Explore
9 rows · Warm compresses are preferred for extravasation of specific drugs including vinca alkaloids, ...
Which drugs cause extravasation?
Jun 29, 2021 · As soon a doctor or nurse suspects extravasation, they will : Stop the infusion and leave the cannula in place. Remove as much of the drug as possible using a 10–20-milliliter syringe (connected to...
What to do for extravasation?
At the first sign of extravasation, nursing intervention with following steps is recommended: stop administration of IV fluids immediately, disconnect the IV tube from the cannula, aspirate any remaining drug from the cannula, administer drug-specific antidote, and notify the physician.
How to prevent extravasation?
Apr 04, 2022 · Treatment options dexrazoxane Vitrase Hylenex Amphadase Hydase
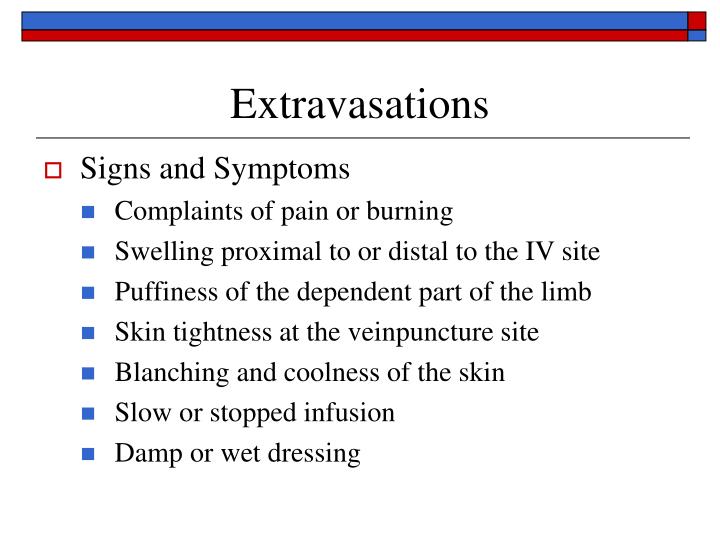
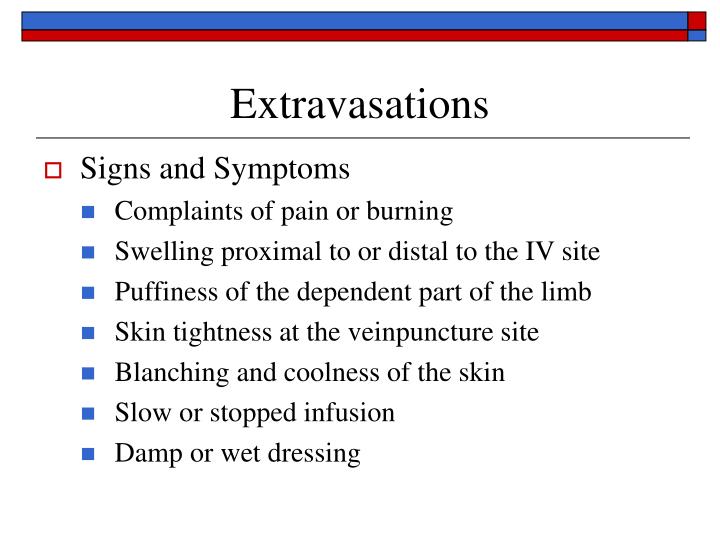
What are the signs of extravasation?
Mix 4 mL of sodium thiosulfate 10% with 6 mL sterile water for injection to prepare a 0.17 mol/L (4%) solution. Inject 3-10 mL subcutaneously into extravasation site; use clinical judgment and size of extravasation site to determine volume. This dosing is based on limited and varied information. Dexrazoxane 9
What is extravasation in a vein?
Extravasation is defined as the leakage or inadvertent administration of a vesicant drug or solution from a vein into the extravascular space. 1 Infiltration, often used in reference to extravasation, refers to leakage of a non-vesicant drug or solution. 2,3 Initial symptoms of extravasation are similar to infiltration and include persistent pain, burning, stinging, swelling, and either blanching or erythema at the site of injection or along the course of the vein. However, vesicants are differentiated from non-vesicants in that they can cause tissue necrosis, blistering, and ulceration. Damage from extravasation can progress to a significant degree, causing permanent disability and disfigurement, and necessitating surgical debridement or skin grafting. 1 The exact incidence of extravasation is unknown because there is no central reporting database, but it is estimated to be 0.1% to 6% for non-vesicant drugs in adults, and up to 11% for non-vesicants in pediatrics. For vesicant drugs and chemotherapeutic agents, the incidence has been reported to range from 0.01% to 6%. 2
What is the best approach to extravasation injury?
3-6 Preventive measures include appropriate dilution of medication, infusion of medication via the appropriate rate of administration , ensuring patency of the vascular access device, careful monitoring of infusions during administration, use of clear tape or dressings to allow for visual inspection of the infusion site, and immobilization of the extremity with the IV cannula.
What is non-cytotoxic management?
Management of extravasation of non-cytotoxic drugs. The management of non-cytotoxic drugs is largely supportive and non-pharmacological, except where antidotes exist, such as for vasopressors. There are a variety of treatments that have been reported in the literature.
What are the risk factors for extravasation?
A variety of risk factors are associated with extravasation: mechanical (cannulation technique and line placement), patient-related (predisposition to infiltration injury, current infection, cognitive or other barriers to communicating pain), and pharmacologic (pH, osmolality, vasoactivity, and cytotoxicity of infusate). 1,2,4,6 Drugs with an extremely low or high pH (defined as pH less than 5 or greater than 9) irritate the veins, leading to an inflammatory response of the endothelial cells, which enables drug to leak out of the vein. Osmolality is also a consideration, as differences in osmotic pressure can damage endothelial cells, leading to potential for drug leakage from vessels. Certain drugs cause vasospasms, which result in back pressure at the intravenous (IV) site and may expand the puncture site in the vein, allowing leakage to occur; drugs that act as vasoconstrictors can also cause tissue ischemia. Some drugs, including anti-cancer agents, are directly cytotoxic to cells. Cytotoxic agents can be further subdivided into DNA-binding and non–DNA-binding agents. Additionally, administration factors, including the experience of personnel administering the injection, the injection technique, and the number of venipuncture attempts to establish a line, contribute to the risk of extravasation, as does the fragility of the patient’s veins.
Can drugs cause tissue ischemia?
Certain drugs cause vasospasms, which result in back pressure at the intravenous (IV) site and may expand the puncture site in the vein, allowing leakage to occur; drugs that act as vasoconstrictors can also cause tissue ischemia. Some drugs, including anti-cancer agents, are directly cytotoxic to cells.
What happens when a vesicant leaks out of the vein and into the surrounding tissue?
Extravasation occurs when a vesicant drug leaks out of the vein and into the surrounding tissue. When this happens, a person will likely experience serious tissue damage, including ulceration and tissue death, if they do not receive treatment in time.
Why does extravasation decrease?
However, improvements in infusion techniques and a higher awareness among healthcare professionals of the early signs of extravasation are causing the rate to decrease. Extravasation has many possible causes, including: repeatedly using the same veins for cannulation. fragile veins.
What is the difference between extravasation and infiltration?
The difference between extravasation and infiltration is the type of solution that leaks into nearby tissue. Vesicant drugs are those that can cause tissue death, whereas non-vesicant drugs do not have this effect.
What happens when you take a venous cannula?
When a healthcare professional administers a drug through a venous cannula, there is a small risk of the solution leaking out of the veins and into the surrounding tissue. If the medication is a vesicant drug — meaning that it has the potential to cause tissue damage through blistering and ulceration — doctors call this complication extravasation. ...
What is grade one pain?
Grade one. Grade one is a mild case of extravasation, and the symptoms include: discomfort or pain around the needle site. medication not passing through the cannula as easily. a minimal amount of swelling without skin discoloration.
What are the symptoms of extravasation?
The symptoms of extravasation include a painful stinging or burning sensation, swelling, and skin discoloration. Read on to learn more about extravasation, its causes, and how doctors treat it.
How to diagnose extravasation?
Doctors diagnose extravasation by examining and inspecting the skin area around the cannula. If they suspect extravasation, they will stop the drug infusion and elevate the limb. Doing this as soon as possible should prevent serious complications from developing and stop the extravasation from escalating to a higher grade.
What is the management of extravasation?
Management of extravasation includes nursing intervention and thermal application.
How to stop IV fluid extravasation?
At the first sign of extravasation, nursing intervention with following steps is recommended: stop administration of IV fluids immediately, disconnect the IV tube from the cannula, aspirate any remaining drug from the cannula, administer drug-specific antidote, and notify the physician.
What is extravasation in IV?
Extravasation is when fluid leaks out of your vein and into the soft tissue around an IV. The fluid is a vesicant medicine. This means that it can cause tissue damage, blisters, or severe tissue loss. Some examples of vesicant medicines include chemo medicines, contrast liquid, certain antibiotics, and seizure medicine.
How to keep limb elevated?
Prop your limb on pillows or blankets to keep it elevated comfortably . Ask how to clean the area. Your healthcare provider may bandage the area. He or she may tell you which products you can apply on the area, such as a mild soap. Medicine may help relieve pain or inflammation: Acetaminophen decreases pain and fever.
How to reduce swelling in a swollen ear?
Ice helps prevent tissue damage and decreases swelling and pain. Continue to apply heat on the area as directed or for 20 to 30 minutes every 2 hours. Heat helps decrease pain and muscle spasms. Continue to elevate the area above the level of your heart as often as you can. This will help decrease swelling and pain.
Can acetaminophen cause liver damage?
Acetaminophen can cause liver damage if not taken correctly. Do not use more than 4 grams (4,000 milligrams) total of acetaminophen in one day. NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order.
Can NSAIDs cause kidney problems?
This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
Can IV catheters move?
The IV catheter may push through the side of your vein. The IV catheter may move from where it is inserted. Fluid may leak through the area where the catheter enters the vein. The vein may be fragile and may tear with the IV fluid. Fluid may leak through the side of your vein.
Does acetaminophen help with fever?
Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist.
What is the degree of cellular injury determined by?
With extravasation injuries, the degree of cellular injury is determined by the volume of the infiltrating solution and physicochemical characteristics, such as pH, osmolarity, and degree of dissociability (pKa).
What are the complications of a peripheral venous catheter?
Complications of peripheral venous catheters include thrombophlebitis, infection, and extravasation injuries . Thrombophlebitis from peripheral venous catheters is a relatively uncommon complication, probably because the average dwell time for such devices is relatively short.
Why do surgeons recommend early aggressive debridement?
On the other hand, with full-thickness skin necrosis, ulcer, or persistent pain, many surgeons suggest early aggressive debridement because the chronicity and the nature of the wound can cause patients to suffer delayed treatment of primary disease (i.e., carcinoma) and morphofunctional damage [13, 45, 46].
Why are intravascular lines important?
These intravascular lines are crucial in resuscitation, allow vital medication to be administered, and can be used to monitor the patients' real-time vital parameters. There is, however, growing recognition of potential risks to life and limb associated with their use.
Is extravasation rare?
Incidence. Extravasation is not as rare as many people think , and it may occur even in the most closely monitored situations. A study which investigated extravasation over a five-week period in a UK hospital established an incidence of 39% in adults, almost double that of previously published reports [2].
Does calcium chloride cause skin necrosis?
Calcium chloride, for example, has caused full-thickness skin necrosis, and hypertonic saline is the most common sclerosant associated with necrosis. Parenteral nutrition extravasation is reported more often in children [18] and can cause skin sloughs [10] and limb contractures particularly in premature infants.
Does vincristine cause blisters?
vincristine, vinblastine, mitomycin, paclitaxel, azathioprine, acyclovir. are vesicant (i.e., produce blisters) [7, 9], and as well as causing immediate injury may also bind to tissue DNA [30] so that the drug is continually released from dying to healthy cells, resulting in a slow increase in ulcer size over time.
What is prompt intervention?
Immediate treatment measures include a prompt intervention when the extravasation is suspected. Leakage of bodily fluids and drugs may also take place due to other reasons as well like infiltration. As such, extravasation and infiltration are two different occurrences.
How long does extravasation last?
Shoulder pain. The late effects of extravasation are: Marked induration that may last between days to months.
What is extravasation in cancer?
Extravasation is a process through which a liquid, maybe a drug or a fluid leak into a surrounding tissue accidentally. In case of inflammation, it indicates white blood cells (WBC) movements from capillaries to tissues, also called diapedesis. In malignant cancer metastasis, the term is used to mean involuntary permeation ...
How to prevent extravasation?
Prevention of Extravasation. Most of the extravasations may be prevented using the systematic implementation and careful I.V administration techniques. Chemotherapy must be given by the trained personnel and during the infusion process, the patient must be observed thoroughly.
What causes a burning sensation in the cannula?
Another differential diagnosis of this condition is chemical phlebitis. This is the inflammation of the veins followed by thrombosis of veins, which causes a burning sensation at cannula. Chemical phlebitis is caused by many drugs.
What is the diagnosis of extravasation?
Diagnosis of Extravasation. Patients must be told to report to the physician regarding any changes in symptoms or sensation at the time of administration of any drug and also to intimate the healthcare professional regarding the early signs of this medical condition.
Can phlebitis cause irritants?
An irritant reaction happens as temporary phlebitis. However, the extravasation of the vesicant drugs like the anthracyclines can cause reactions that can include damage to the progressive tissue, which may progress during the days and the weeks.