Is thickening of the uterine lining always cancer?
This is thickening of the uterine lining and it is not always a sign of cancer, even though, as Dr. Schink points out, it can eventually lead to malignancy.
What does without atypia mean?
Another name for endometrial hyperplasia without atypia is benign endometrial hyperplasia. The uterus is a pear-shaped hollow organ found in the female pelvis between the rectum (last part of the large bowel) and the urinary bladder.
What causes endometrial hyperplasia?
You cannot prevent endometrial hyperplasia, but you can help lower your risk by:
- Losing weight, if you are obese.
- Taking a medicine with progestin (synthetic progesterone), if you already are taking estrogen, due to menopause or another condition.
- Taking birth control or another medicine to regulate your hormones and menstrual cycle.
How do you treat endometrial hyperplasia?
Your healthcare provider may recommend a hysterectomy if: 5
- During follow-up, you develop atypical hyperplasia
- The hyperplasia does not improve after 12 months of progesterone treatment
- You are having significant abnormal bleeding
- You develop endometrial hyperplasia again after it was successfully treated
- You do not want to undergo the repeat endometrial biopsies required with progesterone treatment.
Can simple hyperplasia turn into cancer?
Mild or simple hyperplasia, the most common type, has a very small risk of becoming cancer. It may go away on its own or after treatment with hormone therapy. If the hyperplasia is called “atypical,” it has a higher chance of becoming a cancer.
Does simple endometrial hyperplasia without atypia?
Types of endometrial hyperplasia include: Simple endometrial hyperplasia (without atypia): This type of endometrial hyperplasia has normal-looking cells that aren't likely to become cancerous. This condition may improve without treatment. Hormone therapy helps in some cases.
What is the treatment for simple hyperplasia?
The most common treatment is progestin. This can be taken in several forms, including pill, shot, vaginal cream, or intrauterine device.
Can simple endometrial hyperplasia go away on its own?
Endometrial hyperplasia is an increased growth of the endometrium. Unlike a cancer, mild or simple hyperplasia can go away on its own or with hormonal treatment. The most common type of hyperplasia, simple hyperplasia, has a very small risk of becoming cancerous.
What is the best treatment for endometrial hyperplasia?
In many cases, endometrial hyperplasia can be treated with progestin. Progestin is given orally, in a shot, in an intrauterine device (IUD), or as a vaginal cream. How much and how long you take it depends on your age and the type of hyperplasia. Treatment with progestin may cause vaginal bleeding like a period.
What type of hysterectomy is best for endometrial hyperplasia?
Partial hysterectomy (removal of the uterus and cervix) is the treatment of choice for hyperplasia with atypia in patients who have completed childbearing. Supracervical hysterectomy should not be performed because the abnormal uterine cells can be present in the cervix.
How long do you take progesterone for endometrial hyperplasia?
Approximately 1% of patients who are on combined HRT develop benign EH. In such cases, the dose should be increased or they should be switched to 3 months of progestin-only therapy to encourage the regression of the hyperplastic endometrium.
What is the most common age to get endometrial hyperplasia?
In our study, among women 18–90 years the overall incidence of endometrial hyperplasia was 133 per 100,000 woman-years, was most common in women ages 50–54, and was rarely observed in women under 30. Simple and complex hyperplasia incidences peaked in women ages 50–54.
How can I improve my uterine lining?
Take some helpful supplements Getting an estrogen boost may help improve the uterine lining over time. Furthermore, supplements such as iron, digestive enzymes, fish oils, and vitamin E can help. Some studies show L-Arginine, turmeric, and even low-dose aspirin can also help.
How do you get rid of endometrial hyperplasia naturally?
Natural Hyperplasia TreatmentsBalance Hormones. Your diet and lifestyle play a big part in regulating hormone levels, including estrogen and testosterone. ... Eat an Anti-Inflammatory Diet. ... Supplements. ... Exercise. ... Reduce Stress.
How long does it take to treat endometrial hyperplasia?
The best treatment for this type of endometrial hyperplasia is to have the intrauterine system (IUS) put in. This is better known as a contraceptive device (a type of coil). It releases a progestogen hormone which thins the lining of the uterus (womb). This stays in for at least six months, but for up to five years.
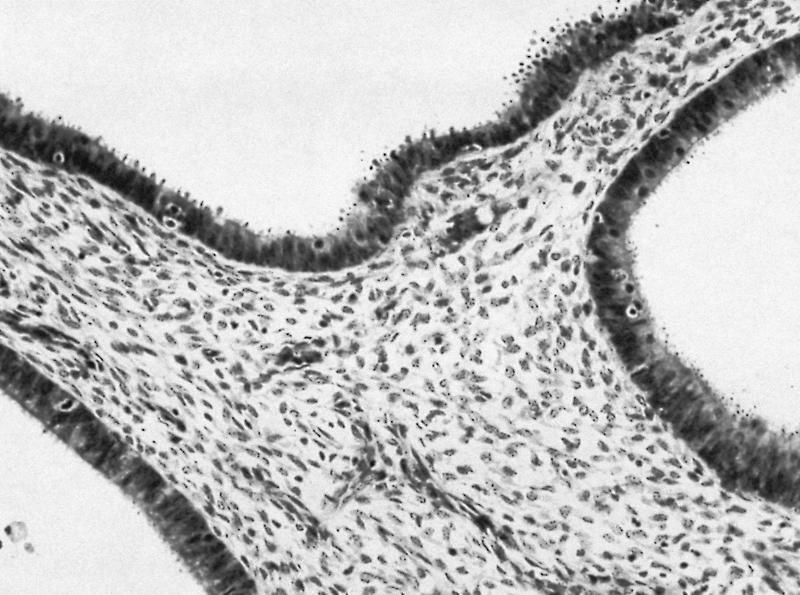
What is simple endometrial hyperplasia?
Simple endometrial hyperplasia (without atypia). This type consists of normal cells that aren't likely to be cancerous. This condition may improve without treatment. Simple or complex atypical endometrial hyperplasia. This type is precancerous and results from an overgrowth of abnormal cells.
What is benign endometrial hyperplasia?
Quick Summary: Benign Endometrial Hyperplasia is a condition that occurs in the endometrium due to an abnormally increased growth of the endometrial glands. It results in an uncharacteristic thickening of the endometrium (lining of the uterus) The condition is also known as Endometrial Hyperplasia without Atypia.
Is benign endometrial hyperplasia a complication?
The most important and significant complication of Benign Endometrial Hyperplasia is that it portends a high risk for endometrial carcinoma (sometimes, as high as 10 times)
What is endometrial hyperplasia?
A note from Cleveland Clinic. Endometrial hyperplasia is a condition that causes abnormal uterine bleeding. These symptoms can be uncomfortable and disruptive. Many women find relief through progestin hormone treatments. Women who have atypical endometrial hyperplasia have a higher risk of developing uterine cancer.
What are the risk factors for endometrial hyperplasia?
Other risk factors include: Certain breast cancer treatments ( tamoxifen ). Diabetes. Early age for menstruation or late onset of menopause.
What hormones are produced by endometrial hyperplasia?
Women who develop endometrial hyperplasia produce too much estrogen and not enough progesterone. These female hormones play essential roles in menstruation and pregnancy. During ovulation, estrogen thickens the endometrium, while progesterone prepares the uterus for pregnancy. If conception doesn’t occur, progesterone levels drop. The progesterone drop triggers the uterus to shed its lining as a menstrual period.
Does endometrial hyperplasia cause estrogen to rise?
Women who have endometrial hyperplasia make little, if any, progesterone. As a result, the uterus doesn’t shed the endometrial lining. Instead, the lining continues to grow and thicken. Additionally, obesity contributes to the elevation of estrogen levels.
Is endometrial hyperplasia cancerous?
Simple endometrial hyperplasia (without atypia): This type of endometrial hyperplasia has normal-looking cells that aren’t likely to become cancerous. This condition may improve without treatment. Hormone therapy helps in some cases.
Can endometrial hyperplasia cause uterine cancer?
Atypical endometrial hyperplasia raises the risk of endometrial cancer and uterine cancer. The condition tends to occur during or after menopause. Progestin therapy can ease symptoms. Women at risk for cancer may choose to get a hysterectomy.
Does obesity cause endometrial hyperplasia?
The adipose tissue (fat stores in the abdomen and body) can convert the fat producing hormones to estrogen. This is the how obesity contributes to elevated circulating levels of estrogen and increases the risk of endometrial hyperplasia. Cleveland Clinic is a non-profit academic medical center.
What is EH with atypia?
EH represents a continuum of histologically distinct processes, starting from simple EH without atypia and then progress to complex EH with atypia, followed by well-differentiated endometrial carcinoma (Fig. 1) [38]. The presence and severity of cytological atypia and architectural crowding are key factors defining the risk for progression to carcinoma. Simple hyperplasia shows the lowest risk of cancer progression, and most cases (80%) of this naturally regress [13,39]. Among patients with atypical hyperplasia, postmenopausal status is associated with the highest risk of progression to adenocarcinoma [16]. Simple hyperplasia is associated with 3% and 8% rates of progression to complex hyperplasia and simple atypical hyperplasia, respectively. Complex hyperplasia has an intermediate risk of progression, which has been shown to regress in most of cases, while EH with cytological atypia is characterized as direct precancerous lesions and may carry a higher risk of progression to carcinoma [40]. Another study reported progression to EC in 1% of patients with simple hyperplasia, 3% of patients with complex hyperplasia, 8% of patients with simple atypical hyperplasia, and 29% of patients with complex atypical hyperplasia [13]. A recent study reported that 2% of the cases with complex hyperplasia (8/390) progressed to EC and 10.5% into atypical hyperplasia, while 52% of the atypical hyperplasia progressed into EC [41].
What is the best treatment for EH?
Although there is no bona fide treatment for EH, most current guidelines recommend hormone therapies (including use of progestin, gonadotropin-releasing hormone (GnRH) or its analogues or their combination) or surgical treatment (Fig. 1). The selection criteria for treatment options are based on patient age, health, the presence of cytologic-atypia and fertility status (Fig. 2). EH without atypia responds well to progestins. Hormone therapy is also recommended for women whose general health prevents them from tolerating surgery due to coexisting medical conditions. However, women with atypical EH or persistent EH without atypia that are symptomatic (abnormal uterine bleeding) are treated with hysterectomy. Among women hoping for childbirth, EH treatment is challenging, demanding conservative treatment regardless of whether the hyperplasia is with or without atypia.
Is EH a precursor to cancer?
Since EH is a precursor to cancer, all risk -factors of EC could be related to EH (Table 2). Postmenopausal, nulliparous, and infertile women are at greater risk of developing EH [42,43]. Diabetes, hypertension, and obesity are also associated with increased EH risk [13,44]. In addition to elevated estrogen levels, obesity causes chronic inflammation that can promote hyperplasia and cancer development [8]. When compared with non-obese ones, obese women (body mass index [BMI] >30 kg/m2) exhibited a nearly 4-fold increase in the incidence of atypical EH. Furthermore, women with a BMI of 40 kg/m2showed a 13-fold increased risk of EH with atypia and a 23-fold increased risk of EH without atypia [45].
Can EH be treated with EC?
Since EH with atypia may progress to or coexist with EC [21], it is of clinical importance and should not be ignored. Moreover, conservative treatment with progestins is designed to regress hyperplasia to normal endometrium to prevent subsequent development of adenocarcinoma [22]. However, hormonal management of women with EH has largely been based on case studies, the efficacy of which has not been well assessed. The lack of standard and conservative treatment options emphasizes the need for new therapies. In this review, we discuss the etiology and risk factors for EH and the related advancement or existing therapies.
What are the two types of endometrial hyperplasia?
There are two main types of endometrial hyperplasia, depending on whether they involve unusual cells, known as atypia. The two types are: Endometrial hyperplasia without atypia. This type doesn’t involve any unusual cells. Atypical endometrial hyperplasia. This type is marked by an overgrowth of unusual cells and is considered precancerous.
Why is my endometrial hyperplasia so bad?
But if you have too much or too little, things can get out of sync. The most common cause of endometrial hyperplasia is having too much estrogen and not enough progesterone. That leads to cell overgrowth. There are several reasons you might have a hormonal imbalance:
What is the term for the thickening of the endometrium?
Endometrial hyperplasia refers to the thickening of the endometrium. This is the layer of cells that line the inside of your uterus. When your endometrium thickens, it can lead to unusual bleeding.
How long does it take for endometrial hyperplasia to show?
The following can all be signs of endometrial hyperplasia: Your periods are getting longer and heavier than usual. There are fewer than 21 days from the first day of one period to the first day of the next. You’re experiencing vaginal bleeding even though you’ve reached menopause.
Can you have endometrial hyperplasia if you have vaginal bleeding?
You’re experiencing vaginal bleeding even though you’ve reached menopause. And, of course, unusual bleeding doesn’t necessarily mean you have endometrial hyperplasia. But it can also be the result of a number of other conditions, so it’s best to follow up with a doctor.
Is hyperplasia cancerous?
Most of the time, it isn’t cancerous and responds well to treatment. Follow up is very important to ensure that hyperplasia isn’t progressing into atypical cells. Continue to have regular checkups and alert your doctor to any changes or new symptoms.
Can atypia go away on its own?
future pregnancy plans. personal and family history of cancer. If you have simple hyperplasia without atypia, your doctor might suggest just keeping an eye on your symptoms. Sometimes, they don’t get worse and the condition may go away on its own.
