
Treatment
- Medications. Intense research to identify treatment options for specific types of interstitial lung disease is ongoing.
- Oxygen therapy. You're most likely to receive oxygen when you sleep or exercise, although some people may use it round-the-clock.
- Pulmonary rehabilitation. ...
- Surgery. ...
| Class | Examples |
|---|---|
| Fluoroquinolone | Moxifloxacin, 400 milligrams IV |
| Cephalosporin or penicillin class with β-lactamase inhibitor | Ceftriaxone, 1 gram IV or ampicillin/sulbactam 1.5 gram IV |
| plus | plus |
| Macrolide | Azithromycin, 500 milligrams IV |
How do you treat lung infiltrates?
Lung infiltrates. The term “lung infiltrates” or “pulmonary infiltrate” is considered a context-dependent, non-specific and imprecise descriptive term when used in radiology reports (plain film or CT) 1). From a pathophysiological perspective, the term “infiltrate” refers to “an abnormal substance that accumulates gradually within cells or body ...
What is the prognosis for lung cancer without treatment?
Jan 01, 2021 · How are lung infiltrates treated? Studies estimate that for ICU patients with pulmonary infiltrates 70%-80% do not have pneumonia, but currently most will receive combination broad spectrum empiric antibiotic therapy with duration from 5-14 days.
What is the difference in infiltrate and pneumonia?
Overinflation and infiltrates suggest cystic fibrosis or chronic asthma. A silent chest with infiltrates should arouse suspicion of alveolar proteinosis (see Chapter 434),Pneumocystis jiroveci infection (see Chapter 271), genetic disorders of surfactant synthesis and secretion causing interstitial pneumonitis, or tumors. Growth should be carefully assessed to determine …
What to do after lung cancer treatment?
Nov 12, 2020 · In some cases, your doctor may simply choose to treat you with antibiotics and see if the infiltrate on chest X-ray will disappear when you get another one after a short time. This assumes you have an infection that will clear with antibiotics. If the repeat chest X-ray shows that the infiltrate has not cleared, then that becomes more concerning.
What causes lung infiltrates?
Pulmonary infiltrates commonly occur in the febrile neutropenic patient and have a number of causes, especially in the BMT recipient. These include non-infective conditions such as pulmonary edema, alveolar hemorrhage, adverse drug reactions, radiation injury and the idiopathic pneumonitis syndrome.
How do you treat infiltrates?
These patients are at risk for resistant and recurrent infections, so precise diagnosis and treatment are key. For treatment, I start with broad-spectrum antibiotics. If it is a small infiltrate, I may use gatifloxacin as well as ointment at night, such as an erythromycin ointment.Jan 22, 2021
Can pulmonary infiltrates be cured?
There is no cure for ILD. Once scarring happens in the lungs, it usually cannot be reversed. Treatment can help slow the disease down to preserve as much quality of life as possible. The prognosis for patients depends on how severe the condition is, and the cause of the ILD.Apr 26, 2018
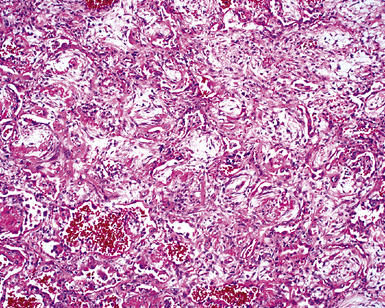
What does infiltrates in the lungs mean?
A pulmonary infiltrate is a substance denser than air, such as pus, blood, or protein, which lingers within the parenchyma of the lungs. Pulmonary infiltrates are associated with pneumonia, tuberculosis, and sarcoidosis.
Is lung infiltrate an infection?
When interpreting the x-ray, the radiologist will look for white spots in the lungs (called infiltrates) that identify an infection. This exam will also help determine if you have any complications related to pneumonia such as abscesses or pleural effusions (fluid surrounding the lungs).
How is sterile infiltrate treated?
Treatment options include cessation of contact lens wear, topical antibiotics and/or topical corticosteroids. Corneal scrapings for stains and cultures should be considered with larger infiltrates complicated with epithelial defect, anterior chamber inflammation and ocular pain.
Can you live a long life with pulmonary fibrosis?
A diagnosis of PF can be very scary. When you do your research, you may see average survival is between three to five years. This number is an average. There are patients who live less than three years after diagnosis, and others who live much longer.Mar 22, 2020
Are there any new treatments for pulmonary fibrosis?
Currently, two drugs are FDA-approved for treatment of idiopathic pulmonary fibrosis (IPF), which is the most common form of PF. These include nintedanib (Ofev®) and pirfenidone (Esbriet®).Mar 22, 2020
Can lung fibrosis be cured?
There is no cure for pulmonary fibrosis. Current treatments are aimed at preventing more lung scarring, relieving symptoms and helping you stay active and healthy.
What does infiltration mean in medical terms?
Infiltration is the movement of cancer cells from their normal location into the surrounding non-cancerous tissue. Another word for infiltration is invasion. Infiltration is an important feature that pathologists look for when trying to decide if a tumour is benign (non-cancerous) or malignant (cancerous).
Does lower lobe infiltrate mean pneumonia?
Answer. Radiographic evidence of aspiration pneumonia depends on the position of the patient when the aspiration occurred. The right lower lung lobe is the most common site of infiltrate formation due to the larger caliber and more vertical orientation of the right mainstem bronchus.Aug 15, 2018
Is infiltrate same as effusion?
Effusions and infiltrates can perhaps be more easily understood using a sponge to represent the lung. In this model, an infiltrate is depicted by the blue coloration that has invaded the sponge itself (sponge on left). An effusion is depicted by the blue fluid upon which the lung is floating (sponge on right).
What percentage of patients die from pulmonary infiltrates?
Pulmonary infiltrates occur in 25% of patients with neutropenia developing after chemotherapy, and up to 5% of patients undergoing hematopoietic stem cell transplantation (HSCT) will die as a result of pneumonia.
What is pulmonary eosinophilia?
Tropical pulmonary eosinophilia consists of myalgia, fatigue, weight loss, and anorexia associated with cough, frequently with nocturnal exacerbations, wheezing, dyspnea, and marked peripheral eosinophilia in patients who have lived in or visited the tropics .
How long does it take for CMV to show up after transplant?
CMV manifests at a median time of 40 to 50 days after the transplantation period (see Fig. 96.1 ).
What is eosinophilic pneumonia?
Pulmonary infiltrates with eosinophilia (PIE), also called eosinophilic pneumonia, is a syndrome associated with a variety of clinical entities, only some of which have an infectious cause.271 Pulmonary eosinophilia with transient, peripheral pulmonary infiltrates and minimal symptoms (Löffler's syndrome) ...
How long did a white woman recover from clarithromycin?
She recovered spontaneously within a few days after drug withdrawal (103 A ).
How long did Henoch-Schönlein purpura last?
Henoch–Schönlein purpura occurred 4 days after a 48-year-old white man started to take clarithromycin 500 mg/day; after a few days clarithromycin was withdrawn and his symptoms quickly resolved (106 A ).
Does clarithromycin interact with digoxin?
Drug interactions. A clinically important interaction between digoxin and clarithromycin has been suggested. Digoxin concentrations increased during concomitant administration of clarithromycin in eight patients, and this effect was related to the dose of clarithromycin .
What is persistent pulmonary infiltrate?
Persistent pulmonary infiltrate results when a substance denser than air (e.g., pus, edema, blood, surfactant, protein, or cells) lingers within the lung parenchyma. Nonresolving and slowly resolving pneumonias are the most common broad categories of persistent pulmonary infiltrate. [1]
What is nonresolving pneumonia?
Nonresolving or slowly resolving pneumonia is loosely defined as a pneumonia that does not improve clinically, or even worsens, despite a minimum of 10 days of adequate antibiotic therapy, or as radiographic infiltrate that does not resolve within 12 weeks. [7]#N#El Solh AA, Aquilina AT, Gunen H, et al. Radiographic resolution of community-acquired bacterial pneumonia in the elderly. J Am Geriatr Soc. 2004 Feb;52 (2):224-9. http://www.ncbi.nlm.nih.gov/pubmed/14728631?tool=bestpractice.com#N#[8]#N#Fein AM, Feinsilver SH, Niederman MS. Nonresolving or slowly resolving pneumonia: diagnosis and management in the elderly patient. Clin Chest Med. 1993 Sep;14 (3):555-69. http://www.ncbi.nlm.nih.gov/pubmed/8222569?tool=bestpractice.com#N#Slowly resolving pneumonias are usually defined as the persistence of radiographic infiltrate in a clinically improved patient for longer than 4 weeks (<50% resolution in 1 month).
What is the treatment for interstitial lung disease?
Many people diagnosed with interstitial lung diseases are initially treated with a corticosteroid (prednisone), sometimes in combination with other drugs that suppress the immune system. Depending on the cause of the interstitial lung disease, this combination may slow or even stabilize disease progression.
How to cope with chronic lung disease?
Your daily routines and activities may need to be adjusted, sometimes radically, as breathing problems worsen or health care needs take priority in your life.
Why do we need a high resolution CT scan?
A high-resolution CT scan can be particularly helpful in determining the extent of lung damage caused by interstitial lung disease. It can show details of the fibrosis, which can be helpful in narrowing down ...
How to diagnose pulmonary fibrosis?
Lung tissue analysis. Often, pulmonary fibrosis can be definitively diagnosed only by examining a small amount of lung tissue (biopsy) in a laboratory. The tissue sample may be obtained in one of these ways: Bronchoscopy.
What is the goal of pulmonary rehabilitation?
The aim of pulmonary rehabilitation is not only to improve daily functioning but also to help people with intersitial lung disease live full, satisfying lives. To that end, pulmonary rehabilitation programs focus on: Physical exercise, to improve your endurance. Breathing techniques that improve lung efficiency.
How to help someone with a disease?
Talking openly may help you and your loved ones cope with the emotional challenges of your disease. In addition, clear communication will help you and your family plan effectively for your needs if your disease progresses.
What is the purpose of echocardiogram?
Echocardiogram. A sonogram for the heart, an echocardiogram uses sound waves to visualize the heart. It can produce still images of your heart's structures, as well as videos that show how your heart is functioning. This test can evaluate the amount of pressure occurring in the right side of your heart.
What causes fluid build up in the lung?
Pulmonary edema. Pulmonary edema is the buildup of fluid in the lung tissue and alveoli due to the increased pressure inside the capillaries which results to leakage. The condition is often triggered by heart disease, heart failure, hypertension and kidney failure. It can also develop from inhalation of toxic gases and shock.
What causes infiltration of the air sacs?
There are various causes of lung infiltration. Certain lung ailments such as silicosis, pneumonia, cystic fibrosis and asbestosis often cause the air sacs to be filled with fluids made of cancer cells, white blood cells, pus, blood or proteins which are called as infiltrates.
What causes pneumonia in the lungs?
Various bacteria can result to pneumonia. The usual cause of bacterial pneumonia is streptococcus pneumoniae. This is a bacterial infection that is not limited to the lung but also involve other body parts. The lungs are significantly inflamed which results to varying degrees of irreversible damage despite treatment.
What are the symptoms of a pleural symtom?
The initial symptoms include coughing with mucus and fever. The buildup of pus in the pleural space or empyema also occurs.
What is acute respiratory distress syndrome?
Acute respiratory distress syndrome is a non-specific disease linked to severe pneumonia, sepsis, shock and trauma. The condition often necessities immediate medical care due to respiratory insufficiency. The airs sacs are filled with fluid from the infection.
Why do I have chest pain and shortness of breath?
Chest pain, coughing and shortness of breath soon arise as the alveoli become inflamed from the infection. The scattered infiltrates show a significant influx of white blood cells that attack the invading bacteria, generating pus.
