Medication
The abdominal organs, such as the stomach and liver, are wrapped in a thin, tough membrane called the visceral peritoneum. How long does it take for peritonitis to heal? If you’re diagnosed with peritonitis, you’ll need treatment in hospital to get rid of the infection. This might take 10 to 14 days.
Procedures
hard to treat b/c there is no blood supply. Why does peritonitis have a wide range effect on abdominal organs? b/c it surrounds multiple organs.
Nutrition
Urgent advice: Get advice from 111 now if you have:
- sudden tummy pain that gets worse when touched or when you move
- a very high temperature (you feel hot and shivery)
- a rapid heartbeat (your heart is beating more quickly than normal)
- not been able to pee or are peeing much less than normal
See more
The potential complications of secondary peritonitis include:
- an intra-abdominal abscess
- gangrenous bowel, which is dead bowel tissue
- intraperitoneal adhesions, which are bands of fibrous tissue that join abdominal organs and can cause bowel blockage
- septic shock, which is characterized by dangerously low blood pressure
How long does it take to heal from peritonitis?
Why is peritonitis difficult to treat?
Why is peritonitis life threatening?
What is the danger of peritonitis?

How long does it take to recover from peritonitis?
If you're diagnosed with peritonitis, you'll need treatment in hospital to get rid of the infection. This might take 10 to 14 days. Treatment usually involves being given antibiotics into a vein (intravenously).
What is the most common cause of peritonitis?
The most common risk factors for primary spontaneous peritonitis include: Liver disease with cirrhosis. Such disease often causes a buildup of abdominal fluid (ascites) that can become infected. Kidney failure getting peritoneal dialysis.
What is one of the first signs of peritonitis?
What are symptoms of peritonitis?Severe belly pain that gets worse with any motion.Nausea and vomiting.Fever.Sore or swollen belly.Fluid in the belly.Not being able to have a bowel movement or pass gas.Less urine than normal.Thirst.More items...
Can you treat peritonitis with antibiotics?
Commonly used antibiotics for the treatment of peritonitis include beta-lactams (penicillins), carbapenems (beta-lactamase−resistant beta-lactams), cephalosporins (semi-synthetic beta-lactams), and quinolones (such as ciprofloxacin).
Is peritonitis an emergency?
Peritonitis requires prompt medical attention to fight the infection and, if necessary, to treat any underlying medical conditions. Peritonitis treatment usually involves antibiotics and, in some cases, surgery. Left untreated, peritonitis can lead to severe, potentially life-threatening infection throughout your body.
How many stages of peritonitis are there?
Peritonitis is divided into three stages. The division is based on the defensive and inhibitory mechanisms of the host.
What are three causes of peritonitis?
What causes peritonitis?an abdominal wound, such as a surgical wound.an abdominal injury.a ruptured appendix.a stomach ulcer.a perforated colon.diverticulitis.pancreatitis.liver disease, such as cirrhosis of the liver.More items...
What is the most common complication of peritonitis?
Aggressive fluid resuscitation and early surgical intervention are the mainstay of therapy of peritonitis. Enterocutaneous fistulas, surgical site infection, sepsis, and multiorgan failure are the commonest complications seen in surgical settings.
Can peritonitis be seen on CT scan?
Inflammatory and malignant diseases of the peritoneum can have a similar appearance. Moreover, different causes of peritonitis can show similar CT findings. Therefore, a CT pattern-approach may represent a further useful diagnostic tool for correct image assessment.
How do you confirm peritonitis?
To diagnose peritonitis, your doctor will talk with you about your medical history and perform a physical exam. When peritonitis is associated with peritoneal dialysis, your signs and symptoms, particularly cloudy dialysis fluid, may be enough for your doctor to diagnose the condition.
What is the best antibiotic for peritonitis?
Cefotaxime is effective against 98% of causative organisms and is considered the treatment drug of choice. Anaerobic, pseudomonal, and staphylococcal coverage is not needed. Cefotaxime (2 g IV q8h) has been shown to achieve excellent ascitic fluid levels.
Which symptom is often observed in cases of peritonitis?
The diagnosis of peritonitis is a clinical diagnosis, based mostly on history and physical examination. The main symptom in all cases is abdominal pain. The pain can be sharp or insidious; often the pain is constant and intense, and is aggravated with movement.
Why is it important to treat peritonitis?
It is important to treat peritonitis quickly to prevent any infection from spreading to other parts of the body.
How to treat acute infectious peritonitis?
Treatment for peritonitis typically starts with antibiotics to get rid of the infection.
What causes peritonitis in the peritoneum?
Infectious agents including, but not limited to, bacteria and fungi causes peritonitis. Sometimes the infection begins in the peritoneum. More often, the infection spreads from another area of the body. Some of the most common reasons infection could spread to the peritoneum include: Burst appendix. Stomach ulcer.
Why is it important to diagnose peritonitis early?
Early diagnosis is very important for anyone with peritonitis to receive effective treatment .
How to diagnose peritonitis?
To diagnose peritonitis, your doctor will do a physical exam to check if your abdomen is tender and if it feels firm or soft. Blood tests and other tests that provide images of the inside of your abdomen may also be used to determine the cause of the problem. These may include a CT scan or ultrasound.
What is the term for inflammation of the peritoneum?
The peritoneum is the thin tissue that lines the inside of your abdomen (belly) and covers the abdominal organs. Peritonitis is the term for inflammation of the peritoneum. Usually, an infection causes peritonitis. An injury or certain diseases also can cause it.
How to diagnose peritonitis?
Diagnostic tests for peritonitis may include: 1 Blood and urine tests 2 Imaging studies such as X-rays and computerized tomography (CT) scans 3 Exploratory surgery
What are the symptoms of peritonitis?
Symptoms of Peritonitis. The first symptoms of peritonitis are typically poor appetite and nausea and a dull abdominal ache that quickly turns into persistent, severe abdominal pain, which is worsened by any movement. Other signs and symptoms related to peritonitis may include:
Why do people with kidney failure need peritoneal dialysis?
It's linked to a higher risk of peritonitis due to accidental contamination of the peritoneum by way of the catheter .
What to do if you have peritoneal dialysis?
Seeking prompt medical attention is especially important for peritoneal dialysis patients who have a combination of abdominal pain and a clouding of the peritoneal fluid , which is caused by a buildup of infection-fighting white blood cells.
What causes peritonitis in the abdomen?
Trauma to the abdomen, such as an injury from a knife or gunshot wound. Noninfectious causes of peritonitis include irritants such as bile, blood, or foreign substances in the abdomen, such as barium.
How to prevent infection from dialysis?
Immediately report any possible contamination of your dialysis fluid or catheter to your peritoneal dialysis nurse. In many cases, a single dose of antibiotics can prevent a contamination from turning into an infection.
What is the inflammation of the peritoneum?
Peritonitis is an inflammation of the peritoneum, the tissue that lines the inner wall of the abdomen and covers and supports most of your abdominal organs. Peritonitis is usually caused by infection from bacteria or fungi.
What is the cause of peritonitis?
There are two types of peritonitis. Spontaneous bacterial peritonitis (SBP) is the result of an infection of the fluid in your peritoneal cavity. Kidney or liver failure can cause this condition. People on peritoneal dialysis for kidney failure are also at increased risk for SBP.
What are the complications of peritonitis?
The potential complications of spontaneous peritonitis include: hepatic encephalopathy, which is a loss of brain function that occurs when the liver can no longer remove toxic substances from your blood. hepatorenal syndrome, which is progressive kidney failure.
What is the peritoneum?
Peritonitis is inflammation of the peritoneum, the thin layer of tissue covering the inside of your abdomen and most of its organs. The inflammation is usually the result of a fungal or bacterial infection. This can be caused by an abdominal injury, an underlying medical condition, or a treatment device, such as a dialysis catheter or feeding tube.
How do you know if you have peritonitis?
Common symptoms of peritonitis include: tenderness in your abdomen. pain in your abdomen that gets more intense with motion or touch. abdominal bloating or distention. nausea and vomiting. diarrhea.
What test can be used to diagnose peritonitis?
Several other tests can help your doctor diagnose peritonitis: A blood test, called a complete blood count (CBC), can measure your white blood cell count (WBC). A high WBC count usually signals inflammation or infection. A blood culture can help to identify the bacteria causing the infection or inflammation.
What causes secondary peritonitis?
Secondary peritonitis is usually due to an infection that has spread from your digestive tract. The following conditions can lead to peritonitis: invasive medical procedures, including treatment for kidney failure, surgery, or the use of a feeding tube.
What is the term for a perforated colon?
a perforated colon. diverticulitis. pancreatitis, or inflammation of the pancreas. cirrhosis of the liver or other types of liver disease. infection of the gallbladder, intestines, or bloodstream. pelvic inflammatory disease (PID) Crohn’s disease.
How to know if you have peritonitis?
Your healthcare provider will look at your past health. He or she will give you a physical exam. Peritonitis is often diagnosed by analyzing a sample of the infected fluid taken from the belly (abdomen).
What tests are done to find out what is causing the infection?
Blood, fluid, and urine tests. These tests are done to find out what is causing the infection. CT scans (computed tomography scans). These imaging tests use X-rays and computer technology to make pictures of the body. CT scans show detailed images of any part of the body. This includes bones, muscles, fat, and organs.
Can peritonitis cause dehydration?
Peritonitis can cause severe health problems. It can be deadly if not treated right away. Peritonitis can make fluid fill up in your belly or abdomen. This can cause severe fluid loss or dehydration. If peritonitis isn’t treated the infection can quickly spread through your body.
What is the treatment for peritonitis?
Peritonitis treatment usually involves antibiotics and, in some cases, surgery. Left untreated, peritonitis can lead to severe, potentially life-threatening infection throughout your body.
What causes peritonitis in the liver?
Injury or trauma may cause peritonitis by allowing bacteria or chemicals from other parts of your body to enter the peritoneum. Peritonitis that develops without an abdominal rupture (spontaneous bacterial peritonitis) is usually a complication of liver disease, such as cirrhosis.
Why does peritoneal dialysis cause infection?
An infection may occur during peritoneal dialysis due to unclean surroundings, poor hygiene or contaminated equipment.
What causes bacteria to enter the peritoneum?
Any of these conditions can allow bacteria to get into the peritoneum through a hole in your gastrointestinal tract. Pancreatitis. Inflammation of your pancreas (pancreatitis) complicated by infection may lead to peritonitis if the bacteria spreads outside the pancreas. Diverticulitis.
Why does my peritoneum smell?
Peritonitis may result from a burst appendix or trauma-related abdominal injury. Seek immediate medical attention if you develop abdominal pain so severe that you're unable to sit still or find a comfortable position.
Can peritonitis cause organ failure?
Left untreated, peritonitis can extend beyond your peritoneum, where it may cause: An infection throughout your body (sepsis). Sepsis is a rapidly progressing, life-threatening condition that can cause shock, organ failure and death.
Can peritoneal infection occur without rupture?
In most cases, the cause is a rupture (perforation) within the abdominal wall. Though it's rare, the condition can develop without an abdominal rupture.
What is the treatment for peritonitis?
In general, intravenous antibiotics or antifungal medications are administered, as soon as possible, in order to treat the patients having this infection.
Why does peritonitis spread?
Such a condition may be caused due to bacterial or fungal infection. In addition to this, abdominal injury, other underlying medical condition or a treatment device (for example, a dialysis catheter or feeding tube) may also result in such a condition. If left untreated, peritonitis can quickly spread into the blood stream ...
What is the peritoneum?
Peritoneum is the thin layer of tissue which covers the inside of the abdomen and also other abdominal organs. Peritonitis refers to a condition which is characterised by inflammation of the peritoneum. Such a condition may be caused due to bacterial or fungal infection. In addition to this, abdominal injury, other underlying medical condition ...
What are the post treatment guidelines?
The post treatment guidelines include taking the prescribed medicines regularly on time, as instructed by the physician. The patient must consult his/her doctor, in case the medicines do not prove to be effective or if the patient is having side effects from such medications.
Is peritonitis a life threatening condition?
Peritonitis can be life threatening and hence requires immediate treatment in order to avoid further complications which may prove fatal. Diagnosis of this condition includes testing of blood and urine samples, imaging studies such as computerized tomography (CT) scans and exploratory surgery.
Can you recover from peritonitis?
However, patients who have been diagnosed as having peritonitis at a later stage or is having further complications may require a longer time for their recovery. Proper medication and care is highly recommended during the course of treatment for early and effective recovery.
Can you be admitted to the hospital for peritonitis?
A person diagnosed as having peritonitis, needs to be immediately admitted to the hospital for medical treatment. Additional supportive treatments may also be deemed necessary if the patient suffers from organ failure due to sepsis which develops as a later complication of this problem.
What is the management approach for peritoneal abscesses?
The management approach to peritonitis and peritoneal abscesses targets correction of the underlying process, administration of systemic antibiotics, and supportive therapy to prevent or limit secondary complications due to organ system failure. Treatment success is defined as adequate source control with resolution of sepsis and clearance of all residual intra-abdominal infection.
How long does it take to repeat paracentesis?
If the course is atypical, repeat paracentesis should be performed in 48 hours. For SBP, a 10-day to 14-day course of antibiotics is recommended. Although not required, a repeat peritoneal fluid analysis is recommended to verify declining polymorphonuclear neutrophil (PMN) counts and sterilization of ascitic fluid.
How long does it take for an ascitic fluid to improve?
If improvement in ascitic fluid or clinical condition does not occur within 48 hours, further evaluation is required to rule out bowel perforation or intra-abdominal abscess. Evaluation may include a combination of radiography, computed tomography scanning, intraluminal contrast studies, or surgical exploration.
What factors can prevent successful source control with percutaneous drainage?
Factors that may prevent successful source control with percutaneous drainage include diffuse peritonitis, lack of localization of the infectious process, multiple abscesses, anatomic inaccessibility, or the need for surgical debridement. [ 5]
What is systemic antibiotic therapy?
Systemic antibiotic therapy. Intensive care with hemodynamic, pulmonary, and renal support. Nutrition and metabolic support. Inflammatory response modulation therapy. Early control of the septic source is mandatory and can be achieved by operative and nonoperative means.
What are the principles of infection?
The general principles guiding the treatment of infections are four-fold, as follows [ 1, 16] : 1 Control the infectious source 2 Eliminate bacteria and toxins 3 Maintain organ system function 4 Control the inflammatory process
Does peritonitis develop after exploration?
In general, patients with peritonitis develop some degree of gut dysfunction (eg, ileus) after exploration. Consider establishing some form of nutritional support early in the course of treatment because most patients have an insufficient enteral intake for a variable amount of time preoperatively.
What is the best treatment for peritonitis?
Oxygen therapy. Oxygen therapy by nasal cannula or mask generally promotes adequate oxygenation. Antibiotic therapy. Antibiotic therapy is initiated early in the treatment of peritonitis.
What is the pathophysiology of peritonitis?
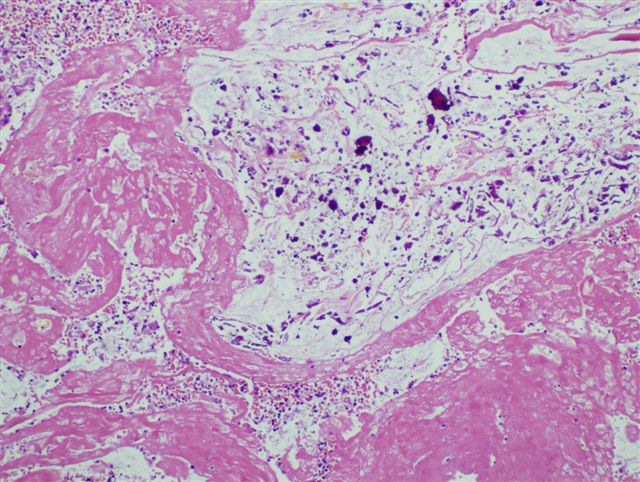
The pathophysiology of peritonitis involves: Leakage. Peritonitis is caused by leakage of contents from abdominal organs into the abdominal cavity. Proliferation. Bacterial proliferation occurs. Edema. Edema of the tissues occurs, and exudation of fluid develops in a short time. Invasion.
What is the peritoneum of diverticulitis?
Peritonitis is the inflammation of the peritoneum, the serous membrane lining the abdominal cavity and covering the viscera.
What causes peritonitis in the kidneys?
Inflammation. An inflammation that extends from an organ outside the peritoneal area such as the kidne ys could cause peritonitis. Bacteria. The most common bacteria implicated are Escherichia coli, Klebsiella, Proteus, Pseudomonas, and Streptococcus.
What is the major cause of death from peritonitis?
Sepsis. Sepsis is the major cause of death from peritonitis. Shock. Shock may result from septicemia or hypovolemia. Intestinal obstruction. The inflammatory process may cause intestinal obstruction, primarily from the development of bowel adhesions.
What is the immediate response of the intestinal tract?
Response. The immediate response of the intestinal tract is hypermotility, soon followed by paralytic ileus with an accumulation of air and fluid in the bowel.
What are the causes of pericoronitis?
What are the causes and risk factors of pericoronitis? Pericoronitis usually occurs when a molar is partially impacted. Bacteria then accumulates around the soft tissue, causing inflammation. The following factors can increase your risk of pericoronitis: age between 20 to 29. wisdom teeth that haven’t properly erupted.
How long does it take for pericoronitis to heal after a tooth removal?
Once a tooth has been removed, pericoronitis rarely returns. In cases where a flap of gum tissue is removed, the tissue can sometimes grow back. People usually recover from treatment in about two weeks’ time after a removal, and within one or two days for symptom-specific treatment for acute pericoronitis.
What is the best way to treat a tooth infection?
Your dentist will also clean the gum tissue around your tooth to prevent buildup of plaque and food particles. They may use local anesthesia to help with the pain during this process. If you experience swelling or infection, you may be prescribed antibiotics like penicillin or erythromycin (Erythrocin Stearate).
What to do if your tooth is erupting on its own?
Managing pain. If the tooth is expected to fully erupt on its own, your dentist may decide to help you manage the symptoms without removing the flap or the tooth. In this case, ibuprofen (Advil) or acetaminophen (Tylenol) can be helpful.
How do you know if you have pericoronitis?
The symptoms of acute pericoronitis include: severe pain near your back teeth. swelling of gum tissue. pain when swallowing. the discharge of pus. trismus (lockjaw) Chronic pericoronitis can include the following symptoms: bad breath. a bad taste in your mouth.
Can you have a flap removed from a pericoronitis?
Most people with pericoronitis have a flap of gum tissue partially covering the crown of the erupting tooth. Your doctor may recommend having the flap removed or extracting the tooth, based on a number of factors. Sometimes, only treating the actual symptoms is the best course of action.
Can pericoronitis spread to other areas?
In some cases, infection can spread from the affected tooth to other areas of your mouth. While rare, a person experiencing pericoronitis can develop a life-threatening complication called Ludwig’s angina, in which the infection spreads into their head and neck.
