
What are the treatment options for urethral pain?
The treatment of urethral pain depends on the underlying cause. For symptom management, topical lidocaine gel or the medication Pyridium (phenazopyride) may reduce pain (note that Pyridium can turn urine red).
How can I relieve painful urination during menopause?
Hormone treatments may relieve symptoms and can be taken orally or applied to the skin in a cream, yet are not appropriate for all suffering from painful urination during menopause. For such patients, vaginal moisturizers and lubricants can be used to ease symptoms.
What are the treatments for urogenital atrophy in postmenopausal women?
As lack of estrogen is the primary cause of urogenital atrophy, the treatments for it in postmenopausal women involve hormone therapy (HT). These can help restore the vagina to premenopausal condition and relieve many symptoms of urogenital atrophy.
What are the symptoms of urethral prolapse after menopause?
In postmenopausal women, urethral prolapse is usually accompanied by additional symptoms, particularly pain with urination, frequent urination, and an increased need to urinate at night. Postmenopausal women with urethral prolapse are also more likely to have blood in their urine. 1
Can low estrogen cause urethral pain?
The urinary tract is also affected by postmenopausal declining estrogen, which may lead to thinning of the bladder and urethral linings and possibly cause chronic dysuria and an increased incidence of urinary tract infections.
How do you apply estrogen cream to the urethra?
Carefully spread the cream onto the top wall of the vagina just underneath the urethral area (see Figure 2, yellow highlighted area). As the cream is spread, some may be gently inserted into the vagina: however, it is not necessary to push the cream high into the vagina.
Does low estrogen cause urethritis?
Estrogen deprivation will result in atrophic urethritis and sometimes urinary incontinence, and estrogen replacement therapy may reverse this trend.
What is postmenopausal urethral atrophy?
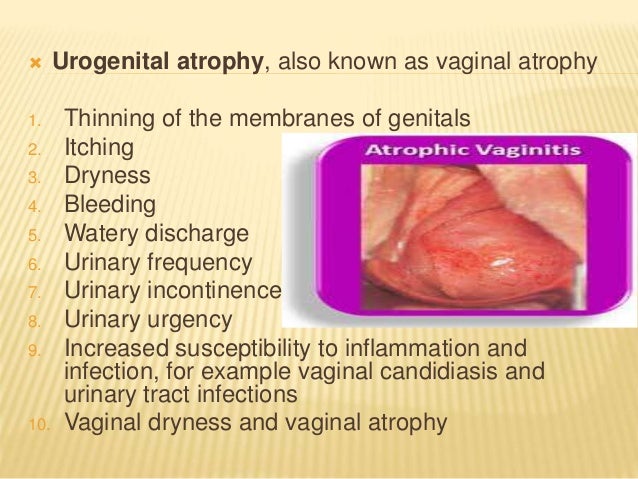
The genitourinary syndrome of menopause (vaginal atrophy or atrophic vaginitis) frequently affects menopausal and postmenopausal women. It's a condition where the lining of the vagina gets drier and thinner from a lack of estrogen.
How do you soothe an irritated urethra?
Home care for urethritis relieves its symptoms.Drink fluids to dilute your urine. ... You may take nonsteroidal anti-inflammatory medications (such as ibuprofen) and acetaminophen (for example, Tylenol) for pain control.Sitz baths can help with the burning associated with chemical irritant urethritis.More items...
How do you treat an inflamed urethra?
Treatment for urethritis typically includes a course of either antibiotics or antiviral medication. Some common treatments for urethritis include: azithromycin, an antibiotic, typically taken as a one time dose. doxycycline, an oral antibiotic that is typically taken twice a day for seven days.
How do you treat an inflamed urethra naturally?
You may use tinctures alone or in combination as noted.Cranberry ( Vaccinium macrocarpon ). Supplements to help prevent urethritis and urinary tract infections. You may also drink 8 to 16 ounces of unsweetened cranberry juice daily. ... Bromelain ( Ananus comosus ). For pain and inflammation.
What happens to the urethra after menopause?
The lack of estrogen weakens the bladder (which holds urine) and the urethra, the tube that carries urine out of the body, compromising their ability to control urinary functions.
Can menopause cause urethritis?
Lack of the female hormone estrogen causes the tissues of the urethra and bladder to get thinner and drier after menopause. This is a common cause of urethritis in older women.
How long does an inflamed urethra take to heal?
In most cases, the symptoms should resolve in a week or two and you should not need further treatmentIf you have had sex or did not take the medication as directed, or have persistent symptoms for longer than two weeks, you should consult a doctor.
Does estrogen cream help interstitial cystitis?
Estrogen Cream Improves Urinary and Sexual Symptoms in Pre-Menopausal Women with IC/BPS - Interstitial Cystitis Association.
Does vagifem help with urinary problems?
Vaginal oestrogen therapy (Vagifem, Ovestin) is likely to be helpful in postmenopausal women to decrease urinary frequency, urgency and the need to pass urine at night (nocturia). These are used 2-3 times at week and are inserted into the vagina at night.
What is TCM medicine?
According to the medical report, TCM (traditional Chinese medicine) is accepted by more and more patients. Take the herbal medicine Diuretic and Anti-inflammatory Pill for example, the herbal medicine has strong broad-spectrum antimicrobial, bactericidal effect, it can effectively kill the pathogens like bacteria, virus, chlamydia, mycoplasma, gonorrhoeae, etc. Besides, it has functions like promoting diuresis and relieving stranguria, it can eliminate the symptoms of frequency and urgency. What is more, the herbal medicine is made from natural herbs; it is safe and without drug resistance and side effect to liver and kidney.
How long does menopause last?
The menopause period lasts 10 – 20 years, during this period, due to the reduced secretion of sex hormones, the ovarian function will decline, leading to urogenital atrophy. Therefore, women are easy to appear the symptoms like vaginal dryness, itching, sexual difficulties, etc.
Why do you need a routine urianlysis?
In fact, at this time, patients should take a routine urianlysis and secretions culture to confirm the pathogens of the urethritis. If the disease is caused by reduced hormone, hormone therapy is necessary.
Is urethritis a gynecological disease?
Commonly, when suffering from urethritis, women will classify it as gynecological disease. And after menopause, the chances of suffering from gynecological diseases will be reduced, so they think that the chances of suffering from urethritis can also be reduced. However, in fact, this argument is biased.
Is TCM safe for menopause?
To sum up, if women have urethritis after menopause, they can choose the TCM to get cure.
When do women appear to be menopaused?
In general, a lot of women will appear menopause phenomenon when they are over 45 years old, then they enter menopause.
Can antibiotics cause urethritis?
And as antibiotics can bring damage to liver and kidney, it isn’t a good choice for postmenopausal women with urethritis. According to the medical report, TCM (traditional Chinese medicine) is accepted by more and more patients.
What hormone is responsible for maintaining elasticity in the vagina?
The hormone estrogen is partly responsible for maintaining elasticity in the vaginal and urethral tissues. Unfortunately, during menopause, what happens is the body begins to slow the circulation of estrogen. The result of which is a thinning out of the urogenital tissue. This then weakens the muscles that control the bladder and urinary functions.
Why does menopause cause urinary tract infections?
This is what causes bladder control and urinary problems during menopause that some women report. Low estrogen at menopause, combined with normal aging, may result in annoying symptoms of vaginal dryness, incontinence, and urinary tract infections.
What is the treatment for urogenital atrophy?
Hormone Therapy. As lack of estrogen is the primary cause of urogenital atrophy, the treatments for it in postmenopausal women involve low-dose hormone replacement therapy (HRT). These can help restore the vagina to premenopausal condition and relieve many symptoms of urogenital atrophy.
What to do if you have bladder problems during menopause?
If you’re having bladder control problems or other urinary problems during menopause, please feel comfortable speaking openly with your women’s health doctor, gynecologist about your concerns. Don’t neglect a doctor’s visit just because you assume you know the cause of the problem.
What is it called when your bladder is irritable?
Also known as irritable/overactive bladder, leakage that occurs when the bladder muscles squeeze seemingly at random or just all the time
What hormones do you stop making after your period?
After the end of your menstrual cycles, your body stops making the female hormone estrogen. In addition to controlling your monthly periods and the changes during pregnancy, estrogen also helps keep the lining of the bladder and the urethra healthy.
How to strengthen pelvic floor muscles?
Practice Kegel exercises. These are very easy exercises designed to strengthen your pelvic floor muscles. The basic idea is that you repetitively squeeze your pelvic muscles as though you were holding urine in. Ask your gynecologist for advice if you’re not sure where to begin.
What is AV in physiology?
Physiological and structural changes that occur within the vulvovaginal mucosa lead to the condition commonly called AV ( Table 1). 8 Subsequent to a marked postmenopausal decline in estrogen, or a loss of estrogen secondary to some treatments (e.g., oophorectomy, pelvic radiation, certain chemotherapy drugs), vaginal thinning occurs, increasing vulnerability to inflammation and infection. 9 A decline in estrogen alters the vaginal flora, which permits bacterial overgrowth, sometimes accompanied by vaginal discharge. 9 These changes are also responsible for dyspareunia, which has the potential to lead to a loss of sexual interest and activity. 10
What is the most common cause of incontinence in women who are in the reproductive years or early postmeno?
Stress Incontinence ( SI) is the most common cause of incontinence in women who are in the reproductive years or early postmenopausal years. 1 It is defined as urine leakage due to abrupt increases in intra-abdominal pressure on exertion, sneezing, coughing, laughing, bending, or lifting without the presence of detrusor activity. 1,12,13. ...
What is the cause of incontinence in geriatrics?
Overactive Bladder (OAB), caused by uninhibited detrusor muscle contractions, or detrusor overactivity, is the usual cause of incontinence in the geriatric population. 1 While most cases of OAB are idiopathic, neurologic conditions such as dementia, stroke, Parkinson’s disease, and multiple sclerosis amplify the condition. 11 Of note, a form of OAB with impaired contractility, characterized by urgency, frequency, a weak flow rate, and urinary retention, among other signs and symptoms, may mimic stress incontinence. 12
What information should a pharmacist have regarding AV?
Pharmacists should familiarize themselves with the necessary information regarding AV, atrophic urethritis, and the management of urogenital health in postmenopausal women. Providing information to patients about the condition and recommending nonpharmacologic and pharmacologic management interventions are imperative ( Table 2, Resources ).
Why does SI occur in obese people?
SI occurs largely because of complications of childbirth and the development of atrophic urethritis —thinning of the estrogen-dependent lining of the outer urethra. 5,12 Typically, it is more severe in obese people secondary to pressure from abdominal contents on the top of the bladder. 12 Cooper and Smith note that this type of incontinence is usually suffered in silence despite available treatment regimens. 1 Pharmacists have an opportunity to guide patients regarding these symptoms and the interventions available.
What are the symptoms of AV?
Diagnosis of AV is chiefly clinical, initiating with the determination of specific symptoms including vaginal dryness, burning, pruritus, abnormal discharge, and dyspareunia. 4,6 Symptoms may be more prominent in nonwhite women, those with diabetes, women who have a lower body mass index, and those who are younger at the time of menopause; more severe symptoms may appear in women who have not experienced a vaginal delivery. 4,6
What is sexual function?
According to Northrup, sexual function is a complex, integrated phenomenon, reflecting the health and balance of the following : 1) the ovaries; 2) the hormones; 3) the cardiovascular system; 4) the brain; 5) the spinal cord; and 6) the peripheral nerves. 5 For further reading, see Reference 5 under the chapter “Sex and Menopause: Myths and Reality,” which explores midlife changes in sexual function and sexuality, including comments on cultural inheritance and barriers. According to Cooper and Smith, since the expression of sexuality has no age limit, early and late postmenopausal women alike should be offered a full spectrum of counseling and treatment where appropriate. 1
What is the best treatment for vaginal atrophy?
The most common treatment for vaginal atrophy symptoms is low-dose vaginal estrogen replacement, utilizing creams, tablets or vaginal rings.
What are the symptoms of pelvic organ prolapse?
Vaginal bleeding. An increase in urinary tract infections due to a change in the acidity of the vagina. Urinary symptoms of pelvic organ prolapse are urge incontinence and painful urination.
What does it mean when you wake up at night to urinate?
Urge incontinence (irritable/overactive bladder): the sudden, strong urge to urinate, which can result in a loss of bladder control before one can reach a bathroom. Waking up several times during the night to urinate (nocturia). Symptoms related to vaginal atrophy are:
Why does estrogen affect menopause?
Reduced estrogen also alters the acidity of the vulva and the vagina, which can make the area more prone to infection by bacteria or yeast overgrowth. Menopausal urinary symptoms can also be caused by pelvic organ prolapse, in which one or more organs of the pelvic area drops down into the vagina. This can be due to stress from vaginal childbirth ...
What causes menopausal uroesis?
Causes of menopausal urinary symptoms. When menopause occurs, estrogen production is reduced, which is the major cause of urogenital atrophy. Atrophy means a wasting away of muscle mass, and urogenital atrophy involves atrophy of the vagina as well as atrophy of the urinary tract. The lack of estrogen weakens the bladder (which holds urine) ...
Why does menopause cause urinary problems?
These urinary changes occur for two reasons: Menopause reduces the amount of the female hormone estrogen, and a lack ...
What are some non-hormonal treatments for bladder control?
These include: Reducing caffeine.
Is Painful Urination a Symptom?
Painful urination during menopause can be a symptom of this stage, but it is not the same problem as a urinary tract infection. Painful urination can accompany the loss of bladder control and/or a feeling of constantly having to go without really having to. These problems can be explained by hormonal as well as physical changes in a woman’s body.
How to maintain bladder control?
Abstaining from alcohol and caffeine in excess and staying hydrated are important to more consistent functioning of the bladder. Strengthening the muscles of the pelvic floor is also beneficial to maintaining control and avoiding urinary incontinence and can be worked on with Kegel exercises.
Why do older women get urinary tract infections?
They happen more often in older women, because bacteria travels more easily to your bladder as the tissue of the urethra thins. The amount of bacteria in the genital area increases as well.
What is the term for a time of significant change for women?
2295. Menopause is a time of significant change for women. A result of this process can be painful urination related to differences in the bladder from when the body was younger. There are symptoms that can be uncomfortable yet a normal component of the process, but there can also be symptoms that are more serious and need to be addressed by ...
Why does the bladder lose its ability to process hormones?
This is because the pelvic muscle weakens and the lining of the urethra thins. Additionally, the bladder has large amounts of estrogen receptors that are losing their ability to process hormones.
What is the term for the loss of muscle mass in the vagina?
The atrophy , or loss of muscle mass, includes both the vagina and the urinary track, and is responsible for the organ’s inability to hold itself in place. This can also reflect damage to the muscles of the pelvic floor.
How long does it take for a urinary tract infection to increase?
The risk of this begins to increase around five years after your final period.
What is the duct through which urine exits your body?
Your urethra is the duct through which urine exits your body. They are mostly found in. Trusted Source. women who have been through the menopause. A urethral caruncle is the most common benign tumor that occurs in the urethra in postmenopausal women.
Why do women have urethral caruncles?
Estrogen naturally keeps your genital area skin flexible and lush. If your levels drop, your skin may dry, thin down, tear easily, and become prone to other irritation. This may be why urethral caruncles are most common in women who have gone through menopause.
What is the best treatment for a swollen thigh?
A typical treatment plan may include topical estrogen cream to help restore your levels and a topical anti-inflammatory medication to further ease symptoms.
What to do if you have pain after surgery?
If you find that you’re experiencing pain or bleeding, make an appointment to see your doctor. They can prescribe medication to ease or even eliminate your symptoms. If you’re symptoms worsen after treatment, surgical removal may be necessary. Last medically reviewed on December 18, 2017.
How long does it take to recover from a cystectomy?
The procedure typically takes up to an hour to complete and around two weeks to recover from.
Can a urethral caruncle cause pain?
A urethral caruncle typically won’t cause any symptoms. Most people don’t even know it’s there until their doctor points it out during a routine examination. However, pain and bleeding are possible. For example, some women report a burning pain when they urinate.
Can a caruncle grow around the urethra?
However, cases have been reported where they’ve have grown at least 2 cm in diameter. They typically sit on one side of the urethra (the posterior edge), and don’t go around the whole circle of the opening. A urethral caruncle typically won’t cause any symptoms.
Causes
Diagnosis
- Diagnosis of urethritis starts with a careful medical history. Your healthcare provider will ask you about any possible risk factors for STIs, such as a new sexual partner or condomless sex. They will also ask about any urological problems you have had in the past. Your doctor will then perform a physical exam. They will pay special attention to the presence of urethral discharge, ul…
Complications
- Some complications may occur with the common causes of urethral pain. These complications make a proper diagnosis essential. Complications include: 1. Pelvic inflammatory disease (PID): Untreated STIs such as chlamydia can lead to pelvic inflammatory disease, one of the leading causes of infertility.12 2. Pregnancy complications: When pregnancy does occur, there is an incr…
Prevention
- Fortunately, there are simple measures you can take to prevent the more common causes of urethral pain. Safer sex practicescan help reduce your risk of STIs. You can make sex safer by: 1. Always using an external condom and other barriers 2. Limiting the number of sexual partners you have 3. Getting tested for STIs regularly Tips for reducing the risk of urinary tract infections inclu…
When to See A Healthcare Provider
- It is never normal to have pain in the urethra. So a healthcare provider should always evaluate this symptom unless it has a clear, reversible cause, such as stinging immediately after using a new personal care product. That said, some conditions are more urgent than others. Untreated infections with chlamydia and gonorrhea can permanently damage reproductive organs. Even in …
Summary
- Urethral pain may be caused by many things, including STIs, trauma, bacterial or fungal infections, and obstruction. To accurately diagnose what is causing pain in your urethra, your doctor will do a physical exam. They may also order labs and imaging tests. Treatment depends on the cause and may include antibiotics, antiparasitics, antivirals, or symptom management. Urethra pain is neve…
A Word from Verywell
- Because a sexually transmitted infection may be one cause of urethral pain, people are sometimes hesitant to talk to their healthcare provider about it. However, STIs are common and nothing that should cause embarrassment. Additionally, there are many potential causes of urethral pain. Pain, in general, is your body's way of letting you know that something is wrong. In …
Symptoms
Diagnosis
- The presence of a circular or donut-shaped bulge protruding from the external opening of the urethra indicates a likely urethral prolapse. Release of urine from the central opening within the mass, either by natural voiding or catheterization, confirms the diagnosis.1 In adults, the cystourethroscopy (inserting a tube with an attached camera into the urethra) is sometimes use…
Causes
- The causes of urethral prolapse are not fully understood. Activities or life events like lifting heavy objects or childbirth may raise the risk for prolapse because they increase abdominal pressure. This can weaken or strain the pelvic muscles and supporting tissue.
Complications
- The most severe complication is strangulatedurethral prolapse. Strangulated urethral prolapse occurs when the prolapse tissue obstructs blood flow. The blocked flow of blood causes clotting and prevents the normal return of blood from the tissue. The protruding tissue begins to die and turns a bluish or purplish color.6 Strangulated urethral prolapse can cause severe pain upon urin…
Treatment
- Many cases of urethral prolapse are mild and go away with minimal or no treatment. More severe cases, such as those involving strangulated urethral prolapse, may require surgery.
A Word from Verywell
- Many cases of urethral prolapse cause no symptoms. If you notice tissue protruding from the urethral opening, be sure to bring it up to your healthcare provider. Prompt treatment can prevent infections and other complications and help you avoid surgery.