What medications cause second degree heart block?
- Mechanism. This is usually a result of a reversible conduction block at the level of the AV node. ...
- Causes. There are multiple causes of second-degree Mobitz type 1 (Wenckebach) AV block, including reversible ischemia, myocarditis, increased vagal tone, status post-cardiac surgery, or even medications that slow AV nodal ...
- Clinical significance. ...
What are symptoms of second degree heart block?
Symptoms of second- and third-degree heart block include fainting, feeling dizzy or lightheaded, fatigue (tiredness), shortness of breath, and chest pain. Heart block may be diagnosed as part of a routine doctor’s visit or during an emergency situation (third-degree heart block is an emergency).
What is the prognosis for heart block?
With second-degree, you may:
- Get tired
- Feel dizzy or faint
- Have a slow heart rate
- Skip heartbeats
- Have trouble breathing
- Get chest pain
- Feel sick to your stomach
When is a pacemaker needed for heart block?
You treatment depends on the type of heart block you have: With first-degree heart block, you might not need treatment. With second-degree heart block, you may need a pacemaker if symptoms are present or if Mobitz II heart block is seen. With third-degree heart block, you will most likely need a pacemaker.

Does second-degree heart block need treatment?
You treatment depends on the type of heart block you have: With first-degree heart block, you might not need treatment. With second-degree heart block, you may need a pacemaker if symptoms are present or if Mobitz II heart block is seen. With third-degree heart block, you will most likely need a pacemaker.
What medication is given for heart block?
Medications that may be used in the management of third-degree AV block (complete heart block) include sympathomimetic or vagolytic agents, catecholamines, and antidotes.
How do you treat symptomatic second-degree heart block?
Symptomatic patients should be treated with atropine and transcutaneous pacing. However, atropine should be administered with caution in patients with suspected myocardial ischemia, as ventricular dysrhythmias can occur in this situation.
Is heart block curable by medicine?
There is no heart-block-specific treatment. Most people with bundle branch block have no symptoms, and they do not require treatment. However, any underlying causes, such as hypertension, will need treatment. Share on Pinterest Patients with second- or third-degree heart block may need a pacemaker.
Can heart blockage be removed by medicine?
In serious cases, medical procedures or surgery can help to remove blockages from within the arteries. A doctor may also prescribe medication, such as aspirin, or cholesterol-reducing drugs, such as statins.
How serious is second-degree heart block?
Second-degree heart block may develop into a more serious type of heart block. It may cause a sudden loss of consciousness or it may cause the heart to suddenly stop beating.
Is atropine used for complete heart block?
In your AHA provider manual, you will see it stated in the bradycardia section that atropine is not effective for Mobitz II and complete heart block.
Is a pacemaker the only treatment for bradycardia?
Bradycardia treatment may include lifestyle changes, medication changes or an implanted device called a pacemaker. If an underlying health problem, such as thyroid disease or sleep apnea, is causing the slow heart rate, treatment of that condition might correct bradycardia.
What are the symptoms of a second degree heart block?
Symptoms may include: Chest pain. Lightheadedness, faintness, or dizziness. Feeling tired. Shortness of breath.
What happens when a second heart block is not completed?
With the second type of second-degree heart block, some electrical signals are not relayed from the upper chambers to the lower chambers.
What is a heart block?
Heart block is a condition in which the electrical wiring system of the heart does not work properly. Sometimes it can result in a slow heartbeat that is either regular or irregular. This may cause symptoms.
Do you need a pacemaker for a second degree heart block?
Most people who have the second type of second-degree heart block will need a pacemaker even if they have no symptoms. This type of heart block often can progress to more serious type of heart block that can be potentially dangerous.
Can a second degree heart block be treated?
Second-degree heart block without symptoms may not need treatment. Your healthcare provider is likely to ask you to have regular follow-up visits. You may also be asked to take your own pulse and be alert to changes in your heart rate.
What is AV block type 2?
A second-degree AV block type II rhythm is an indication that a patient will likely require a permanent pacemaker; transvenous pacing will be necessary until a permanent pacemaker is placed.
Why is pacing important in AV block?
Pacing. Because there is a risk for patients with a cardiac rhythm of a second-degree AV block type II to deteriorate clinically into a complete heart block (third-degree AV block) or ventricular asystole, it is imperative that pacing be considered in patients who are hemodynamically unstable due to bradycardia.
How often should I take atropine for AV block?
For the patient with poor perfusion due to a consistent second-degree AV block type II, the ACLS Adult Bradycardia Algorithm recommends starting with 1mg of atropine administered intravenously, which can be repeated every 3-5 minutes, up to a total dose of 3mg. Although atropine is indicated as a first-line medication in the ACLS Adult Bradycardia Algorithm, patients with a second-degree AV block type II may not respond to this medication or it may worsen the heart block, increasing the risk for clinical deterioration to a complete heart block or ventricular asystole. If the atropine is not effective, the healthcare provider can administer beta-adrenergic medications while concurrently preparing the patient for pacing.
What is AV block?
QRS complexes in this rhythm tend to be wide. In a third-degree AV block (also known as a complete AV block), atrial impulses cannot initiate ventricular contraction, resulting in an escape rhythm that paces the ventricles at an inherent rate.
What is the first step in care for a patient?
Initial steps the healthcare provider should take in caring for a patient, according to the Advanced Cardiac Life Support (ACLS) Primary Assessment, are to manage the patient's airway, provide supplemental oxygen if needed, determine the patient's cardiac rhythm, and monitor vital signs.
Is atropine a first line treatment for bradycardia?
Beta-adrenergics. Dopamine and epinephrine infusions are not considered first-line treatments for unstable bradycardia. However, when the patient does not respond to the administration of atropine, these medications can be used as alternatives.
Can ACLS perform TCP?
TCP can be performed by ACLS providers and should be urgently considered in symptomatic patients experiencing poor perfusion with a second-degree AV block type II. TCP can be painful for the patient; patients who are conscious should be sedated prior to this intervention, if possible.
What is a Second-Degree AV Block Type I?
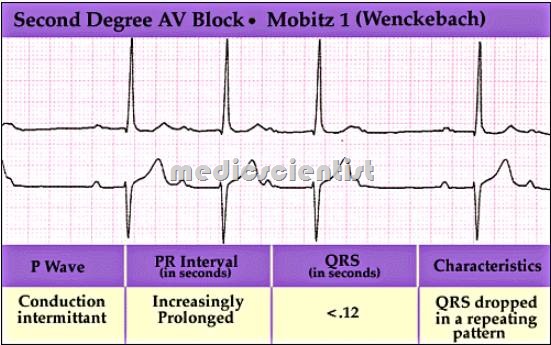
An atrioventricular block, in general, occurs when there is a conduction delay between the atria and ventricles of the heart. A second-degree atrioventricular (AV) block type I is also known as Wenckebach or Mobitz type I. This rhythm occurs at the AV node, where conduction of an electrical impulse is impaired.
What Signs or Symptoms May be Present?
A patient with a second-degree AV block type I may have the following signs or symptoms:
What Causes a Second-Degree AV Block Type I?
This heart block is generally considered benign. Most commonly, there is little hemodynamic disruption, and patients are largely asymptomatic.
Treatment of Second-Degree AV Block Type I
It is essential to identify the difference between a second-degree AV block type I (Wenckebach or Mobitz type I) and type II (Mobitz type II) as the management approach to each is different. Patients with a second-degree AV block type I may be asymptomatic.
Next Steps & Considerations
A second-degree AV block type I bradyarrhythmia is often benign; many patients are asymptomatic. If this rhythm was induced by a medication, the rhythm disturbance often reverses after the medication’s cessation or a dosing modification - this would warrant management through expert consultation.
FAQs
Understanding the difference between second-degree AV blocks type I and type II is key to providing accurate and effective patient care. A second-degree AV block type I occurs at the AV node of the heart. On an ECG, the PR interval gradually lengthens until the QRS complex ‘drops’ (more P waves are present than QRS complexes).
How to Prepare for Your ACLS or PALS Exam
Achieving and maintaining these certifications ensures that you are a knowledgeable and skillful healthcare provider ready to respond and care for patients experiencing life-threatening cardiac emergencies. To earn this certification, you’ll need to master common ECG rhythms and the appropriate procedures to respond to each.
What is the mildest heart block?
First-degree heart block: The electrical impulse still reaches the ventricles, but moves more slowly than normal through the AV node. The impulses are delayed. This is the mildest type of heart block. Second-degree heart block is classified into two categories: Type I and Type II.
What medications slow the heart's electrical impulses?
You take medications that slow the conduction of the heart’s electrical impulses including some heart medications (beta blockers, calcium channel blockers, digoxin), high blood pressure drugs, antiarrhythmics; muscle relaxants and sedatives; antidepressants and antipsychotics; diuretics; lithium.
What is the name of the block that makes your heart beat?
Heart Block. Heart block, also called AV block, is when the electrical signal that controls your heartbeat is partially or completely blocked. This makes your heart beat slowly or skip beats and your heart can’t pump blood effectively. Symptoms include dizziness, fainting, tiredness and shortness of breath. Pacemaker implantation is ...
What is the purpose of an electrophysiology study?
An electrophysiology study: An electrophysiology study involves inserting a long, thin tube called a catheter through a blood vessel and guiding it to your heart to measure and record electrical activity from inside your heart. If you need this test, you’ll get more detailed information.
How to keep your heart healthy?
Steps you can take to keep your heart and body as healthy as possible include: Lead a heart-healthy lifestyle, which includes eating a heart healthy diet, exercising regularly, getting an adequate amount of sleep each night, reducing stress, limiting alcohol and stopping smoking and use of illicit drugs.
How long do you need to wear a Holter monitor?
You may need to wear a portable ambulatory monitor device, such as a Holter monitor or an event recorder, for 24 to 48 hours or longer to collect more information about your heart’s electrical activity. If you need to use a monitor, you’ll get detailed information about how to use it.
Do you need a pacemaker for a heart block?
Second-degree block: If you have second-degree heart block and have symptoms, you may need a pacemaker to keep your heart beating like it should. A pacemaker is small device that sends electrical pulses impulses to your heart.
What is the difference between a first degree heart block and a second degree heart block?
The electrical signals slow down as they move from your atria to your ventricles. First-degree heart block might not require treatment of any kind. Second-degree heart block means that the electrical signals between your atria and ventricles can intermittently fail to conduct. There are 2 types of second-degree heart block.
How to prevent heart block?
A healthy lifestyle contributes to overall good health — including heart health. Exercise, eat a well-balanced diet, and don’t smoke. Understanding the risks of your medicines and reviewing them with your healthcare provider can reduce the risk of medicine-induced heart block.
What happens when your heart is blocked?
When you have heart block, there is interference with the electrical signals that usually move from the atria to the ventricles. These signals tell your heart when to beat. This is known as a conduction disorder. If the electrical signals can’t move from your atria to your ventricles, they can’t tell your ventricles to contract ...
What causes wire damage in the heart?
Cardiomyopathies which are diseases that weaken the heart muscle can also result in wire damage. Any disease that can infiltrate the heart such as sarcoidosis and certain cancers or any disease that results in heart inflammation such as certain autoimmune disease or infections can result in heart block.
How to improve quality of life with pacemaker?
Also, always keep follow-up appointments to make sure your treatment is on track. To improve your quality of life with a pacemaker, you may need to: Avoid situations in which your pacemaker may be disrupted, such as being near an electrical device or devices with strong magnetic fields.
Can heart block cause heart failure?
First degree heart block may cause minimal problems, however third degree heart block can be life-threatening. Heart block may cause no symptoms or it may cause dizziness, fainting, the feeling of skipped heart beats, chest pain, difficulty breathing, fatigue, or even cardiac arrest.
Do you need a pacemaker for a heart block?
You treatment depends on the type of heart block you have: With first-degree heart block, you might not need treatment. With second-degree heart block, you may need a pacemaker if symptoms are present or if Mobitz II heart block is seen . With third-degree heart block, you will most likely need a pacemaker.
Can atropine be given with ventricular dysrhythmia?
However, atropine should be administered with caution in patients with suspected myocardial ischemia, as ventricular dysrhythmias can occur in this situation. The goal of atropine administration is to improve conduction through the AVN by reducing vagal tone via atropine-induced receptor blockade.
Is it safe to implant a pacemaker outside of conventional criteria?
In some cases, depending on the type of the implanted valve, baseline electrocardiographic (ECG) features, degree and location of the aortic valve calcification, and the patient's comorbidities, implanting a permanent pacemaker outside of conventional criteria may be a reasonable and safe approach.
Is atropine effective for denervated heart?
In addition, in patients who have denervated hearts (eg, patients who have undergone a cardiac transplant), atropine is also not likely to be effective. Admit all patients to a unit with monitored beds, where transcutaneous and transvenous pacing capabilities are available.
Does AV block require atropine?
Second-degree atrioventricular (AV) block in the asymptomatic patient does not require any specific therapy in the prehospital setting. If the patient is symptomatic, standard advanced cardiac life support (ACLS) guidelines for bradycardia, including the use of atropine and transcutaneous pacing, are indicated. [ 11, 33]
What happens after a heart block?
Life After Heart Block . Your heartisn’t plugged into an outlet. And you don’t use a switch to turn it on. But just like a lamp, your heartruns on an electrical system. Every time your heart beats, an electrical signal travels from the upper to the lower chambers. Along the way, the signal tells your heart to contract and pump blood.
What is the name of the monitor that a doctor will use to check your heart?
They may also ask you to wear a monitor, called a Holter, for anywhere from a day to a month to track the rhythm of your heart. Treatment.
Is a pacemaker considered a minor surgery?
This is considered “minor” surgery and you’ll be sedated for it. Like a backup electrical system, it reminds the heart to beat at a normal rate if it slows or stops. Life After Heart Block. Just like your heart, your pacemaker needs to be treated right to work well.
What is the treatment for AV block type 2?
Second-degree AV block (Type 2) should be treated with immediate transcutaneous pacing or transvenous pacing because there is risk that electrical impulses will not be able to reach the ventricles and produce ventricular contraction.
What causes heart block type 2?
Second-degree heart block type 2 is usually caused by structural damage to the conduction system of the heart. Causes of the structural damage to the conduction system include the following:
What is the most common P wave block?
If every third P-wave is blocked, then there is 3-to-2 block (which is the most common). If every fourth P-wave is blocked, it is classified as 4-to-3 block, which is less common. 5-to-4 block is even more uncommon.
Does Mobitz block progress to advanced blocks?
The prognosis is good, even in the elderly. Mobitz type 1 block generally does not progress to more advanced blocks. Should it progress to more advanced blocks, which typically is due to a more distal location of the block, an artificial pacemaker is needed.
Is Mobitz type 1 block good?
It is also common among athletes due to their high vagal tone. It is more common in older individuals. The prognosis is good, even in the elderly. Mobitz type 1 block generally does not progress to more advanced blocks. Should it progress to more advanced blocks, which typically is due to a more distal location of the block, an artificial pacemaker is needed.
Is Mobitz type 2 block a sporadically block?
Mobitz type 2 block implies that some atrial impulses are blocked sporadically. The PR interval is constant (although it may be prolonged). Mobitz type 2 is more serious, because it is usually chronic and tends to progress to third-degree AV block. Moreover, cardiac output may be reduced if many impulses are blocked.

What Are The ECG Characteristics of A Second-Degree Av Block Type II?
What Signs Or Symptoms May Be present?
- A patient with a second-degree AV block type II may exhibit: 1. Shortness of breath 2. Fatigue 3. Diaphoresis 4. Pallor 5. Chest pain 6. Altered mental status 7. Loss of consciousness 8. Bradycardia 9. Hypotension
What Causes A Second-Degree Av Block Type II?
- This type of heart block may be attributed to structural damage within the AV conduction system of the heart. Patients exhibiting this heart dysrhythmia often have underlying heart disease. Potential causes of this rhythm include: 1. Myocardial ischemia 2. Myocardial infarction 3. Infiltrative cardiomyopathies (such as hemochromatosis, amyloidosis, sarcoidosis) 4. Idiopathi…
Treatment of Second-Degree Av Block Type II
- Initial steps the healthcare provider should take in caring for a patient, according to the Advanced Cardiac Life Support (ACLS) Primary Assessment, are to manage the patient's airway, provide supplemental oxygen if needed, determine the patient's cardiac rhythm, and monitor vital signs. Intravenous access should be obtained, as well as a 12-lead E...
FAQs
- What is the difference between type I and type II second-degree AV blocks?
A second-degree AV block type I occurs at the AV node. Each impulse is gradually prolonged until one is unsuccessful at being conducted to the ventricles. With this rhythm, the PR interval lengthens gradually until a QRS complex is dropped; there are more P waves than QRS complexe… - What is the difference between a second-degree AV block type II and a third-degree AV block?
In a second-degree AV block type II, AV conduction is irregularly blocked below the AV node. There are more P waves than QRS complexes, P waves are consistent and regular, PR intervals are uniform, and QRS complexes drop unexpectedly. QRS complexes in this rhythm tend to be wi…
Preparing For Your Acls Or Pals Exam
- Mastery of rhythms such as this are key to passing your ACLS or PALS exam, and being prepared to respond effectively when a patient is experiencing a cardiac emergency. That’s why the American Medical Resource Institute (AMRI) incorporates a multidisciplinary teaching approach that utilizes clinical scenarios through an expansive library of case studies to provide meaningfu…
Clinical significance
- In people with heart block, also called AV block, the electrical signal that controls the heartbeat is partially or completely blocked from reaching the ventricles.
Classification
- Heart block is classified as first-, second- or third-degree, depending on the extent of electrical signal impairment.
Overview
- Type I heart block (also called Mobitz Type I or Wenckebach's AV block) is the less serious form of second-degree heart block. In this condition, the electrical signal goes slower and slower until the heart actually skips a beat.
Symptoms
- In patients with Type II heart block (also called Mobitz Type II), some of the electrical signals do not reach the ventricles, and the pattern is irregular. Individuals with this type of heart block may have a heartbeat that is slower than normal. The area that is blocked is lower in the conduction system and is often associated with more severe conduction disease. Symptoms of second- an…
Mechanism
- In patients with third-degree (complete) heart block, the electrical signal is not sent from the atria to the ventricles. The heart compensates by producing electrical signals from a specialized pacemaker area in the ventricles. These signals make the heart contract and pump blood, but at a rate that is much slower than normal.
Signs and symptoms
- First-degree heart block often does not cause symptoms. It may be detected during a routine electrocardiogram (ECG/EKG), but the patients heart rate and rhythm are usually normal.
Causes
- Acquired heart block has many possible causes, including heart attack (the most common cause), heart disease, an enlarged heart (cardiomyopathy), heart failure and rheumatic fever. Sometimes heart block occurs as a result of injury to the heart during open heart surgery, as a side effect of some drugs, or after exposure to a toxin.