Treatment options include:
- Antiseptic mouth rinses, like chlorhexidine or hydrogen peroxide
- Antibiotics
- Minor surgical procedures, in which a surgeon removes tiny parts of the affected bone
- Good oral hygiene practices
- Temporarily stopping antiresorptive medications while the jaw heals
What are the treatment options for jaw necrosis?
Amoxicillin / therapeutic use* Anti-Bacterial Agents / therapeutic use* Bisphosphonate-Associated Osteonecrosis of the Jaw / drug therapy* Bone Density Conservation Agents / administration & dosage Bone Density Conservation Agents / therapeutic use* Bone Regeneration / drug effects Dental Fistula / drug therapy
What is medication-related osteonecrosis of the jaw?
Aug 13, 2020 · Medication Related Osteonecrosis of the Jaw: Drug: Antibiotics Drug: Chlorhexidine mouthwash Procedure: Minimally invasive surgery with LPRF Procedure: Surgical resection: Phase 4
How do you get rid of an infected jaw bone?
Mar 09, 2022 · Osteonecrosis of the jaw is a rare side effect of some drugs for osteoporosis and cancer. But early detection, specialized dentistry, and oral surgery can cure it. Patients with osteoporosis are often prescribed medications that can help prevent severe bone fractures.
Can osteonecrosis of the jaw be reversed?
Jul 31, 2016 · Many authors have studied the management of MRONJ, including different treatments such as surgical debridement, resection of the lesions, oxygen therapy and recently also the use of mesenchymal cells to regenerate the damaged bone ( 7 - 9 ). The type of treatment depends on the diagnosis and clinical stage of MRONJ.
Can osteonecrosis of the jaw be reversed?
Can doctors treat osteonecrosis of the jaw? While there is no specific treatment for ONJ, it can heal on its own with the help of antibiotic rinses and avoiding any other dental surgery.
Is osteonecrosis of the jaw fatal?
Osteonecrosis of the jaw is a rare but serious condition in which the cells in the jawbone start to die. Osteonecrosis of the jaw is a rare but serious condition in which the cells in the jawbone start to die.Feb 22, 2022
What does osteonecrosis of the jaw feel like?
Symptoms of ONJ can range from very mild to severe. ONJ looks like an area of exposed bone in your mouth. It can cause tooth or jaw pain and swelling in your jaw. Severe symptoms include infection in your jaw bone.Oct 29, 2020
How long does osteonecrosis of the jaw take to heal?
For those on high-dose bisphosphonate or denosumab IV therapy or with multiple risk factors for ONJ, it is recommended that the antiresorptive therapy be withheld following the oral surgery until the surgical site has healed with mature soft tissue closure over the wound. This typically requires 4 to 6 weeks.Nov 27, 2015
What are the four stages of osteonecrosis?
Stage 1 has a normal x-rays but MRI reveals the dead bone. Stage 2 can be seen on regular x-ray but there is no collapse of the femoral ball. Stage 3 shows signs of collapse (called a crescent sign) on x-ray. Stage 4 has collapse on x-ray and signs of cartilage damage (osteoarthritis).
What kind of doctor treats osteonecrosis of the jaw?
Once established, osteonecrosis of the jaw is challenging to treat and should be managed by an oral surgeon with experience treating ONJ. Treatment of ONJ typically involves limited debridement, antibiotics, and antibacterial oral rinses (eg, chlorhexidine; 1.
What happens if osteonecrosis is not treated?
If osteonecrosis is not treated, the joint deteriorates, leading to severe arthritis. Osteonecrosis can be caused by disease or by severe trauma, such as a fracture or dislocation, that affects the blood supply to the bone. Osteonecrosis can also occur without trauma or disease.Jun 13, 2021
Can I have a root canal while on Prolia?
Neither bisphosphonates nor denosumab drugs enter or become incorporated into the teeth themselves. So treatment such as prophylaxis, restorations, crowns, bridges, nonsurgical root canal treatments, and nonsurgical periodontal treatment that does not place excessive pressure on alveolar ridges is considered safe.Aug 21, 2014
What are the stages of osteonecrosis of the jaw?
proposed an ONJ classification comprising three stages (31): stage 1 = bone exposure but without signs or symptoms of infection; stage 2 = bone exposure/necrosis with clinical evidence of infection; stage 3 = the above manifestations and also alterations such as pathological fractures, extraoral fistulas or osteolysis ...
What kind of jaw problems does Prolia cause?
Prolia may cause bone loss (osteonecrosis) in the jaw. Symptoms include jaw pain or numbness, red or swollen gums, loose teeth, gum infection, or slow healing after dental work. Osteonecrosis of the jaw may be more likely if you have cancer or received chemotherapy, radiation, or steroids.Feb 11, 2022
What happens if your jaw bone dies?
Sharp fragments of bone may cause painful tongue sores. Large areas of necrotic bone are sometimes associated with loose or painful teeth that may require extraction. At times, numbness or sharp pain may develop if necrotic bone damages a nerve within the jawbones; this is referred to as neuropathic pain.
How does necrosis of the jaw start?
Osteonecrosis of the jaw (ONJ) is classically considered a disruption of vascular supply or avascular necrosis with exposure of the jaw bones. It can be caused by radiation, high-dose steroid therapy, and medications that disrupt vascular supply or bone turnover in the jaws.Mar 11, 2020
What is bone modifying agent?
A history of at least one administration of, or an ongoing treatment with, a bone modifying agent in dose registered for the prevention of skeletal related events in bone metastatic disease or multiple myeloma.
What is a betcon?
BETCON is a pragmatic randomized controlled open-label multi-center study in patients with newly diagnosed stage I-II MRONJ designed to answer the question whether minimally invasive management with LPRF membranes or primary surgical treatment is better than the standard of care of conservative therapy alone. The primary end-point is the time to mucosal healing. Secondary end-points consist of supporting measures of efficacy, patient reported symptoms, quality of life, well-being, and functioning.
What is the best medicine for osteonecrosis of the jaw?
Antibiotic therapy is usually recomended for treatment of osteonecrosis of the jaw. Medications which may be prescribed include: 1 Penicillin or Amoxicillin 2 Clindamycin 3 Vibramycin 4 Erythromycin Ethylsuccinate
How to treat jaw necrosis?
The painful exposed jaw bone can persist for years in many cases, and most experts recommend treatment with antibiotic and preventative actions to avoid jaw infection. The best preventative action for treatment of jaw necrosis is to avoid dental surgery, tooth extraction or other procedures which could irritate or cause ...
Can you take Fosamax before surgery?
The use of Fosamax can lead to a significantly increased risk of osteonecrosis of the jaw. Therefore, if you have been taking Fosamax, it has been recommended that a specialist be consulted before undergoing even the most routine oral surgery. A thorough oral examination should be performed before any dental procedure to avoid exacerbation ...
Does Fosamax cause bone loss?
Studies have also suggested that Fosamax side effects may lead to decay or death of other bones, including the hip , knee or shoulder. The lack of blood flow to the bones may lead to avascular necrosis or osteonecrosis of the hip, knee or shoulder, in addition to decay of the jaw bone.
Can Fosamax cause osteonecrosis?
Studies have shown that osteonecrosis of the jaw may be caused as a side effect of Fosamax and other bisphosphonate medications. If dentists and users of the medication had been made aware of the jaw side effects of Fosamax, they could have avoided dental treatments that may aggravate the condition. Saiontz and Kirk previously pursued Fosamax ...
What does ONJ mean in dentistry?
ONJ looks like an area of exposed bone in your mouth. It can cause tooth or jaw pain and swelling in your jaw. Severe symptoms include infection in your jaw bone. You can get ONJ after some dental surgeries, such as getting teeth extracted (removed) or implanted.
What is the phone number for MSK?
If you're a patient at MSK and you need to reach a provider after 5:00 pm, during the weekend, or on a holiday, call 212-639-2000.
Does bisphosphonate increase the risk of ONJ?
Your risk of ONJ increases the longer you’re treated with bisphosphonates or denosumab. Since people who take these medications to treat cancer usually take them for longer periods and at higher doses than do people with osteoporosis, they are at a higher risk of developing ONJ.
Do you have to wear a mask at MSK?
Masks Are Still Required at MSK. Patients and visitors must continue to wear masks while at MSK, including people who are fully vaccinated. MSK is offering COVID-19 vaccines to all patients age 12 and over. To schedule or learn more, read this. For Adult Patients /.
What are the symptoms of osteonecrosis of the jaw?
Osteonecrosis of the jaw symptoms. The primary symptom of ONJ is the exposure of the mandible or the maxilla to the air through lesions that cut to the bone . However, before ONJ becomes that severe, you may experience the following symptoms: Development of systemic infections: These can be bacterial, fungal, or viral.
What is the best treatment for osteoporosis?
However, antibiotics are often used to treat mild to moderate cases of ONJ. Oral rinses and painkillers: In cases of ONJ related to osteoporosis, conservative treatment with rinses and oral painkillers have proven to be effective.
Why do teeth get pulled?
Dental extractions: These are usually performed because of infections of the teeth and gums. Infections can spread after the procedure and cause bacteria to grow deep within the bones. Growth of bacteria in the bone can cause inflammation and further affect blood flow to these areas.
What is the term for the process of bone deterioration?
Osteonecrosis is a process in which bone cells deteriorate and die. Osteonecrosis of the jaw (ONJ) occurs specifically in the cells of the maxilla and mandible jaw bones. This is a rare condition associated with dental extractions and bone therapies often used in cancer treatments, and occurs when jaw bones become uncovered by ...
How long does it take for an ONJ to develop?
Once ONJ has developed, usually over eight weeks, the primary symptom is lesions that expose bone. Surgery or surgeries to remove ...
Why is my jaw swollen?
A swollen jaw could be a result of abnormalities within the structure of the jaw, issues with the teeth or gums, or swollen glands under the chin. Other swollen jaw causes include viral infections, like the mumps. a traumatic injury, or swollen lymph nodes under the jaw. Face.
Why does my jaw feel stiff?
Jaw stiffness is often associated with pain, tenderness, or swelling, and be caused by a variety of conditions, including anatomy, inflammation-related causes, trauma-related causes, or excess stimulation. Read below to learn more about jaw stiffness and its causes. Face.
What Is Osteonecrosis Of The Jaw?
Osteonecrosis of the jaw occurs due to a lack of blood supply to the jaw bone because the gums aren’t covering the bone. Osteo is a Greek word that means bone, and necrosis means death, so osteonecrosis of the jaw means the death of the jaw bone, which results in little to no blood reaching the jaw bone. There are four stages of ONJ:
What Are The Osteonecrosis Of The Jaw Symptoms?
Early osteonecrosis of the jaw may exist for a long time without any symptoms, although pain is sometimes one of the osteonecrosis of the jaw early symptoms. A purulent discharge from the maxilla or the mandible may be obvious osteonecrosis of the jaw symptoms, as can a jaw bone infection.
What Medications Can Cause Osteonecrosis Of The Jaw?
Many people never develop osteonecrosis of the jaw, but those who have cancer treatments involving specific medications and those who have some specific immune disorders or conditions may be at higher risk of developing ONJ.
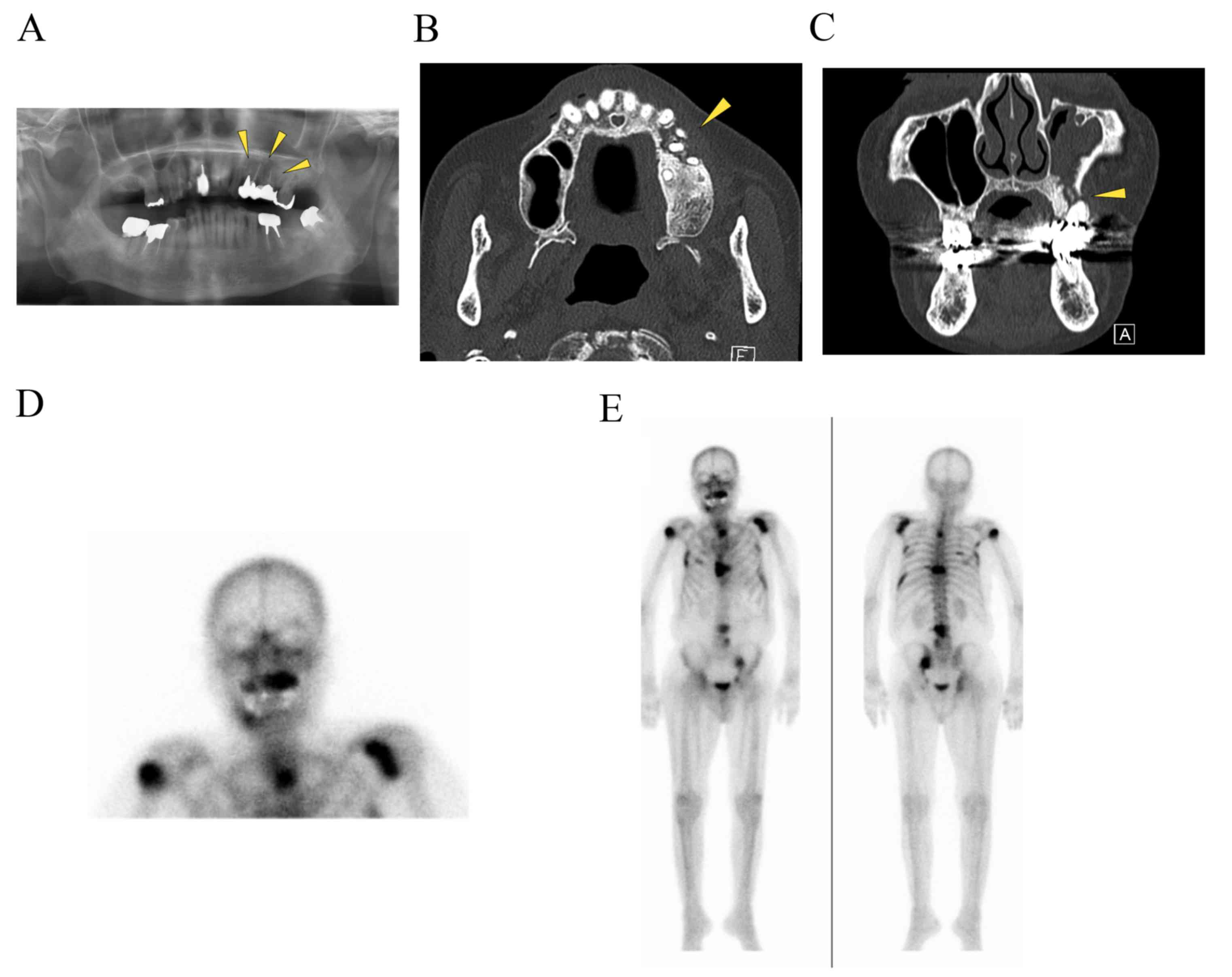
How Is ONJ Diagnosed?
Although there’s no specific diagnostic test for determining risk, osteonecrosis of the jaw is diagnosed by the presence of an exposed jaw bone that has persisted for eight weeks or more. You may have no visible sores in your mouth, but your dentist can determine if you have ONJ. When treated at this early stage, there’s a very good prognosis.
What Are The Treatment Options For ONJ?
The initial treatment options for osteonecrosis of the jaw are typically conservative and include antibacterial mouth rinses, antibiotics, and limited debridement. Since surgical intervention often makes the condition worse, it’s not used unless the initial treatment protocol isn’t effective.
Can Jaw Bone Loss Be Reversed?
At the present time, jaw bone loss reversal is beyond the capabilities of medical science. However, if you have lost bone due to periodontal disease or ONJ, we can perform a bone graft. A bone graft will stimulate growth in the local bone cells, and eventually, your graft will be replaced by your own healthy bone tissue.
How Can ONJ Be Prevented?
A regimen of good oral hygiene is the best method for preventing osteonecrosis of the jaw. Keep your teeth and gums healthy by following the guidelines established by the American Dental Association for good oral health. Brush and floss at least twice daily, and use an antibacterial mouthwash at least once each day.
