Treatment of MDR-TB requires treatment with second-line drugs, usually four or more anti-TB drugs for a minimum of 6 months, and possibly extending for 18–24 months if rifampin resistance has been identified in the specific strain of TB with which the patient has been infected. Under ideal program conditions, MDR-TB cure rates can approach 70%.
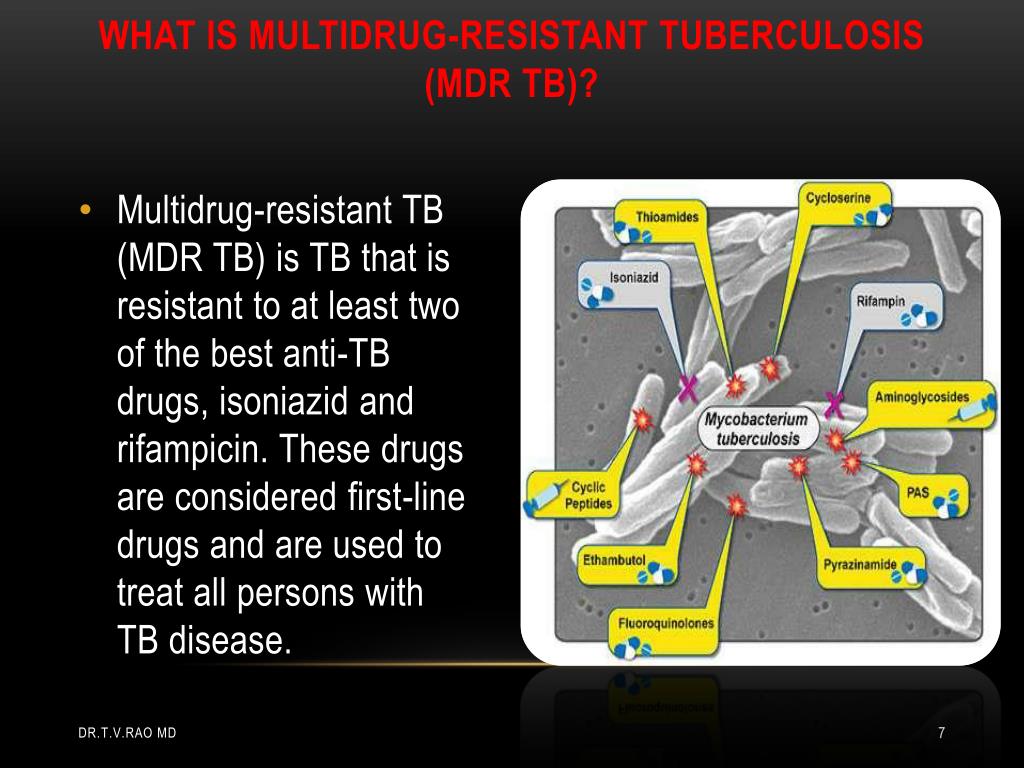
What is multidrug resistant tuberculosis (MDR TB)?
Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. These drugs are used to treat all persons with TB disease. What is extensively drug resistant tuberculosis (XDR TB)?
What drugs are used to treat extensively drug resistant tuberculosis (XDR)?
These drugs are used to treat all persons with TB disease. What is extensively drug resistant tuberculosis (XDR TB)? Extensively drug resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin).
What is MDR-TB and how is it treated?
MDR-TB is a form of TB caused by mycobacteria that have become resistant to the two most effective anti-TB drugs, isoniazid and rifampicin. As a consequence, MDR-TB needs to be treated with other drugs, known as second-line drugs.
How can health care providers help prevent MDR TB?
Health care providers can help prevent MDR TB by quickly diagnosing cases, following recommended treatment guidelines, monitoring patients’ response to treatment, and making sure therapy is completed.

What is the treatment for multidrug-resistant TB?
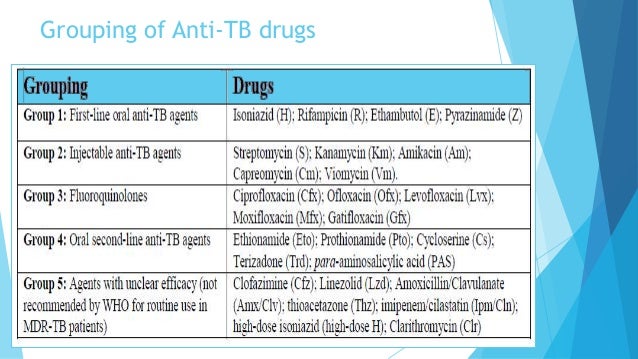
Levofloxacin and moxifloxacin are the two most frequently recommended agents, and the WHO has recommended the use of these drugs for the treatment of MDR-TB. The optimal dose of levofloxacin is 750 mg once daily and that of moxifloxacin is 400 mg once daily.
Which drugs are used in the treatment of Multi Drug Resistance tuberculosis MDR-TB )?
Which medications are used for the treatment of multidrug-resistant tuberculosis (MDR-TB)?A fluoroquinolone: levofloxacin or moxifloxacin preferred.Bedaquiline.Linezolid.Clofazimine (available only through Investigational New Drug application through FDA)Cycloserine.More items...
Is MDR-TB treatable?
In most cases, TB is treatable and curable; however, people with TB can die if they do not get proper treatment. Sometimes drug-resistant TB occurs when bacteria become resistant to the drugs used to treat TB. This means that the drug can no longer kill the TB bacteria.
Can MDR-TB be treated and cured?
Although MDR-TB presents a major challenge to TB control, effective treatment can result in cure.
How is MDR treated and how long is the treatment?
The recommended dose of bedaquiline for the treatment of pulmonary MDR in adults is: Weeks 1 – 2: 400 mg (4 tablets of 100 mg) given orally, once daily. Weeks 3 – 24: 200 mg (2 tablets of 100 mg) three times per week, for a total dose of 600 mg per week.
What is the current treatment for tuberculosis?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
What is the most appropriate treatment for a patient with multi antibiotic resistant TB?
Fluoroquinolones are often the most effective anti-TB drugs in an MDR-TB regimen.
How long is drug resistant TB treated?
The intensive-phase treatment for MDR-TB should be 5-7 months, followed by the continuation phase, so that the total duration of treatment is 15-24 months after culture conversion. The drugs should be prescribed daily (no intermittent therapy), and the patient should always be on DOT.
How do you know if MDR-TB treatment is working?
Physical Signs That TB Treatment Is WorkingA reduction in symptoms, such as less coughing.Overall improvement in the way one feels.Weight gain.Increased appetite.Improvement in strength and stamina.
How can MDR be prevented?
How can MDR TB be prevented? The most important thing a person can do to prevent the spread of MDR TB is to take all of their medications exactly as prescribed by their health care provider. No doses should be missed and treatment should not be stopped early.
What Is Tuberculosis (TB)?
Tuberculosis (TB)(https://www.cdc.gov/tb/publications/factsheets/general/tb.htm) is a disease caused by bacteria that are spread from person to per...
What Is Multidrug-Resistant Tuberculosis (MDR TB)?
Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. These...
What Is Extensively Drug Resistant Tuberculosis (XDR TB)?
Extensively drug resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least...
How Does Drug Resistance Happen?
Resistance to anti-TB drugs can occur when these drugs are misused or mismanaged. Examples include when patients do not complete their full course...
Who Is at Risk For Getting MDR TB?
Drug resistance is more common in people who: 1. Do not take their TB medicine regularly 2. Do not take all of their TB medicine as told by their d...
How Can MDR TB Be Prevented?
The most important thing a person can do to prevent the spread of MDR TB is to take all of their medications exactly as prescribed by their health...
Is There A Vaccine to Prevent TB?
Yes, there is a vaccine for TB disease called Bacille Calmette-Guérin (BCG)(https://www.cdc.gov/tb/publications/factsheets/prevention/bcg.htm). It...
What Should I Do If I Think I Have been Exposed to Someone With TB Disease?
If you think you have been exposed to someone with TB disease, you should contact your doctor or local health department about getting a TB skin te...
What Are The Symptoms of TB Disease?
The general symptoms of TB disease include feelings of sickness or weakness, weight loss, fever, and night sweats. The symptoms of TB disease of th...
What is MDR-TB?
MDR-TB is a form of TB caused by mycobacteria that have become resistant to the two most effective anti-TB drugs, isoniazid and rifampicin. As a consequence, MDR-TB needs to be treated with other drugs, known as second-line drugs. The treatment is longer, more expensive and more difficult. Like other bacteria, mycobacteria can undergo genetic changes (known as mutations), which can make them naturally resistant to an anti-TB drug. In this instance, treatment with 3 or 4 drugs can prevent the resistant mycobacteria from growing and replacing ‘sensitive’ mycobacteria that have been eliminated by the usual TB treatment.
What causes MDR-TB?
The main causes of MDR-TB are: inappropriate medical prescription; poor quality of anti-TB drugs; interruptions in treatment; nonexistent national TB control programmes; lack of standardised guidelines; inefficient supervision by healthcare providers; and failure to complete treatment. Failure to suspect or detect MDR-TB will give resistant mycobacteria more time to spread to other individuals in the community and worsen the problem.
What are the symptoms of MDR-TB?
MDR-TB causes identical symptoms and involves the same organs as usual TB (weight loss, low-grade fever and tiredness, with cough, sputum production and chest pain if mycobacteria are in the lungs) but the disease will last longer because the mycobacteria are removed more slowly or are not destroyed at all.
What is multi-drug resistant tuberculosis?
Multi-Drug Resistant Tuberculosis (MDR-TB) is defined as the disease caused by Mycobacterium Tuberculosis resistant to at least Isoniazid & Rifampicin , with or without resistance to other anti-TB drugs. Contrary to earlier belief, multi-drug resistant Mycobacteria have proved to be as infectious as drug susceptible ones & can cause severe disease. Erratic prescribing by physicians & patient non-adherence to the treatment regimens are the major causes leading to the emergence of MDR-TB. World Health Organization (WHO) has issued guidelines for the management of MDR-TB. The regimens for the treatment of MDR-TB are designed according to the availability / unavailability of drug susceptibility test results. Second line anti-Tuberculosis (anti-TB) drugs and the newer agents have vital role in treatment of MDR-TB. Directly Observed Therapy (DOT) is strongly recommended for all anti-TB regimens. In general, the treatment of MD R-TB is costlier, less effective & more toxic as compared to treatment of drug susceptible Tuberculosis. In last few years there has been increased incidence of what has been described as ‘Extensively Drug Resistant Tuberculosis (XDR-TB). A WHO consultation in held in March 2012 has come up with the diagnostic definition and various treatment options for the management of Extensively Drug Resistant Tuberculosis (XDR-TB).
What antibiotics are used for MDR TB?
There are reports suggesting the usefulness of b-Lactam antibiotics such as Imipenem, Amoxicillin – Clavulanic acid in treatment of MDR-TB. Linezolid is an oxazolidinone derivative, which acts by inhibiting early steps of protein synthesis in the Mycobacteria & is found to be useful in MDR-TB. Several other drugs such as interferon-g, recombinant human interleukin 2 have been reportedly useful in MDR-TB. Currently these drugs are under clinical trials. As the treatment of MDR-TB has been found to be less effective, resectional surgery has been advocated in selected patients of MDR-TB who have good respiratory reserve & in whom drug treatment alone is not working.
Which is the first line of TB treatment?
Isoniazid ( INH ) , Rifampicin , Pyrazinamide , Ethambutol& Streptomycin are labeled as the first line drugs which have high efficacy & less adverse effects. These agents are routinely used for the treatment of TB. Isoniazid & Rifampicin are the two most potent drugs in the treatment of TB.
Is multi-drug resistant TB less effective?
In general, the treatment of Multi-Drug Resistant TB is less effective . The cost of the treatment as well as the incidence of adverse effects is higher in comparison to the treatment of drug susceptible TB. The WHO has issued important guidelines for the management of drug / Multi-Drug Resistant TB.
Is MDR TB resistant to INH?
It is defined as the disease caused by M.Tuberculosis that is resistant to at least Isoniazid (INH) & Rifampicin, with or without resistance to other anti-TB drugs6. The drug treatment of MDR-TB is difficult as the options are limited owing to the resistance to INH & Rifampicin, two of the most potent anti-TB drugs.
Is TB a global health problem?
Tubercul osis (TB) continues to ha unt mankind & remains a world wide health problem even today, despite isolation of its causative agent, advent of BCG Vaccine & availability of effective chemotherapeutic agents. According to WHO, one third of the world population is infected with Mycobacterium Tuberculosis. The disease is taking heavy toll on the third world countries of Asia & Africa. HIV epidemic & emergence of resistant forms of TB especially MDR-TB together have added a new dimension to the problem. It is well known that people living with HIV/AIDS are very susceptible to contracting TB as compared to general population. The incidence of MDR-TB is also higher in these patients. In the last two decades there have been a number of outbreaks of M D R-TB in United States & other parts of the world. These outbreaks were marked by very high mortality rates. WHO has taken cognizance of the problem. In fact the WHO declaration of TB as a “ Global Emergency” in 1993 was prompted by the emergence of M. D. R. –TB. The management of TB is getting even more complicated with the emergence of Extremely Drug Resistant TB (XDR-TB), a form of Multi Drug Resistant TB where the M. Tuberculosis is resistant not only to the first line anti TB agents but also to the second line anti TB agents.
Is TB a drug resistant disease?
Although there is increased incidence of Tuberculosis (TB) patients with severe patterns of drug resistance which is posing a formidable challenge to the clinicians, a new definition of resistance beyond Extensively Drug-Resistant TB (XDR-TB ) is not recommended , owing to the technical difficulties with drug susceptibility testing (DST) of many anti-TB drugs, insufficient evidence to link such DST results to treatment outcomes of patients, and the lack of standardized DST methods for several anti-TB drugs.