What drug is used to reverse the effects of heparin?
- Black, tarry stools
- bleeding gums
- blood in the urine or stools
- pain in the chest, groin, or legs, especially calves of legs
- pinpoint red spots on the skin
- severe headaches of sudden onset
- sudden loss of coordination
- sudden shortness of breath for no apparent reason
- sudden slurred speech
- sudden vision changes
What happens if you overdose on heparin?
What will happen if there is high heparin in the blood? 1. Bleeding due to overdose is the most serious complication of heparin therapy. Haematuria is generally the first sign. With proper monitoring, serious bleeding occurs only in 1–3% patients. 2. Thrombocytopenia is another common problem.
When should I stop heparin before surgery?
- Stop Warfarin 4-5 days before surgery
- Allow INR to decrease
- Start Anticoagulation 2 days before surgery Low dose Heparin 5000 U SC or Low Molecular Weight Heparin at prophylactic doses
- Restart low dose Heparin or LMWH postoperatively (hold for 24-48 hours postoperatively)
- Restart Warfarin immediately postoperatively
What is the antidote for heparin overdose?
- Nosebleeds
- Vomit that looks like it contains coffee grounds
- Bowel movements that are black and tarry
- Bright red blood in stools or vomit
- Blood in the urine
- Excessive or unexplained bruising
- Petechiae (a spattering of red or brown dots on the skin or whites of the eyes caused by the bursting of underlying blood vessels)

What is the antidote or antagonist for heparin overdose?
A heparin antagonist used for heparin overdose is protamin, a mixture of proteins that are isolated from fish sperm. Upon reaction, it inactivates heparin by forming an insoluble complex.
Is vitamin K an antidote for heparin?
Abstract. Individuals anticoagulated with warfarin or heparin are typically treated with specific antidotes such as vitamin K or protamine, respectively, if they bleed or require surgery.
What is the reversal for heparin?
Background Protamine is used to reverse the anticoagulant effects of heparin, but it can have important side effects. Platelet factor 4 (PF4) is a protein found in platelet alpha granules that binds to and thereby neutralizes heparin.
Which medication is used to reverse bleeding associated with heparin?
Protamine sulfate reverses the effect of unfractionated heparin completely and of low-molecular-weight heparin (LMWH) partially.
How do you reverse over anticoagulation?
Probably the most important intervention to reverse warfarin is vitamin K. 10 mg should be given intravenously, as soon as possible (infused over 30 minutes). FFP or PCC will work only for ~8 hours. Vitamin K will do the job after the FFP/PCC wears off.
What is the treatment for a heparin overdose?
Sulfate of protamine When it is essential to reverse the anticoagulant action of heparin or to treat heparin overdose, a blood factor is utilized....
How do you inactivate heparin?
To counteract the anticoagulant action of heparin, protamine sulfate was administered (1 mg per 100 units of heparin that has been given over the p...
Is protamine sulfate the antidote for heparin?
Heparin's anticoagulant effects can be quickly reversed by intravenous protamine sulfate. Protamine sulfate is a basic protein produced from fish s...
Which drug reverses the effect of heparin?
Protamine is a drug that is used to counteract and neutralize heparin's anticoagulant effects. Protamine was originally extracted from fish skin bu...
Which drug is an anticoagulant antagonist used to reverse the effects of heparin?
The particular antagonist that counteracts heparin-induced anticoagulation is protamine. When given in sufficient dose, it will restore normal clot...
What do you give to reverse heparin?
Protamine sulfate, a fish sperm product, is often used to reverse the anticoagulant effects of unfractionated heparin (UFH) and low-molecular weigh...
Drugs used to treat Heparin Overdose
The following list of medications are in some way related to, or used in the treatment of this condition.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Is heparin flushed?
From the smallest doses associated with heparin flushes to the largest doses associated with therapeutic uses, familiarity with heparin has led to a faded perception of the risks associated with its use and misuse. Those familiar with the drug may forget that even a slight mistake can lead to patient harm.
Is heparin a high alert drug?
Thus, attention is needed to enhance staff perception of the risks associated with heparin, and to remind staff that heparin is a high-alert drug—regard less of the concentration or dose—and that safeguards must always be employed.
How it works
Heparin belongs to a class of drugs called anticoagulants. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Serious side effects
Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency. Serious side effects and their symptoms can include the following:
Interactions that can increase your risk of side effects
Taking heparin with certain drugs can increase your risk of bleeding and make you bruise more easily. Examples of these drugs include:
Interactions that can make heparin less effective
When used with heparin, certain drugs can make heparin less effective. Examples of these drugs include:
Warnings for people with certain health conditions
For people with pig protein sensitivity: Do not take this drug. This drug is made from pork tissue and can cause a life-threatening allergic reaction in people who are sensitive or allergic to other pig proteins.
Warnings for other groups
For pregnant women: Research in animals has shown negative effects to the fetus when the mother uses heparin. However, there haven’t been enough studies done in humans to be certain how the drug might affect the fetus.
Dosage for deep vein thrombosis and pulmonary embolism
Typical starting dosage: 333 units/kg of body weight injected under your skin.
Why is heparin used in IV?
It is also used before surgery to reduce the risk of blood clots. Do not use heparin injection to flush (clean out) an intravenous (IV) catheter. A separate product is available to use as catheter lock flush.
What are the side effects of heparin?
fever, chills, runny nose, or watery eyes; easy bruising, unusual bleeding, purple or red spots under your skin; or. signs of a blood clot - sudden numbness or weakness, problems with vision or speech, swelling or redness in an arm or leg. Common heparin side effects may include: unusual bleeding or bruising;
What is the FDA number for heparin?
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. Heparin side effects (more detail)
What to do if you have a blood clot?
You will need frequent tests to measure your blood-clotting time. Call your doctor or seek emergency medical attention if you have unusual bleeding or bruising, severe stomach or back pain, unusual tiredness, a nosebleed, blood in your urine or stools, coughing up blood, or any bleeding that will not stop.
Can you take heparin with blood thinners?
Keep it out of the reach of children and pets. You may be switched from injectable heparin to an oral (taken by mouth) blood thinner. Do not stop using the injection until your doctor tells you to. You may need to use both the injection and the oral forms for a short time.
Can heparin harm an unborn baby?
if you are having a menstrual period. It is not known whether heparin will harm an unborn baby.
Can you take heparin if you are allergic to pork?
Before taking this medicine. You should not use this medicine if you are allergic to heparin or pork products, or if you have: a history of low platelets in your blood caused by using heparin or pentosan polysulfate; a severe lack of platelets in your blood; or. uncontrolled bleeding.
What are the risk factors for heparin?
Heparin-related risk factors include type of heparin and duration of exposure. Low molecular weight heparin (LMWH) is associated with a 5- to 10-fold lower risk of HIT than unfractionated heparin (UFH) 7, 8 but accounts for a growing proportion of cases because of its increasing use.
How long does it take for a platelet count to drop after heparin?
In heparin-naive patients, HIT classically presents with a platelet count fall beginning 5 to 14 days after initial exposure while drug is still present. 23 Rapid-onset HIT, in which the platelet count drops within hours of heparin administration, may occur in patients with preexisting anti-PF4/heparin antibodies.
What are the drawbacks of parenteral anticoagulants?
First, management is complex, cumbersome, and prone to error. Approved agents require continuous intravenous infusion, serial monitoring, and frequent dose adjustments. Indeed, these drugs are sufficiently complex that many institutions have reassigned primary responsibility for their management to dedicated pharmacist-directed anticoagulation services. 89 Desirudin and fondaparinux offer hope of reducing therapeutic complexity. Neither appears to require routine laboratory monitoring or dose adjustment. Both are administered subcutaneously and have negligible effect on the International Normalized Ratio (INR), thereby facilitating transition to outpatient therapy. In theory, new oral inhibitors of thrombin and FXa constitute rational therapies for HIT and also offer the promise of simplifying management. Dabigatran, apixaban, and rivaroxaban do not induce platelet aggregation or PF4 release in the presence of HIT-positive sera in vitro 90 and warrant further investigation, although no published clinical data are available to support their use.
What is desirudin used for?
Desirudin is a subcutaneously administered, renally cleared DTI licensed for thromboprophylaxis after hip arthroplast y. In the open-label PREVENT-HIT trial, the only prospective head-to-head comparison of DTIs, patients were randomized to receive argatroban or fixed-dose desirudin. Although the study closed because of poor accrual after only 16 subjects had been randomized, results were promising with no new thrombotic events or major bleeding among the 8 desirudin-treated subjects. Moreover, cost per treatment course was substantially lower in the desirudin arm ($1688 vs $8250). 80 More data are needed to define the role of this promising agent.
What percentage of platelets fall after heparin?
Percentage fall is measured from peak platelet count after heparin exposure to its nadir. A 50% or greater reduction occurs in the large majority of patients, although approximately 10% evince a more modest decline of 30% to 50%. 26
What is heparin induced thrombocytopenia?
Heparin-induced thrombocytopenia (HIT), formerly HIT type II, is a prothrombotic and potentially lethal disorder caused by platelet, endothelial, and monocyte-activating antibodies that target multimolecular complexes of platelet factor 4 (PF4) and heparin. 1 Although HIT was first described more than 50 years ago, 2 not until the 1990s was the target antigen identified, the now widely used anti-PF4/heparin ELISA developed, 1 and the first effective therapies approved. Since that time, a major emphasis of training and contemporary literature has been early disease recognition and prompt initiation of therapy. 3, 4
What are the two types of tests that are used to determine if a patient has heparin-dependent
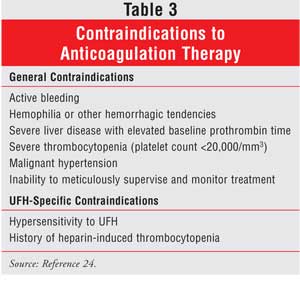
Because of the challenges of clinical diagnosis, physicians rely heavily on laboratory testing. Standard tests fall into 2 categories: functional assays , which detect patient antibodies that induce heparin-dependent platelet activation; and immunologic assays , which identify circulating anti-PF4/heparin antibodies, irrespective of their capacity to activate platelets ( Table 3 ).
