Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional support, and other therapies. You may also receive palliative treatments similar to those meant to treat the MDS, such as chemotherapy (see above).
How to cure leukemia naturally?
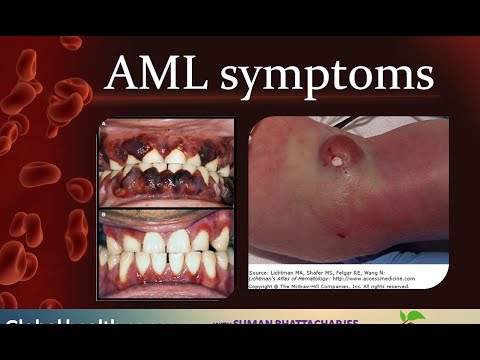
Leukemia Symptoms
- swollen lymph nodes (neck, underarm, groin or stomach)
- enlarged spleen or liver
- frequent infections
- fever
- pale skin tone
- night sweats
- fatigue (feeling very tired)
- unplanned weight loss (10% of body weight over 6 months)
- bone or joint pain and/or tenderness
- easy bruising or bleeding
When does MDS become AML?
MDS can turn into acute leukaemia (AML) and this is caused by the acquisition of new changes in the DNA. Azacitidine is the only PBS funded medication to treat MDS, but the underlying mechanisms of response are still poorly understood.
What is the natural cure for leukemia?
Natural Remedies and Herbs for Leukemia
- Grape Seed Extract - Grape seed extract comes from the seeds of red wine grapes. ...
- Green Tea - Green tea is brewed from the Camellia sinensis plant. ...
- Astragalus - This leukemia home remedy is a Chinese root herb that helps boost the immune system. ...
What are some of the common treatments for leukemia?
What are the current treatment options for older adults with leukemia?
- Watch and wait. If you have a chronic type of leukemia and are relatively healthy, your doctor may recommend watching and waiting before beginning treatment.
- Chemotherapy. Chemotherapy is a common treatment for leukemia in people of all ages. ...
- Stem cell transplant. ...
- Medications. ...
How long can you live with MDS with treatment?
With current treatments, patients with lower-risk types of some MDS can live for 5 years or even longer. Patients with higher-risk MDS that becomes acute myeloid leukemia (AML) are likely to have a shorter life span.
What is the best treatment for MDS?
A bone marrow transplant, also known as a stem cell transplant, is the only treatment option that offers the potential of a cure for myelodysplastic syndromes.
Is MDS leukemia curable?
MDS cannot be cured with chemotherapy. An allogeneic bone marrow transplant (BMT) is the only potential cure for patients with MDS.
What is the survival rate of MDS?
Survival statistics for MDSIPSS-R risk groupMedian survivalVery low8.8 yearsLow5.3 yearsIntermediate3 yearsHigh1.6 years1 more row•Jan 22, 2018
What are the end stages of MDS?
MDS progresses over time in two ways. In most people with MDS, fewer and fewer healthy blood cells are produced or survive. This can lead to severe anemia (low RBCs), increased risk of infection (due to low WBCs) or risk of severe bleeding (due to low platelets).
Is MDS always fatal?
MDS is a potentially fatal disease; the common causes of death in a cohort of 216 MDS patients included bone marrow failure (infection/hemorrhage) and transformation to acute myeloid leukemia (AML).
Does chemotherapy cure MDS?
The chemo drug most often used for MDS is cytarabine (ara-C). It can be given by itself at a low-dose, which can often help control the disease, but doesn't often put it into remission. Another option is to give the same, intense type of chemo that is used for younger patients with AML.
How fast does MDS progress?
The pace of progression varies. In some individuals the condition worsens within a few months of diagnosis, while others have relatively little problem for several decades. In about 50 percent of cases, MDS deteriorates into a form of cancer known as acute myeloid leukemia (AML).
Is a bone marrow transplant a cure for MDS?
How does blood or marrow transplant (BMT) work for MDS? BMT, also known as a bone marrow transplant or blood stem cell transplant, can treat patients who have MDS, including older patients. It replaces the unhealthy blood-forming cells (stem cells) with healthy ones. For some people, transplant can cure MDS.
How serious is MDS?
MDS is a severe, chronic syndrome. The recovery rate varies as it often progresses to AML, a form of leukemia. An individual's outlook depends on the progression of MDS and treatment success. A stem cell transplant provides the highest chance of curing the condition.
What causes death in MDS patients?
Death from MDS is often caused by bleeding and/or infection from low blood cell counts or after the disease becomes acute myeloid leukemia (AML). About a third of patients with MDS develop AML.
Are there any new treatments for MDS?
FDA Approves New Therapy for Myelodysplastic Syndromes (MDS) That Can Be Taken at Home. Today, the U.S. Food and Drug Administration approved Inqovi (decitabine and cedazuridine) tablets for treatment of adult patients with myelodysplastic syndromes (MDS) and chronic myelomonocytic leukemia (CMML).
What are the goals of low risk MDS patients?
The goals for low-risk MDS patients are to. Improve blood counts. Lessen the need for blood transfusions. Lower the risk of infection. Improve the quality of life. High-risk MDS tends to grow quickly and progress to AML within a shorter time. For this reason, more intensive treatments are generally used.
Who should evaluate a patient for MDS?
Every patient’s situation should be evaluated individually by a hematologist-oncologist who specializes in treating MDS and who will discuss the disease subtype, prognostic factors and treatment options with the patient. It is also important to seek treatment at a center that has experience in treating MDS.
Can you participate in a clinical trial for allogeneic stem cell transplantation?
Allogeneic stem cell transplantation. Your doctor may suggest that you participate in a clinical trial. Clinical trials can involve therapy with new drugs and new drug combinations or new approaches to stem cell transplantation.
What happens if you have MDS?
Over time, people with MDS have more abnormal blood cells than healthy ones, which can lead to conditions such as anemia, leukopenia (a drop in white blood cell count), and thrombocytopenia (a drop in platelet count). About 25% to 30% of people with MDS will develop acute myeloid leukemia, a fast-growing cancer of bone marrow cells. ...
Why does MDS not cause symptoms?
MDS Symptoms. Because failure of the bone marrow to produce normal mature cells is a slow process , MDS might not cause symptoms in its early stages. As the disease progresses, patients might experience: Fatigue. Recurrent infections, due to leukopenia (low white blood cell count)
What is the purpose of blood transfusions?
Blood transfusions to replace red blood cells or platelets. Medications with the goal of increasing the number of blood cells, suppressing the immune system, stimulating blood cells to mature, or treating infections. Bone marrow transplant to replace abnormal bone marrow stem cells with healthy, donated cells.
What tests are used to confirm a diagnosis?
To confirm a diagnosis, we might recommend additional tests, such as: Blood tests: Tests that identify the number of red cells, white cells, and platelets and look for changes in the appearance of various blood cells. Bone marrow aspirate and biopsy: Removal of a small amount of liquid bone marrow and piece of bone, typically from the hipbone, ...
What are the risk factors for MDS?
Risk factors for MDS include: Older age (most people with the disease are older than 65) Chemotherapy or radiation treatment. Exposure to tobacco, pesticides, or other toxic chemicals. Exposure to heavy metals, such as lead or mercury.
Is MDS a center of excellence?
It is nationally recognized by the MDS Foundation as a center of excellence for the treatment of people with MDS. Our specialists are renowned for providing state-of-the-art care and advancing research related to cancer and blood diseases.
Supportive therapy
Supportive therapy is meant to treat MDS symptoms and prevent complications, rather than treat the underlying disorder itself. Supportive therapy is often used alongside other treatments.
Lenalidomide
Lenalidomide is a type of medication called an immunomodulatory agent. Your doctor may suggest this oral medication if you have MDS and a certain genetic change known as an isolated del (5q) chromosome abnormality.
Antithymocyte globulin
Antithymocyte globulin is in a large group of drugs known as immunosuppressants that weaken the body’s immune response. Organ transplant recipients usually take them to help prevent rejection of the new organ. You may take antithymocyte globulin to keep your immune system from attacking stem cells in your bone marrow.
Chemotherapy
Certain chemotherapy drugs, known as hypomethylating agents, activate specific genes in your stem cells to help them mature. Two examples of these agents are azacitidine and decitabine. These drugs are used when your doctor determines there is a serious risk for leukemia, which is a serious potential complication of MDS.
Stem cell transplant
A stem cell transplant involves removing some of your bone marrow, usually from the pelvic bone, and replacing it with bone marrow that produces healthy blood cells.
What are the different types of myelodysplastic syndrome?
The different types of myelodysplastic syndromes are diagnosed based on certain changes in the blood cells and bone marrow. Refractory anemia: There are too few red blood cells in the blood and the patient has anemia. The number of white blood cells and platelets is normal.
What is myelodysplastic syndrome?
Key Points. Myelodysplastic syndromes are a group of cancers in which immature blood cells in the bone marrow do not mature or become healthy blood cells. The different types of myelodysplastic syndromes are diagnosed based on certain changes in the blood cells and bone marrow. Age and past treatment with chemotherapy or radiation therapy affect ...
What is the term for a group of cancers in which immature blood cells in the bone marrow
Myelodysplastic syndromes are a group of cancers in which immature blood cells in the bone marrow do not mature or become healthy blood cells. In a healthy person, the bone marrow makes blood stem cells (immature cells) that become mature blood cells over time. Anatomy of the bone.
What is PDQ cancer?
This PDQ cancer information summary has current information about the treatment of myelodysplastic syndromes. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
What is the difference between a myeloid and a lymphoid stem cell?
A lymphoid stem cell becomes a white blood cell. A myeloid stem cell becomes one of three types of mature blood cells: Red blood cells that carry oxygen and other substances to all tissues of the body.
Can myelodysplastic syndrome cause shortness of breath?
Signs and symptoms of a myelodysplastic syndrome include shortness of breath and feeling tired. Myelodysplastic syndromes often do not cause early signs or symptoms. They may be found during a routine blood test. Signs and symptoms may be caused by myelodysplastic syndromes or by other conditions.
Do myelodysplastic cells die?
In a patient with a myelodysplastic syndrome, the blood stem cells (immature cells) do not become mature red blood cells, white blood cells, or platelets in the bone marrow. These immature blood cells, called blasts, do not work the way they should and either die in the bone marrow or soon after they go into the blood.
What is MDS and AML?
Myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML) exist along a continuous disease spectrum starting with early-stage MDS, which may progress to advanced MDS, AML, cured AML or resistant AML. The disease is characterized by an overproduction of immature blood cells. The resulting lack of mature, healthy blood cells causes anemia and an increased risk for infection and bleeding. Around 5-10% of patients with solid tumors who are treated with chemotherapy, radiation or autologous stem cell transplantation develop treatment-related MDS or AML. The majority of patients with MDS and AML are not cured with available therapies, underscoring the urgent need for new therapeutic alternatives that will improve the clinical outcomes of these patients.
Can stem cell transplants be used for AML?
Stem cell transplants (SCT) can elicit long-term disease free survival, but this treatment presents risks for the largest subpopulation of AML patients, the elderly. We’re developing cellular therapies that can reduce the risk associated with SCT and, in some cases, even enhance treatment outcomes. We’re also developing cellular therapies, which improve the cancer-killing activity of powerful immune cells called NK cells and T cells, rather than using drugs to treat the cancer directly.
Is MDS an aggressive disease?
MDS/AML is an aggressive disease with few treatment options. Simona Colla, Ph.D. , is leading research efforts of the Moon Shot to better understand and overcome the resistance of MDS to current treatments.
Does nivolumab help with AML?
Immunotherapy drug improves outcomes for AML patients. The immunotherapy drug nivolumab, in combination with standard chemotherapy, more than doubled response rates and improved overall survival in patients with acute myeloid leukemia (AML), according to preliminary findings by researchers at MD Anderson. Learn more.
What is the best treatment for MDS?
Immunotherapy. Immunotherapy, also called biologic therapy, is designed to boost the body's natural defenses to fight MDS. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function. Although this is rarely used for MDS, it may be an option for some patients.
What is standard of care for MDS?
This section explains the types of treatments that are the standard of care for MDS. “Standard of care” means the best treatments known. When making treatment plan decisions, you are encouraged to consider clinical trials as an option. A clinical trial is a research study that tests a new approach to treatment.
What is systemic therapy?
Systemic therapy is the use of medication to destroy unhealthy cells. This type of medication is given through the bloodstream to reach those cells throughout the body. Systemic therapies are generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication, or a hematologist, a doctor who specializes in treating blood disorders.
What is a multidisciplinary team in MDS?
For MDS, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. Your health care team may include a variety of other health care professionals, such as physician assistants, nurses, social workers, pharmacists, counselors, dietitians, and others.
What is clinical trial?
Clinical trials are an option to consider for treatment and care for all stages of cancer. Your doctor can help you consider all your treatment options. To learn more about clinical trials, see the About Clinical Trials and Latest Research sections.
Why do doctors want to do clinical trials?
Doctors want to learn whether the new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option to consider for treatment and care for all stages of cancer.
Can you recover from MDS?
If treatment does not work. Recovery from MDS is not always possible. If the MDS cannot be cured or controlled, the disease may be called advanced or terminal. This diagnosis is stressful, and for many people, advanced MDS is difficult to discuss.
What is MDS in medical terms?
Takeaway. MDS is a severe, chronic syndrome from which very few people successfully recover. It often progresses to AML, which is a form of leukemia. Depending on which scoring system a doctor uses, life expectancy can change, according to the progression of MDS.
What are the factors that affect the outlook of people with MDS?
Treatment for MDS depends on several factors, including the type of MDS, the individual’s age, and other health problems they may have. Those with a low risk of MDS becoming cancer may not need treatment at first.
Can MDS cause leukemia?
Progression to leukemia. About one-third of people with MDS will develop AML, which is cancer of the bone marrow. For this reason, doctors sometimes refer to MDS as preleukemia. People with more advanced MDS have a much higher risk of AML.
Can MDS cause anxiety?
Treating a chronic condition can be expensive, and mounting costs may add to the emotional difficulties that MDS can present. If a condition is tough to treat, it can lead to feelings of depression and anxiety. If these feelings develop during MDS treatment, people can look to possible support networks.
Can cancer treatment be stopped?
The side effects of cancer treatment can be severe. If a treatment is not improving blood cell counts, a person may choose to stop active treatment and focus instead on supportive care. MDS is a chronic disease, and so it is vital to make sure some form of insurance is available.
Can MDS be treated?
For most people, treatment cannot often cure MDS. Typically, there will be periods of intensive treatment with time to rest in between. Treatments may include: Supportive treatment: Options include blood transfusions, drugs to remove excess iron from the blood, growth factor drugs, and antibiotics.
Can bone marrow transplants cure MDS?
Of these options, a bone marrow transplant is the best chance for a person with MDS to cure the condition. However, many older adults are not eligible due to potentially life threatening side effects. The side effects of cancer treatment can be severe.
What is the pathophysiology of MDS/MPN?
The pathophysiology of MDS/MPN involves abnormalities in the regulation of myeloid pathways for cellular proliferation, maturation, and survival. Clinical symptoms are caused by complications resulting from the following: [ 6]
What is MDS/MPN?
The myelodysplastic/myeloproliferative neoplasms (MDS/MPN) are clonal myeloid disorders that possess both dysplastic and proliferative features but are not properly classified as either myelodysplastic syndromes (MDS) or chronic myeloproliferative disorders (CMPD). [ 1] This category is composed of three major myeloid disorders: chronic myelomonocytic leukemia (CMML), juvenile myelomonocytic leukemia (JMML), and atypical chronic myeloid leukemia (aCML). Myeloid disease that shows features of both MDS and CMPD but does not meet the criteria for any of the three major MDS/MPN entities is designated as myelodysplastic/myeloproliferative neoplasm, unclassifiable (MDS/MPN-UC).
What is PDQ cancer?
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of myelodysplastic/ myeloproliferative neoplasms. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions.
What is JMML in children?
JMML (also known as juvenile chronic myelomonocytic leukemia) is a rare hematopoietic malignancy of childhood accounting for 2% of all childhood leukemias. [ 4] . A number of clinical and laboratory features distinguish JMML from adult-type chronic myeloid leukemia, a disease noted only occasionally in children.
What is CMML in medical terms?
The World Health Organization (WHO) classifies chronic myelomonocytic leukemia (CMML) as a myelodysplastic/myeloproliferative neoplasm (MDS/MPN). [ 1] The WHO recognizes a dysplastic subtype and a proliferative subtype, with prognostic groups differentiated by the percentage of blasts in the bone marrow (higher percentage with worse prognosis). [ 2]
How long does hydroxyurea take to cure aCML?
Treatment with hydroxyurea may lead to short-lived partial remissions of 2- to 4-months' duration. [ 4] Atypical CML, appears to respond poorly to treatment with interferon-alpha. [ 4]
Which precursors account for more than 10% of white blood cells?
Neutrophil precursors (e.g., promyelocytes, myelocytes, and metamyelocytes) accounting for more than 10% of white blood cells. Minimal absolute basophilia with basophils accounting for less than 2% of white blood cells. Absolute monocytosis with monocytes typically account for less than 10% of white blood cells.