thrombophlebitis: If the vein that has the clot is just under the skin, it is called a superficial venous thrombosis or superficial thrombophlebitis. This type of clot does not usually travel ...
Why is a vascular ultrasound important?
An ultrasound is also important because about 20% of people with superficial thrombophlebitis also have a DVT. Many times, patients who have superficial thrombophlebitis wait to see a doctor, thinking they have a muscle strain or sprain.
How long does it take for thrombophlebitis to clear up?
In most cases, superficial thrombophlebitis clears up within a few weeks.
What does it feel like to have a blood clot on your leg?
Swelling of the leg or arm (sometimes this happens suddenly) Pain or tenderness in the area of the clot. Feeling of increased warmth in the area of the clot. Red or discolored skin in the area of the clot. If thrombophlebitis causes pain or interferes with your daily activities, talk to your doctor about treatment options.
Where is the catheter placed for endovenous ablation?
Types of surgery include: Endovenous ablation. A special catheter (long, thin tube) is placed in the saphenous vein (the longest vein in your body; it runs along the inside of your leg).
How old do you have to be to get a clot?
Pregnancy and the first 6 weeks after giving birth. Being over age 40 (although clots can form at any age) Being overweight. Taking birth control pills or hormone therapy, including for treatment for postmenopausal symptoms. Placement of a central venous catheter or pacemaker.
