Removal of placental pieces that remain in the uterus
- KQ1-3, 5: Women with postpartum hemorrhage (PPH) immediately post-birth to 12 weeks postpartum following pregnancy >24 weeks’ gestation
- KQ4: Women with stabilized PPH and acute blood loss anemia
- All modes of birth in any setting
Examination of the uterus and other pelvic tissues
What are the 3 main causes of postpartum hemorrhage?
- Placental abruption. The early detachment of the placenta from the uterus.
- Placenta previa. The placenta covers or is near the cervical opening.
- Overdistended uterus.
- Multiple pregnancy.
- Gestational hypertension or preeclampsia.
- Having many previous births.
- Prolonged labor.
- Infection.
Hysterectomy
Yes. It's common for postpartum bleeding (lochia) to last for at least a couple of weeks if not longer than a month. It's different for every woman. Postpartum bleeding typically stops after four to six weeks. What Should Postpartum Bleeding Look Like? It can depend on how much time has passed since you gave birth.
Medication
- Retained products of conception
- Infection
- Subinvolution of the placental site
- Inherited coagulation deficits
Manual massage of the uterus
How to manage postpartum hemorrhage?
What are the 4 most common causes of postpartum hemorrhage?
Is it normal to bleed 3 months postpartum?
What are the stages of postpartum hemorrhage?

How do doctors treat postpartum hemorrhage?
It may include: Getting fluids, medicine (like Pitocin) or having a blood transfusion (having new blood put into your body). You get these treatments through a needle into your vein (also called intravenous or IV), or you may get some directly in the uterus. Having surgery, like a hysterectomy or a laparotomy.
What is the first priority in management of postpartum hemorrhage?
External uterine massage and bimanual compression are generally used as first-line treatments. These compression techniques encourage uterine contractions that counteract atony and assist with expulsion of retained placenta or clots. Aortic compression is another compression technique that has been used for severe PPH.
What Medication is given to stop postpartum hemorrhage?
Oxytocin is the drug of choice for preventing postpartum hemorrhage because it is at least as effective as ergot alkaloids or prostaglandins and has fewer side effects.
What interventions does the nurse do for postpartum hemorrhage?
Nursing Interventions Save all perineal pads used during bleeding and weigh them to determine the amount of blood loss. Place the woman in a side lying position to make sure that no blood is pooling underneath her. Assess lochia frequently to determine if the amount discharged is still within the normal limits.
How does oxytocin stop bleeding?
Oxytocin controls bleeding after the birth of a child by tightening the blood vessels of the uterus. Oxytocin causes the uterus to contract, which helps to close uterine blood vessels. When blood vessels tighten, they release less blood.
How much blood loss is considered a postpartum hemorrhage?
Traditionally, postpartum hemorrhage (PPH) has been defined as greater than 500 mL estimated blood loss associated with vaginal delivery or greater than 1000 mL estimated blood loss associated with cesarean delivery.
Why is oxytocin given in postpartum haemorrhage?
Oxytocin prevents excessive postpartum bleeding by helping the uterus to contract. It is given to the mother by injection into a vein or into muscle during or immediately after the birth of her baby.
Is there any injection to stop bleeding during pregnancy?
Tranexamic acid has been proposed and used for prevention and management of antepartum and postpartum hemorrhage. Detailed Description: Bleeding during pregnancy is associated with a three- to fourfold increase in perinatal mortality.
Which of the following is the best strategy to prevent a postpartum hemorrhage?
The most effective strategy to prevent postpartum hemorrhage is active management of the third stage of labor (AMTSL). AMTSL also reduces the risk of a postpartum maternal hemoglobin level lower than 9 g per dL (90 g per L) and the need for manual removal of the placenta.
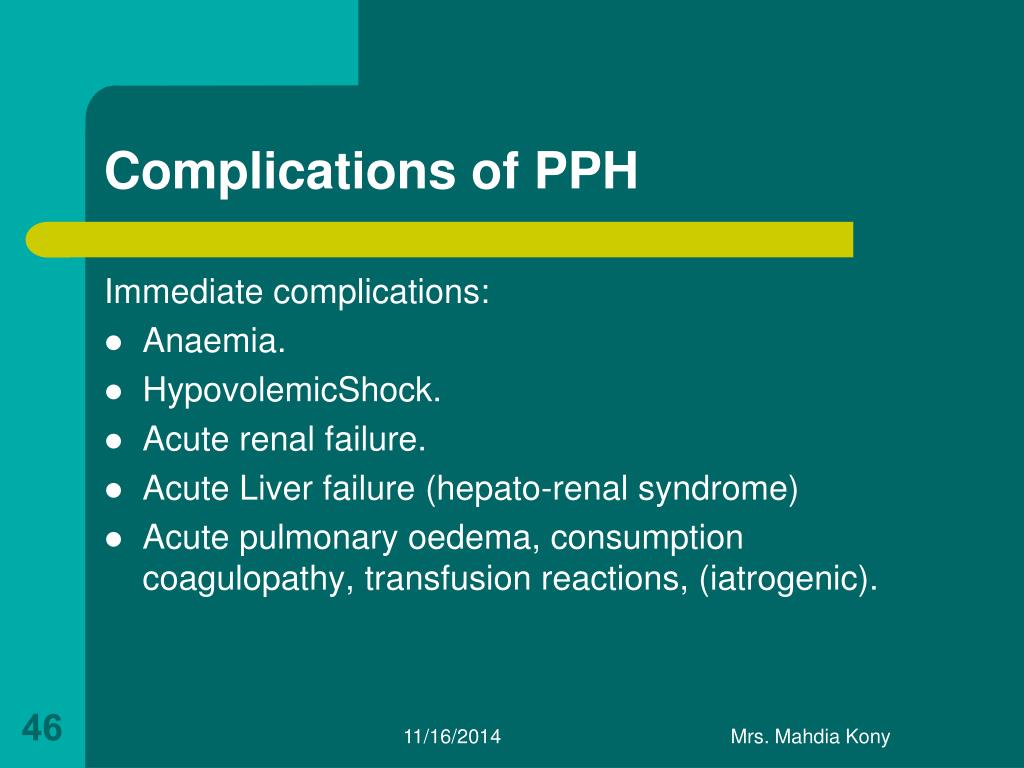
What are the complications of postpartum hemorrhage?
Complications include sterility, uterine perforation, uterine synechiae (Asherman syndrome), urinary tract injury and genitourinary fistula, bowel injury and genitointestinal fistula, vascular injury, pelvic hematoma, and sepsis.
What are the risk factors for postpartum hemorrhage?
Risk factors for postpartum hemorrhage include the following: placental abruption - the early detachment of the placenta from the uterus. placenta previa - the placenta covers or is near the cervical opening. overdistended uterus - excessive enlargement of the uterus due to too much amniotic fluid or a large baby, ...
What percentage of women have postpartum hemorrhage?
Postpartum hemorrhage is excessive bleeding following the birth of a baby. About 4 percent of women have postpartum hemorrhage and it is more likely with a cesarean birth. Hemorrhage may occur before or after the placenta is delivered. The average amount of blood loss after the birth of a single baby in vaginal delivery is about 500 ml ...
How much blood loss is there after a cesarean birth?
The average amount of blood loss for a cesarean birth is approximately 1,000 ml (or one quart). Most postpartum hemorrhage occurs right after delivery, but it can occur later as well.
What is the procedure to remove bleeding blood vessels?
tying-off of bleeding blood vessels. laparotomy - surgery to open the abdomen to find the cause of the bleeding. hysterectomy - surgical removal of the uterus; in most cases, this is a last resort. Replacing lost blood and fluids is important in treating postpartum hemorrhage.
What happens to the uterus after a baby is born?
Once a baby is delivered, the uterus normally continues to contract (tightening of uterine muscles) and expels the placenta. After the placenta is delivered, these contractions help compress the bleeding vessels in the area where the placenta was attached.
What happens if the placenta doesn't contract?
After the placenta is delivered, these contractions help compress the bleeding vessels in the area where the placenta was attached. If the uterus does not contract strongly enough, called uterine atony, these blood vessels bleed freely and hemorrhage occurs. This is the most common cause of postpartum hemorrhage.
What percentage of women have postpartum hemorrhage?
Postpartum hemorrhage is excessive bleeding following the birth of a baby. About 1 to 5 percent of women have postpartum hemorrhage and it is more likely with a cesarean birth. Hemorrhage most commonly occurs after the placenta is delivered. The average amount of blood loss after the birth of a single baby in vaginal delivery is about 500 ml ...
What is the placenta attached to?
The placenta is abnormally attached to the inside of the uterus (a condition that occurs in one in 2,500 births and is more common if the placenta is attached over a prior cesarean scar). Placenta increta. The placental tissues invade the muscle of the uterus. Placenta percreta.
What is the placenta previa?
Placenta previa. The placenta covers or is near the cervical opening. Overdistended uterus. Excessive enlargement of the uterus due to too much amniotic fluid or a large baby, especially with birthweight over 4,000 grams (8.8 pounds).
What does postpartum hemorrhage feel like?
Swelling and pain in tissues in the vaginal and perineal area, if bleeding is due to a hematoma. The symptoms of postpartum hemorrhage may resemble other conditions or medical problems. Always consult your doctor for a diagnosis.
What is the purpose of a Bakri balloon?
Bakri balloon or a Foley catheter to compress the bleeding inside the uterus. Packing the uterus with sponges and sterile materials may be used if a Bakri balloon or Foley catheter is not available. Tying-off of bleeding blood vessels using uterine compression sutures. Laparotomy.
How much blood loss is there after a cesarean birth?
The average amount of blood loss for a cesarean birth is approximately 1,000 ml (or one quart). Most postpartum hemorrhage occurs right after delivery, but it can occur later as well.
Is oxytocin used in labor?
Active management of the third stage of labor should be used routinely to reduce its incidence. Use of oxytocin after delivery of the anterior shoulder is the most important and effective component of this practice. Oxytocin is more effective than misoprostol for prevention and treatment of uterine atony and has fewer adverse effects.
Is postpartum hemorrhage a risk factor?
Postpartum Hemorrhage: Prevention and Treatment. Postpartum hemorrhage is common and can occur in patients without risk factors for hemorrhage. Active management of the third stage of labor should be used routinely to reduce its incidence.
What is PPH in medical terms?
Postpartum Haemorrhage (PPH) is a major cause of maternal morbidity and mortality. Treatment of acquired coagulopathy observed in severe PPH is an important part of PPH management, but is mainly based on literature in trauma patients, and data thus should be interpreted with caution. This review describes recent advances in transfusion strategy and in the use of tranexamic acid and fibrinogen concentrates in women with PPH.
What is the role of fibrinogen in hemostasis?
Fibrinogen plays a critical role in achieving and maintaining hemostasis and is fundamental to effective clot formation. In the context of massive obstetric bleeding, fibrinogen is the first coagulation factor to decrease 27; rapid fibrinolysis has also been described in some specific causes of PPH, such as placental abruption, placenta previa, genital tract trauma, and uterine atony.
What is PPH in obstetrics?
PPH is a typical obstetric emergency situation that can develop rapidly and unexpectedly. Health-care professionals taking care of obstetric emergencies act as a team in which each provider uses his or her specific competencies. Moreover, because each obstetric emergency situation is a relatively rare event, even in high-level reference centers, providers have relatively few opportunities to train by self-experience and to evaluate and discuss how previous cases have been managed. During any emergency situation, communication and organizing the process of care are difficult tasks. It has been recognized that in many cases there is no clear leadership 59, and poor teamwork has been recognized as a major cause of poor outcome 60. For each team member, non-technical skills thus represent an important component of competency. Flin and Maran have described non-technical skills as two cognitive competencies (situational awareness and decision making) and two social competencies (teamwork and leadership) 61. Most of these competencies are universal and should be practiced by every health-care provider whatever his or her profession or grade. Unfortunately, using these four skills is difficult and does not come naturally to most humans. Recognition of these deficiencies and subsequent training are thus essential. Unfortunately, traditional teaching is almost ineffective to improve patients’ outcomes. Recently developed strategies have emerged to facilitate adoption of these non-technical skills in clinical practice. Interprofessional education is a relatively recent concept and is said to occur ‘when two or more professions learn with, from and about each other to improve collaboration and the quality of care’ 62. Interprofessional education is believed to be important for undergraduate students 63 but also for professionals working in clinical units to develop or maintain interprofessional collaboration. Team training is gaining popularity, as it is now recognized to improve quality of care 64. Team training as well as interprofessional education for students can be done through formal courses and meetings, but many studies have shown that simulation is effective to improve communication, teamwork, and patients’ outcomes 65 , 66. Quality of care can also be improved by writing protocols that are made available to all providers 67 and through retrospective audits, which reduce the incidence of severe PPH and improve the application of recommendations 68.
What causes postpartum hemorrhage?
The main causes of PPH are uterine atony, retained placenta, and genital tract trauma. Abnormal placentation, placental abruption, and uterine rupture are less frequent but often responsible for severe PPH with acquired coagulopathy. PPH accounts for nearly one-quarter of all maternal deaths worldwide and an estimated 125,000 deaths occur each year 1. Most of the time, these deaths due to obstetric hemorrhage are considered to be potentially preventable 2 , 3. Maternal mortality is the end result of a worsening process, and PPH is also responsible for half of maternal morbidity 4. The incidence of PPH has recently increased in most developed countries such as Canada, Australia, and the US and has been notably related to an increased use of oxytocin for labor augmentation and subsequent uterine atony 5.
What is TA in menorrhagia?
Postpartum hemorrhage and tranexamic acid. TA is an antifibrinolytic agent that inhibits the activation of plasminogen into plasmin. Its use is now clearly established for the control and prophylaxis of menorrhagia 20.
What is a F1000 review?
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
Is fibrinogen available everywhere?
In the past, fibrinogen therapy was usually given as cryoprecipitate, but owing to the potential viral contamination and variable concentration of fibrinogen in cry oprecipitate, human plasma-derived fibrinogen concentrates are now available in most countries but not everywhere.
What is postpartum hemorrhage (PPH)?
PPH is the loss of large amounts of blood after delivery. Most common is early PPH. It happens within 24 hours of delivery. The risk for PPH is greatest within the first hour after delivery. Delayed or late PPH happens 25 hours to 6 weeks after delivery. PPH can be life-threatening no matter when it happens.
What are the causes of early PPH?
Uterine atony means your uterus does not contract after delivery. Atony may be caused by your uterus being stretched too much. It may also be caused if you have had more than 4 vaginal deliveries, long labor, medicines, or fibroids. If parts of the placenta stay in your uterus, it can also cause atony.
How is PPH diagnosed and treated?
Your healthcare provider will diagnose PPH by your symptoms. He or she will also do a pelvic exam. You may also need to have an ultrasound to check your uterus. Treatment may include any of the following:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.