
Explore
The best-studied alternative to steroid–cytotoxic drug therapy for MN is cyclosporine, usually employed in relatively low doses of 3.5–5 mg/kg/day adjusted to trough levels of 150–225 mg. Cyclosporine does reduce protein excretion in MN, usually by 30–50%, and about 70% of patients show occasional complete or more commonly partial remission. [ 19]
How to diagnose and treat membranous nephropathy?
Considerable evidence supports the use of B-cell depletion as initial therapy in nephrotic patients with MN. ACTH should be considered for patients who do not respond to traditional therapies such as alkylating agents and calcineurin inhibitors. Keywords:
Does membranous nephropathy go away on its own?
Some people with MN end up with kidney failure. These people may need a kidney transplant or dialysis (long-term treatment where a machine filters the blood for the kidneys). MN can come back after treatment. Your nephrologist may monitor your kidney function regularly to look for signs that the disorder has returned.
What are the long-term complications of membranous nephropathy?
There is no specific treatment for membranous nephropathy. Supportive care with the use of diuretics and angiotensin-converting enzyme inhibitors in combination with angiotensin II receptor blocker is recommended, but these agents have only a limited effect.
What are the treatment options for nephrotic syndrome (NS) with nephropathy?
Treatment of MN usually involves several different parts that are managed by a nephrologist (kidney specialist). ACE-inhibitor or ARB – these are blood pressure medications that can decrease the amount of protein in the urine. These medications are …
How serious is membranous nephropathy?
In mild cases, membranous nephropathy may get better on its own, without any treatment. As protein leakage increases, so does the risk of long-term kidney damage. In many, the disease ultimately leads to kidney failure.Dec 3, 2020
Is membranous nephropathy a kidney disease?
Membranous nephropathy, also called membranous glomerulonephritis, is a rare kidney disease that affects the filters, or glomeruli, of your kidneys. These filters usually help remove waste and fluids. But when the glomeruli become inflamed, your kidneys may swell and stop working properly.May 18, 2021
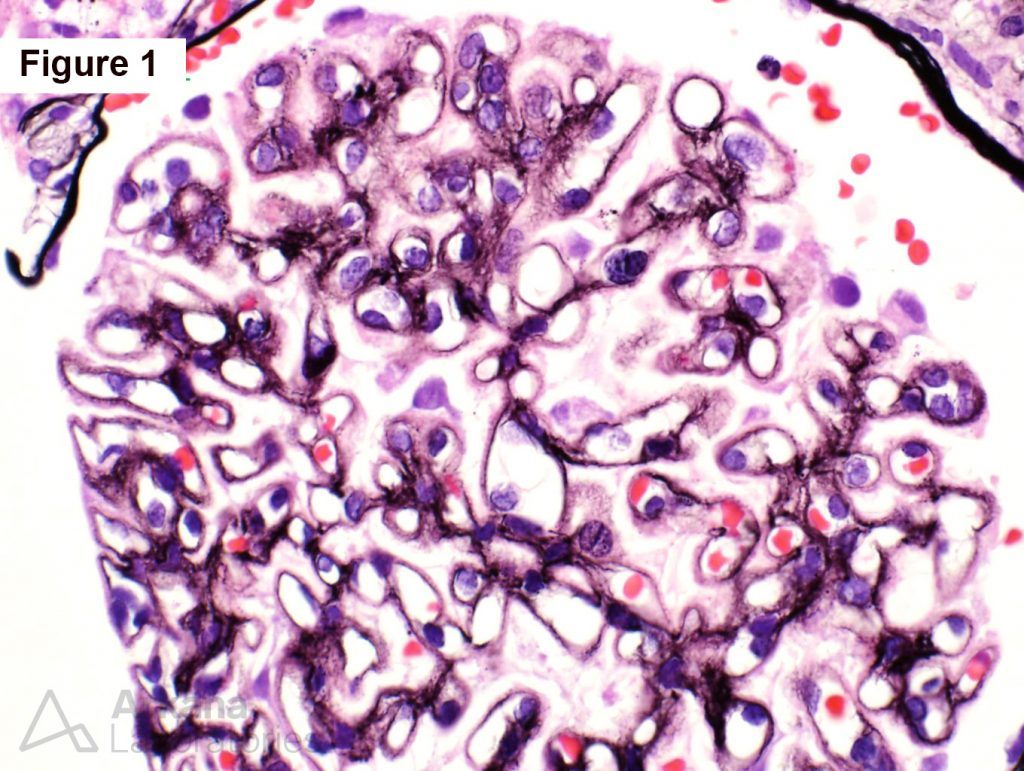
What is stage 2 membranous nephropathy?
Four pathological stages of membranous nephropathy. Stage I is characterized by the presence of immune-complex-type electron-dense deposits in the subepithelial zone between the basement membrane and the podocyte. Stage II is characterized by projections of basement membrane material around the subepithelial deposits.
How common is membranous nephropathy?
Membranous nephropathy (MN) is the second most common nephropathy in adults after focal segmental glomerulosclerosis (FSGS). [5] It is the most common cause of primary nephrotic syndrome in White adults. [6] It most commonly occurs above 40 years of age, with the peak incidence between 50 to 60 years in the USA.Oct 11, 2021
Who does membranous nephropathy affect?
Who gets Membranous Nephropathy? MN is most common in older-middle aged adults, in their 50s and 60s, though can occur earlier or later. It is rare in children. Men are affected more often than women, and it is much more common in Caucasians (versus blacks).
What is another name for membranous nephropathy?
Membranous glomerulonephritis (MGN) is a specific type of GN. MGN develops when inflammation of your kidney structures causes problems with the functioning of your kidney. MGN is known by other names, including extramembranous glomerulonephritis, membranous nephropathy, and nephritis.
How long can you live with membranous nephropathy?
There is no certain cure. However, up to three out of 10 people with membranous nephropathy have their symptoms completely disappear (remission) after five years without any treatment.Dec 3, 2020
Is membranous nephropathy a disability?
Nephrotic syndrome is listed as a qualifying disability under the SSA's Blue Book under Medical Listing 6.06. According to this listing, an individual must be suffering from nephrotic syndrome with anasarca and the condition must persist for at least three months despite prescribed treatments and therapy.
What is membranous nephropathy?
Membranous nephropathy (MN) is a type of glomerular disease and is an autoimmune disease. An autoimmune disease is caused when your body's defense system turns against you and harms your body when it should be protecting you. Your defense system is known as your immune system which is “turned on” by glomerular disease.
Can you live a long life with proteinuria?
For example, the life expectancies of 40-year-old men and women with no proteinuria were 15.2 and 17.4 years longer, respectively, than those with heavy proteinuria. Proteinuria-free men and women also outlived those with mild proteinuria by 8.2 years and 10.5 years, respectively.Mar 21, 2013
Will drinking water reduce protein in urine?
Drinking water will not treat the cause of protein in your urine unless you are dehydrated. Drinking water will dilute your urine (water down the amount of protein and everything else in your urine), but will not stop the cause of your kidneys leaking protein.
What food should be avoided during nephrotic syndrome?
Restrictions and foods to avoid on a nephrotic syndrome dietprocessed cheeses.high-sodium meats (bologna, ham, bacon, sausage, hot dogs)frozen dinners and entrées.canned meats.pickled vegetables.salted potato chips, popcorn, and nuts.salted bread.
What is the name of the disease in which the kidneys are responsible for cleaning waste products from the blood?
The kidneys have filters that are responsible for cleaning waste products from your blood. In membranous nephropathy (MN), these filters are attacked by the body’s immune system. Grouped together, the symptoms of this disease are called nephrotic syndrome. Treatment for MN depends on the type and cause of the condition.
What are the complications of membranous nephropathy?
Health issues and complications from membranous nephropathy can include: High cholesterol (higher than average levels of fat in the blood). Severe swelling (called nephrotic syndrome ). Kidney failure. Additional complications that can happen due to MN can include:
What are the three layers of a blood vessel?
These filtering units are made up of blood vessels so small, they only have three layers: Endothelial cells: These cells are part of a single layer of cells on the inside of the blood vessel. Podocytes: These cells are in a single layer of cells on the outside of the blood vessel.
What is the glomerular basement membrane?
Glomerular basement membrane (GBM): The GBM is a thin membrane in between the two layers of cells. The glomerular basement membrane is so thin that it acts as a filter. MN can develop very suddenly or slowly get worse over a long time. Some people do not know they have the condition for many years.
What is primary MN?
Instead of targeting an infection, these antibodies attack the podocytes. The podocytes stop retaining the proteins in the blood stream and allow them to leak into the urine. This is called primary MN. Less commonly, MN can be due to other causes ( secondary MN), such as:
What are the symptoms of MN?
Together, the symptoms of MN are called nephrotic syndrome. Signs of nephrotic syndrome include: Edema (swelling caused by fluid retention, most commonly in the legs and feet). High cholesterol.
What are the symptoms of a renal vein thrombosis?
Symptoms of each condition can include: Pulmonary embolism: Sharp chest pain that is worse when you take a breath. Deep vein thrombosis: Pain or swelling in one leg.
Is membranous nephropathy a glomerular disease?
Idiopathic membranous nephropathy is still the most common glomerular disease associated with nephrotic syndrome. The greater the proteinuria, the greater the long-term risk for renal failure. In addition, patients who have membranous nephropathy with nephrotic syndrome have significant morbidity and mortality, ...
What is the best treatment for immunosuppression?
Immunosuppressive treatment options include the use of corticosteroids, alkylating agents, cyclosporin A, tacrolimus, and mycophenolate mofetil, but their use is controversial, not all have been shown to be effective, and their use can be associated with significant adverse effects.
What is a MN?
What is Membranous Nephropathy? Membranous Nephropathy (MN) is a kidney disease that affects the filters ( glomeruli) of the kidney and can cause protein in the urine, as well as decreased kidney function and swelling. It can sometimes be called membranous glomerulopathy as well (these terms can be used interchangeably and mean the same thing).
Is nephropathy an autoimmune disease?
Membranous nephropathy is considered an autoimmune disease, which means that it caused by the body’s own immune system. MN is caused by the build-up of immune complexes within the filters (glomeruli) of the kidney itself.The immune system normally creates antibodies to recognize and attach to something (called an antigen).
What is the most common cause of nephrotic syndrome?
It can sometimes be called membranous glomerulopathy as well (these terms can be used interchangeably and mean the same thing). Membranous nephropathy is one of the most common causes of the nephrotic syndrome in adults. Nephrotic syndrome includes significant amounts of protein in the urine (at least 3.5 grams per day), ...
Can nephropathy cause protein loss?
Membranous nephropathy often causes nephrotic syndrome. Nephrotic syndrome is a group of symptoms or changes that often occur together in someone that is losing a lot of protein into the urine. Nephrotic syndrome can also happen in other diseases that cause a lot of protein to be lost into the urine. Although a lot of people with MN have nephrotic syndrome, not everybody does. Nephrotic syndrome includes these findings:
What is the MN antibody?
In most cases of MN, antibodies are made to an antigen that is part of the kidney filter (glomerulus) itself. Together these antibodies and antigens create immune complexes that get stuck in the kidney filter (glomerulus) and cause disease. Recently the antibody that causes most cases of membranous nephropathy was discovered and identified.
Can nephropathy be delayed?
Membranous nephropathy is an uncommon disease and diagnosis can sometime be delayed. Since swelling, the most common symptom, can be caused by a lot of different diseases or problems (including kidney, heart, or liver problems), the kidneys may not be identified right away as the cause.
What is a kidney biopsy?
A kidney biopsy is a procedure that involves using a needle to get a sample of kidney tissue to look at under the microscope. This allows the individual glomeruli (kidney filters) to be seen under high magnification. Additional tests can be done on the kidney tissue from the biopsy to help make a diagnosis.
What is membrane nephropathy?
Membranous nephropathy (MEM-bruh-nus nuh-FROP-uh-thee) occurs when the small blood vessels in the kidney (glomeruli), which filter wastes from the blood, become damaged and thickened. As a result, proteins leak from the damaged blood vessels into the urine (proteinuria). For many, loss of these proteins eventually causes signs ...
Can gold salts cause nephropathy?
Certain medications, such as gold salts and nonsteroidal anti-inflammatory drugs. Solid cancerous tumors or blood cancers. Membranous nephropathy may also occur along with other kidney diseases, such as diabetic nephropathy and rapidly progressive (crescentic) glomerulonephritis.
What are the symptoms of membranous nephropathy?
Signs and symptoms of membranous nephropathy include: Swelling in the legs and ankles. Weight gain.
What is the immune system that attacks the kidneys?
Your body's immune system mistakes healthy tissue as foreign and attacks it with substances called autoantibodies. These autoantibodies target certain proteins located in the kidney's filtering systems (glomeruli). This is known as primary membranous nephropathy. Sometimes membranous nephropathy is brought on by other causes.
What are the risks of proteinuria?
Blood clots. With proteinuria, you may lose proteins that help prevent clotting from your blood into your urine.
Why do you need dialysis?
You may need emergency dialysis to remove extra fluids and waste from your blood. Chronic kidney disease.
What is the function of the glomeruli?
The glomeruli filter waste products and substances your body needs — such as so dium, phosphorus and potassium — which then pass through tiny tubules. The substances your body needs are reabsorbed into your bloodstream. The waste products flow through the ureters — the tubes that lead to the bladder.
What causes MN?
There are two kinds of MN: idiopathic (or primary) MN and is more common than secondary MN, which is caused by another disease or drug. Although there has been progress in learning about the autoimmune cause of primary MN, a lot more research is needed to find the reason the immune system is triggered. The most common causes of secondary MN are: 1 Hepatitis B virus 2 Non-steroidal anti-inflammatory drugs (NSAIDs) 3 Systemic lupus erythematosus (lupus for short) 4 Cancer 5 Other diseases and infections
What is the most common cause of nephrotic syndrome?
MN is one of the most common causes of nephrotic syndrome. When your immune system attacks the glomeruli in membranous nephropathy, it causes changes to the filters that lead you to lose large amount of protein into the urine. If this continues at high levels, it can eventually lead to kidney failure.
What is glomerular disease?
Glomerular diseases include many conditions with many different genetic and environmental causes. Membranous nephropathy (MN) is a type of glomerular disease and is an autoimmune disease. An autoimmune disease is caused when your body’s defense system turns against you and harms your body when it should be protecting you.
Does salt help with edema?
Low-salt diet: Lowering salt may help to reduce edema (swelling in your body parts like your legs, and around your eyes) If your symptoms do not go away after supportive care, you may be given treatments that affect your immune system. The goal of your treatment is to manage your symptoms.
What are the symptoms of membranous nephropathy?
Signs and symptoms of membranous nephropathy include: Swelling in body parts like your legs, ankles and around your eyes (called edema) Foaming of the urine caused by high protein levels in the urine (called proteinuria)
Is membranous nephropathy a glomerular disease?
Idiopathic membranous nephropathy is still the most common glomerular disease associated with nephrotic syndrome. The greater the proteinuria, the greater the long-term risk for renal failure. In addition, patients who have membranous nephropathy with nephrotic syndrome have significant morbidity and mortality, in particular related to thromboembolic and cardiovascular complications. There is no specific treatment for membranous nephropathy. Supportive care with the use of diuretics and angiotensin-converting enzyme inhibitors in combination with angiotensin II receptor blocker is recommended, but these agents have only a limited effect. Immunosuppressive treatment options include the use of corticosteroids, alkylating agents, cyclosporin A, tacrolimus, and mycophenolate mofetil, but their use is controversial, not all have been shown to be effective, and their use can be associated with significant adverse effects. This has resulted in relatively small improvement in the prognosis of membranous nephropathy in the past 30 yr, with up to 40% of patients eventually reaching end-stage renal failure. Agents that offer more complete response rates with lower adverse effects are truly needed. Recent data suggest that B cells play a key role in the pathogenesis of a number of autoimmune diseases including membranous nephropathy and that selective depletion of B cells in humans may be beneficial in preventing the production of pathogenic immunoglobulins and subsequent renal injury.
Can cytotoxic agents be combined with corticosteroids?
In relation to cytotoxic agents combined with corticosteroids, there has not been a randomized, controlled trial of cytotoxic agents plus corticosteroids in this high-risk group, although a number of uncontrolled studies have been conducted ( 46, 47, 49, 58 – 69 ). In patients with deteriorating renal function, the supporting data are much less compelling than the results obtained in patients at medium risk for progression; adverse effects, especially infections, are higher; and the likelihood of benefit is reduced in patients with severe renal failure (serum creatinine >3 mg/dl).

Treatment
- Treatment of membranous nephropathy focuses on addressing the cause of your disease and relieving your symptoms. There is no certain cure. However, up to three out of 10 people with membranous nephropathy have their symptoms completely disappear (remission) after five yea…
Clinical Trials
Lifestyle and Home Remedies
Preparing For Your Appointment