
Medication
- Drink plenty of water.
- Eat plenty of vegetables and fruits.
- Maintain bowel regularity through high fiber intake.
- Eat probiotic foods (yogurt, sauerkraut, tempeh, etc.)
Procedures
Other examples of high-fat foods to avoid, include:
- dairy products
- processed meats, such as hot dogs and sausage
- mayonnaise
- potato chips
Therapy
- Eating an alkalized, healing diet
- Drinking healing mineral water
- Using acupuncture
- Taking herbs
- Having chiropractor manipulations and abdominal massage
- Taking nutritional supplements
- Participating in medical hypnosis, meditation, relaxation techniques
Nutrition
- Drink plenty of water
- Stop or reduce alcohol consumption
- Stop smoking, because the habit increases your risk of pancreatitis
- Refrain from eating foods high in fat
What foods should you eat while recovering from pancreatitis?
What foods can you not eat with pancreatitis?
How do you heal pancreatitis naturally?
What is the best remedy for pancreatitis?

What is the fastest way to cure pancreatitis?
Adopt a liquid diet consisting of foods such as broth, gelatin, and soups. These simple foods may allow the inflammation process to get better. Over-the-counter pain medications may also help. Avoid pain medications that can affect the liver such as acetaminophen (Tylenol and others).
How long can it take to recover from pancreatitis?
People with mild acute pancreatitis usually start to get better within a week and experience either no further problems, or problems that get better within 48 hours. Many people are well enough to leave hospital after a few days.
Does pancreatitis go away?
A:If acute pancreatitis is mild, it may go away on its own without treatment. But in more serious cases, treatments for both acute and chronic pancreatitis can include IV fluids, medications, and possibly surgery depending on the cause of the pancreatic inflammation.
What causes pancreatitis?
Pancreatitis is the redness and swelling (inflammation) of the pancreas. It may be sudden (acute) or ongoing (chronic). The most common causes are alcohol abuse and lumps of solid material (gallstones) in the gallbladder. The goal for treatment is to rest the pancreas and let it heal.
What are the warning signs of pancreatitis?
SymptomsUpper abdominal pain.Abdominal pain that radiates to your back.Tenderness when touching the abdomen.Fever.Rapid pulse.Nausea.Vomiting.
What foods irritate the pancreas?
There are a few things you must completely avoid, such as alcohol and fried/greasy/high fat foods (such as creamy sauces, fast food, full fat meat and dairy, and anything fried). These foods can cause your pancreas to release more enzymes at once than it normally would, leading to an attack.
What happens if pancreatitis is left untreated?
If left untreated, pancreatitis can cause kidney failure, trouble breathing, digestion issues, diabetes, and abdominal pain.
How can I treat pancreatic pain at home?
How can you care for yourself at home?Drink clear liquids and eat bland foods until you feel better. ... Eat a low-fat diet until your doctor says your pancreas is healed.Do not drink alcohol. ... Be safe with medicines. ... If your doctor prescribed antibiotics, take them as directed. ... Get extra rest until you feel better.
What is the best antibiotic for pancreatitis?
The best option for the treatment is Imipenem 3 × 500 mg/day i.v. for 14 days. Alternatively, Ciprofloxacin 2 × 400 mg/day i.v. associated with Metronidazole 3 × 500 mg for 14 days can also be considered as an option.
Can pancreatitis be caused by stress?
Summarizing this topic, chronic stress appears as a risk factor to develop pancreatitis by sensitizing the exocrine pancreas through TNF-α, which seems to exert its detrimental effects through different pathways (Figure 2).
Can you live without your pancreas?
It's possible to live without a pancreas. But when the entire pancreas is removed, people are left without the cells that make insulin and other hormones that help maintain safe blood sugar levels. These people develop diabetes, which can be hard to manage because they are totally dependent on insulin shots.
How do you treat pancreatitis naturally?
Omega-3 Fatty Acids These are nutrients you can get by eating salmon, tuna, and flaxseeds. Some small studies have shown that omega-3 fatty acids may reduce inflammation from pancreatitis and repair damaged tissue. Researchers reviewed eight clinical trials involving 364 participants with severe acute pancreatitis.
How Is Acute Pancreatitis Treated?
Cases of moderate and severe acute pancreatitis are treated in the hospital. Visits should only last a few days. Doctors will administer blood and...
How Is Chronic Pancreatitis Treated?
There is no cure for chronic pancreatitis, but the related pain and symptoms may be managed or even prevented. Since chronic pancreatitis is most o...
How Is Severe Pancreatitis Treated?
About 20 percent of pancreatitis cases are severe, meaning they result in multiple organ failure that doesn't naturally subside within 48 hours. (3...
How Are Pancreatitis Complications Treated?
Antibiotics may also be necessary if an extra-pancreatic (outside of the pancreas) infection has developed.Up to one-third of people with pancreati...
How Do You Manage Pancreatitis at Home?
In addition to hospital treatment, the following lifestyle changes are recommended to help aid recovery and possibly prevent pancreatitis: 1. Drink...
What Is A Pancreatic Diet?
There is no one specific pancreatic diet that can treat chronic pancreatitis.But there are some general rules for nutrition if you have the conditi...
How do you treat pancreatitis?
How do health care professionals treat pancreatitis? 1 a hospital stay to treat dehydration with intravenous (IV) fluids and, if you can swallow them, fluids by mouth 2 pain medicine, and antibiotics by mouth or through an IV if you have an infection in your pancreas 3 a low-fat diet, or nutrition by feeding tube or IV if you can’t eat
What to do if you have a blockage in your pancreas?
If you have stones blocking your pancreatic duct, your doctor may use a procedure to break up and remove the stones. Treatment for acute or chronic pancreatitis may include a hospital stay to treat dehydration and prescribe pain medicine, antibiotics, and nutrition.
What is ERCP in gastroenterology?
Doctors use ERCP to treat both acute and chronic pancreatitis. ERCP combines upper gastrointestinal endoscopy and x-rays to treat narrowing or blockage of a bile or pancreatic duct. Your gastroenterologist may use ERCP to remove gallstones blocking the bile or pancreatic ducts.
How long does it take for pancreatitis to go away?
Mild acute pancreatitis usually goes away in a few days with rest and treatment. If your pancreatitis is more severe, your treatment may also include: Surgery. Your doctor may recommend surgery to remove the gallbladder, called cholecystectomy, if gallstones cause your pancreatitis.
What can a doctor prescribe for diabetes?
Your doctor may prescribe or provide the following: Medicines and vitamins. Your doctor may give you enzyme pills to help with digestion, or vitamins. NIH external link. A, D, E, and K if you have malabsorption. He or she may also give you vitamin B-12. NIH external link. shots if you need them. Treatment for diabetes.
What is the treatment for dehydration?
a hospital stay to treat dehydration with intravenous (IV) fluids and, if you can swallow them, fluids by mouth. pain medicine, and antibiotics by mouth or through an IV if you have an infection in your pancreas. Your doctor may send you to a gastroenterologist or surgeon for one of the following treatments, depending on the type ...
Where is the surgery done for pancreatitis?
Surgery is done in a hospital, where you may have to stay a few days. In patients who do not get better with other treatments, surgeons may perform surgery to remove your whole pancreas, followed by islet auto-transplantation. Islets are groups of cells in your pancreas that make hormones, including insulin.
How to treat pancreatitis in the hospital?
In addition to hospital treatment, the following lifestyle changes are recommended to help aid recovery and possibly prevent pancreatitis: 1 Drink plenty of water 2 Stop or reduce alcohol consumption 3 Stop smoking, because the habit increases your risk of pancreatitis 4 Refrain from eating foods high in fat
How to help pancreatitis?
In addition to hospital treatment, the following lifestyle changes are recommended to help aid recovery and possibly prevent pancreatitis: Drink plenty of water. Stop or reduce alcohol consumption. Stop smoking, because the habit increases your risk of pancreatitis. Refrain from eating foods high in fat.
Why does my pancreas hurt?
It's long been thought that an inflamed head of the pancreas or a blocked pancreatic duct causes the pain. In cases where doctors believe that to be the problem, surgery will be performed to remove the head of the pancreas.
How long does a pancreatitis visit last?
Cases of moderate and severe acute pancreatitis are treated in the hospital. Visits should only last a few days. Doctors will administer blood and imaging tests to diagnose you, and then begin care. Because of the loss of fluids from vomiting and decreased food intake, the initial treatment for pancreatitis is hydration using intravenous (IV) ...
What is the procedure called when the pancreas is removed?
During this procedure, known as autologous islet cell transplantation, the entire pancreas is removed and the insulin-making cells of the pancreas are reinserted into the liver with a catheter. When the transplant is successful, it allows patients to make insulin without the pancreas.
What is the most common symptom of pancreatitis?
There are varying severities of the condition, but abdominal pain, nausea, and vomiting are among the most common symptoms of both acute and chronic pancreatitis.
Can pancreatitis be treated in intensive care?
People with severe pancreatitis may need to be transferred to an intensive care unit for an extended treatment, which could last more than a week. Due to vomiting, sweating, and reduced consumption of food and liquids, severe pancreatitis frequently causes hypovolemia — a decreased volume of blood circulating in the body.
How to treat pancreatitis?
Doctors use one or more of these methods to treat acute pancreatitis: Hospitalization with supportive care and monitoring. Pain medication to provide comfort. Endoscopic procedure or surgery to remove a gallstone, other blockage or damaged part of the pancreas.
What blood test is used to determine if you have acute pancreatitis?
For acute pancreatitis, your provider may order a blood test that measures the levels of two digestive enzymes (amylase and lipase) produced by the pancreas. High levels of these enzymes indicate acute pancreatitis.
Why does my pancreas swell?
Pancreatitis. Pancreatitis happens when your pancreas becomes irritated and inflamed (swollen). It’s not a common condition. There are multiple causes, but the main culprits are gallstones or heavy alcohol use. The condition can flare up suddenly or be a long-lasting problem, which can lead to permanent damage.
What is the term for inflammation of the pancreas?
What is pancreatitis ? Pancreatitis is an inflammation (swelling) of the pancreas. When the pancreas is inflamed, the powerful digestive enzymes it makes can damage its tissue. The inflamed pancreas can cause release of inflammatory cells and toxins that may harm your lungs, kidneys and heart.
What is the function of the pancreas?
First, it makes digestive enzymes (chemicals) and releases them into the small intestine. These enzymes break down carbohydrates, proteins and fat from food. Your pancreas also produces several hormones and releases them into the blood.
What is laparoscopic surgery?
During laparoscopic surgery, your surgeon inserts a laparoscope (an instrument with a tiny camera and light) into keyhole-sized cuts in your abdomen.
Does pancreatitis go away?
While chronic pancreatitis doesn’t go away, you can manage the symptoms and avoid complications with help from your doctor.
What are the immediate treatments for pancreatitis?
Support wikiHow by unlocking this expert answer. If you have chronic pancreatitis, immediate treatments might include hospitalization and aggressive hydration. If you have complications, like an infection, you might need antibiotics.
How to prevent pancreatitis?
Eat healthy and exercise. If you have only a mild case of pancreatitis, you may want to take some precautions so that you don't get pancreatitis again in the future. One of the best things that you can do is to eat healthy and exercise. Pancreatitis can develop due to high triglycerides or diabetes.
What is the name of the condition that causes nausea, vomiting, fever, sweating, and abdominal pain?
Pancreatitis occurs when the pancreas is inflamed, which results in malabsorption of nutrients. It can come on suddenly or become chronic, which may cause long-term damage to the pancreas. Symptoms include nausea, vomiting, fever, sweating, rapid breathing and abdominal pain.
What tests are done to determine if you have pancreatitis?
Blood tests, stool tests, CT scans, and ultrasounds are the most common tests to find out the source of your health problems when pancreatitis is suspected. [7] Receive basic treatment. For 75% of patients, basic hospital care will be all that is needed to recover.
Why is it important to recognize pancreatitis symptoms?
It's important to recognize the symptoms of pancreatitis, so that you can seek help sooner. The sooner the problem is dealt with, the easier it will be to solve. If you have any of the following symptoms that persist for several days or that cause you serious discomfort, call your doctor:
What painkillers are prescribed for pancreatitis?
Meperidine or Demerol are the most commonly prescribed painkillers for patients with pancreatitis. Take antibiotics should your doctor prescribe them. They may be given to prevent possible infection or to treat an existing one.
Can pancreatitis be serious?
You may not have pancreatitis, but instead have some other problem. However, these problems can still be very serious, so it's important to still seek treatment.
Chronic Pancreatitis Treatment: Medication
For patients with chronic pain that cannot be controlled otherwise, we may recommend medication.
Chronic Pancreatitis Treatment: Surgery
When medical and endoscopic therapies have failed, we may recommend surgery. There are many surgical options. Different procedures work better for different patients. We will work closely with you to find the surgical approach that offers you the best outcome.
Chronic Pancreatitis Treatment: Celiac Nerve Block
In the advanced stages of chronic pancreatitis, oral drugs may not be enough to control the pain. Your doctor may recommend a nerve block, which is an injection of an anesthetic around your nerve. The injection stops the nerves from sending pain messages.
Chronic Pancreatitis Treatment: Endoscopic Therapy
Your doctor may be able to treat chronic pancreatitis using endoscopic procedures.
Chronic Pancreatitis: Treating Complications
Chronic pancreatitis can cause complications in other parts of the body. Part of treating the disease is to treat and manage those complications. Depending on the complication and the severity, we can treat it endoscopically, surgically or using percutaneous therapy.
Endoscopic Therapy
Endoscopic therapy helps treat three specific areas of acute pancreatitis:
Acute Pancreatitis Treatment: Surgery
Resecting (removing) the diseased pancreatic tissue, depending on the severity of your condition.
Acute Pancreatitis: Complications
In patients with severe pancreatitis, complications may develop that affect other organs in the body. These systemic problems can involve the pulmonary system, kidneys, stomach and colon. Severe pancreatitis can also cause local complications, including:
How to treat pancreatitis pain?
Acute pancreatitis is usually very painful. There are a number of medications to relieve the pain. Strong painkillers (opioids) are often needed. Painkillers are also usually given through a drip or catheter(epidural). Sometimes it’s possible to adjust the dose of the painkiller on your own.
Why do we take antibiotics for pancreatitis?
This was done to keep the dead tissue from becoming infected and causing a condition called infected pancreatic necrosis.
What is the most common complication of pancreatitis?
Severe cases of pancreatitis. In about 15 to 20 out of 100 cases, acute pancreatitis leads to complications affecting the pancreas or other organs. Pseudocysts (fluid-filled cyst-like blisters in the pancreas) are a common complication. If they are small and don’t cause any symptoms, they don’t need to be treated.
How long does it take for pancreatitis to clear up?
Acute pancreatitis usually clears up within one to two weeks. Solid foods are generally avoided for a while in order to reduce the strain on the pancreas. Supportive measures like an infusion (IV drip) to provide fluids and painkillers can help to relieve symptoms and prevent complications.
How do you know if you have pancreatitis?
The main signs of acute pancreatitis are sudden and severe pain in the upper abdomen, nausea and vomiting. It is usually caused by gallstones blocking the opening of the pancreas or by drinking too much alcohol.
How long does it take for your pancreas to return to normal?
It can sometimes take several weeks for your appetite to return and to put the weight back on. Advice from a nutritionist can help during this time. In some people, the pancreas doesn’t produce enough digestive juices (for a while) after the pancreatitis has cleared up.
How long after pancreatitis can you drink alcohol?
Some experts recommend not drinking any alcohol at all for 6 to 12 months after each episode of pancreatitis.
Diagnosis
Clinical Trials
Lifestyle and Home Remedies
Alternative Medicine
Specialist to consult
Preparing For Your Appointment
- Tests and procedures used to diagnose pancreatitis include: 1. Blood teststo look for elevated levels of pancreatic enzymes, along with white blood cells, kidney function and liver enzymes 2. Abdominal ultrasoundto look for gallstones and pancreas inflammation 3. Computerized tomog…
Function
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Clinical significance
- Once you leave the hospital, you can take steps to continue your recovery from pancreatitis, such as: 1. Stop drinking alcohol.Even if alcohol was not deemed to be the cause of acute pancreatitis, it is prudent to stop drinking alcohol while recovering. If you're unable to stop drinking alcohol on your own, ask your doctor for help. Your doctor can refer you to local programs to help you stop …
Mechanism
- Alternative therapies can't treat pancreatitis, but some alternative therapies may help you cope with the pain associated with pancreatitis. People with chronic pancreatitis may experience constant pain that isn't easily controlled with medications. Using complementary and alternative medicine therapies along with medications prescribed by your doctor may help you feel more in …
Causes
- Start by seeing your family doctor or a general practitioner if you have any signs or symptoms that worry you. If your doctor suspects you may have pancreatitis, you may be referred to a doctor who specializes in the digestive system (gastroenterologist). Because appointments can be brief, and because there's often a lot to discuss, it's a good idea to be well prepared. Here's some informati…
Prognosis
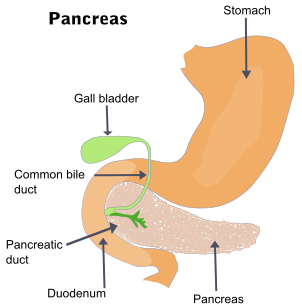
- The pancreas is a large gland in the abdomen located behind the stomach and next to the upper part of the small intestine (the duodenum). The pancreas has two main jobs:
Symptoms
- Pancreatitis is a rare disease in which the pancreas becomes inflamed. Pancreatic damage occurs when the digestive enzymes are activated and begin attacking the pancreas.