What is the treatment for embryonal tumors?
· Options include: Surgery to relieve fluid buildup in the brain. Some embryonal tumors may grow to block the flow of cerebrospinal fluid,... Surgery to remove the tumor. A pediatric brain surgeon (neurosurgeon) removes as much of the tumor as possible, taking... Radiation therapy. A pediatric ...
How is embryonal carcinoma of the testis treated?
· A biopsy can be taken to get a closer look at the cells in the growth to determine what is causing the abnormality and to stage the cancer. If the cancer is an embryonal carcinoma, treatment options can include surgery, chemotherapy, and radiation.
What is embryonal carcinoma?
While standard treatment for patients with advanced embryonal carcinoma is total abdominal hysterectomy, bilateral salpingo-oophorectomy, and limited debulking, young patients can be treated by unilateral salpingo-oophorectomy and limited debulking if the contralateral ovary and uterus are uninvolved.

Is embryonal cell carcinoma curable?
At present, patients with completely resected embryonal carcinoma are treated with postoperative cisplatin-based adjuvant chemotherapy with nearly complete success. Many patients with residual or recurrent tumors can be cured with combination chemotherapy.
Is embryonal carcinoma cancerous?
1 Embryonal Carcinoma. Embryonal carcinoma is the second most common testicular malignancy and, in its pure form, accounts for 15 to 30% of nonseminomatous germ cell tumors. It occurs most commonly in the second decade of life and is rare after the fifth decade. It is not found in infants or children.
Is embryonal carcinoma aggressive?
Embryonal carcinoma: present in about 40 percent of tumors and among the most rapidly growing and potentially aggressive tumor types.
Is embryonal carcinoma painful?
However, it is present as a component of almost ninety percent of mixed nonseminomatous germ cell tumours. The average age at diagnosis is 31 years, and typically presents as a testicular lump which may be painful.
What causes embryonal carcinoma?
The most accepted theory on the development of germ cell tumors involves an initiating event that causes fetal gonocytes to undergo abnormal cell division. As with other germ cell tumors, with the exception of spermatocytic seminoma, embryonal carcinomas are believed to originate from intratubular malignant germ cells.
How does embryonal carcinoma occur?
Cellular origin. Embryonal carcinomas arise from gonadal or extragonadal germ cells, i.e. pluripotent stem cells. Some authors consider these neoplasms to be a transitional step in teratoma development.
What is embryonal carcinoma of the ovary?
Embryonal carcinomas are one of the most malignant cancers arising in the ovary. With an age-adjusted incidence of 0.014 per 100,000 woman-years,6 they represent only 4% of all malignant ovarian germ cell tumors. They are a relatively undifferentiated product of the primordial germ cell.
Is embryonal carcinoma genetic?
Embryonal carcinoma was found to have a six-gene signature which was detected in 3 of 5 studies and included DNMT3B, DPPA4, GAL, GPC4, POU5F1, and TERF1. All six genes play important roles in embryonic development and pluri-potency, which is the evidence that embryonic carcinoma resembles inner cell mass.
What does embryonal mean?
Definitions of embryonal. adjective. of an organism prior to birth or hatching. synonyms: embryologic, embryonic immature. not yet mature.
What is embryonal sarcoma?
Undifferentiated embryonal sarcoma of the liver (UESL) is a rare form of liver cancer that occurs mainly in children, usually between ages 5 and 10, but also well into adolescence. It is the third most common type of primary liver cancer in kids, after hepatoblastoma and hepatocellular carcinoma.
Is Stage 4 germ cell tumor curable?
The cure rate for a stage IV tumor is 82%. Learn more about the stages of germ cell tumors. It is important to remember that statistics on the survival rates for children and teens with a germ cell tumor are an estimate.
Does germ cell tumors come back?
One goal of follow-up care is to check for a recurrence, which means that the tumor has come back. A tumor recurs because small areas of tumor cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms.
What is embryonal carcinoma of the ovary?
Embryonal carcinomas are one of the most malignant cancers arising in the ovary. With an age-adjusted incidence of 0.014 per 100,000 woman-years,6 they represent only 4% of all malignant ovarian germ cell tumors. They are a relatively undifferentiated product of the primordial germ cell.
What is embryonal tumor?
(em-BRY-uh-nul TOO-mer) A mass of rapidly growing cells that begins in embryonic (fetal) tissue. Embryonal tumors may be benign or malignant, and include neuroblastomas and Wilms tumors. Also called embryoma.
Is embryonal carcinoma genetic?
Embryonal carcinoma was found to have a six-gene signature which was detected in 3 of 5 studies and included DNMT3B, DPPA4, GAL, GPC4, POU5F1, and TERF1. All six genes play important roles in embryonic development and pluri-potency, which is the evidence that embryonic carcinoma resembles inner cell mass.
What is embryonal sarcoma?
Undifferentiated embryonal sarcoma of the liver (UESL) is a rare form of liver cancer that occurs mainly in children, usually between ages 5 and 10, but also well into adolescence. It is the third most common type of primary liver cancer in kids, after hepatoblastoma and hepatocellular carcinoma.
What is an embryonal carcinoma?
An embryonal carcinoma is a malignant growth which develops in germ cells. These types of cancers can be seen in men, women, and children, and they take a number of forms. If caught early, the prognosis for someone with an embryonal carcinoma can be very good, as these cancers generally respond well to chemotherapy and radiation.
Who confirms embryonal carcinoma?
A diagnosis of embryonal carcinoma is typically confirmed by a pathologist who is familiar with oncology.
Why is biopsies important?
This is important for treatment, as it may determine which treatments are most appropriate, and it can be used to identify areas of the body which require monitoring. If, for example, embryonal carinoma has spread to the lungs, it can complicate treatment, recovery, and the prognosis.
What is the term for testicular cancer?
If the cancer is allowed to grow, it can spread to other regions of the body. The equivalent cancer in women is known as a dysgerminoma . Other forms of embyonal carcinomas can include teratomas, choriocarcinomas, and yolk sac or endodermal sinus carcinomas, with these last being more common in young children.
What are malignant growths?
These malignant growths develop when germ cells run wild. These cells are rather unique and specialized, designed to produce the gametes used in reproduction. When they start to behave erratically, they can form growths which may contain several layers of different kinds of cells, most notably in the case of a teratoma, which can include things like hair, cartilage, and parts of anatomical structures.
Is embryonal carcinoma more common in children?
Certain forms of embryonal carcinoma will be more common in children.
Does chemotherapy cause hair loss?
Chemotherapy treatment may cause hair loss in some patients.
What is an embryonal tumor?
Embryonal carcinoma is a relatively common testicular germ cell tumor after puberty; 10% are pure embryonal tumors, and a substantial number of tumors will have a mixed embryonal component.29 This tumor demonstrates distinctive sheets, glands, and papillary structures composed of primitive epithelial cells with crowded pleomorphic nuclei. In poorly differentiated tumors, positive immunostains for CD30 and OCT3 with a c-KIT–negative profile are helpful in confirming an embryonal carcinoma. 32 Embryonal carcinoma is treated with orchiectomy. Tumors composed of more than 80% embryonal cell carcinoma or with elevated preoperative AFP (>10,000 mg/mL), vessel invasion in the primary tumor, and tumors of stage T2 or greater are considered high risk and are treated with postoperative chemotherapy and close follow-up. 34
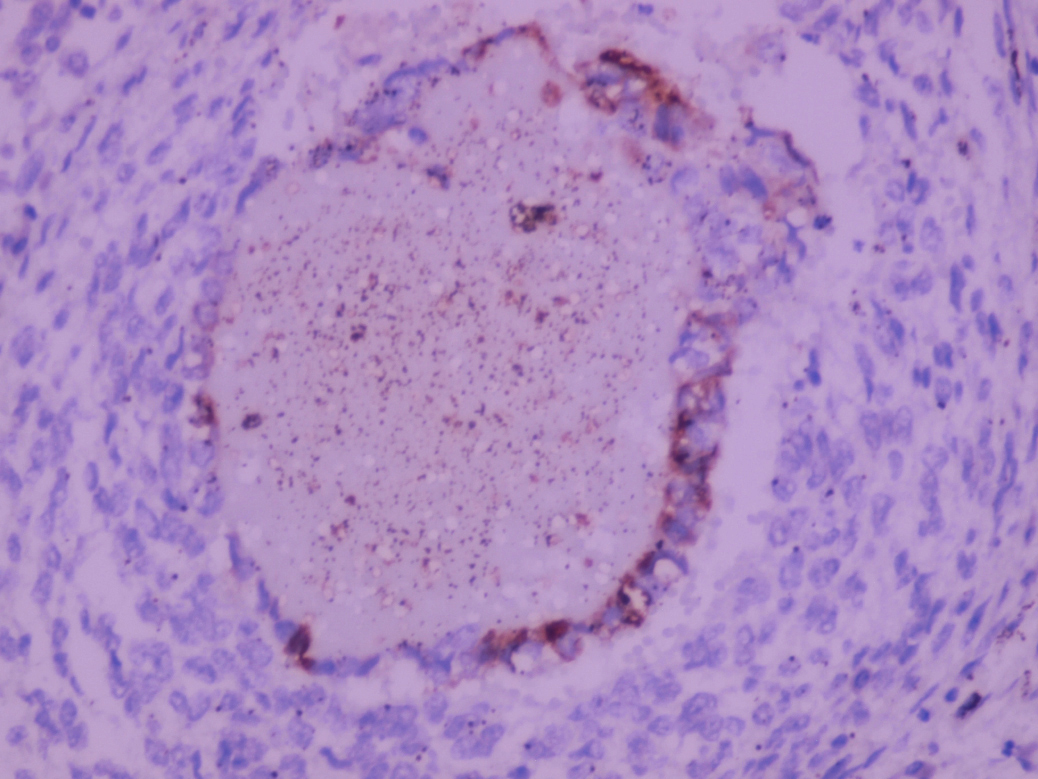
What are the features of embryonal carcinoma?
A common feature of embryonal carcinoma is the presence of extensive areas of necrosis . Note the transition areas with tumor cells . Embryonal carcinoma may also show extensive areas of hemorrhage , which, in some cases, may obscure the nature of the neoplasm.
What is the age of ovarian carcinoma?
Embryonal carcinoma occurs in the ovary less commonly than in the testis, accounting for 4% of malignant ovarian tumors.200,202 The median age at diagnosis is 14 years , somewhat younger than for ovarian yolk sac tumor. Ovarian embryonal carcinoma is more frequently associated with β-hCG production and with hormonal manifestations such as precocious puberty, amenorrhea, and hirsutism. 200 Because of the totipotent nature of embryonal carcinoma cells, differentiation into various histologies may be seen, including teratomas and syncytiotrophoblastic giant cells resembling choriocarcinoma. Polyembryoma is a rare tumor in which multiple embryoid bodies resembling presomite-stage embryos are seen. Polyembryoma is considered by some to be an organoid variant of embryonal carcinoma, 167 although others have described it as one component of mixed germ cell tumors. 256,257
What are EC cells?
Embryonal carcinoma (EC) cells are historically the first pluripotent stem cells derived from mouse embryonic or fetal tissues. EC cells are self-renewing undifferentiated cells derived from teratocarcinomas—malignant tumors containing undifferentiated cells mixed with various differentiated tissues of the three primary germ layers. Teratocarcinomas, first observed in some strains of mice as naturally gonadal developing tumors, arise from pre-implantation/pre-gastrulating embryos or primordial germ cells (PGCs) that had been ectopically grafted in vivo. EC cells can re-form teratocarcinomas in vivo and differentiate in vitro when cultured in suspension. They provide a suitable model system to study cellular commitment and differentiation, but have a major disadvantage: EC cells are tumor cells and consequently they are typically aneuploid. Although they could integrate into a developing embryo and contribute to adult tissues, their contribution was extremely poor and lacked consistency and reproducibility. Most importantly, EC cell contribution to the germline was shown to be a very rare event.
Is embryonal carcinoma a germ cell tumor?
Embryonal carcinoma may be confused with other germ cell tumors, particularly dysgerminoma and yolk sac tumor. Distinction from dysgerminoma is important due to differences in prognosis and treatment. The solid pattern of embryonal carcinoma may mimic dysgerminoma; however, the cells in embryonal carcinoma are more primitive, with higher mitotic rate, greater degree of nuclear irregularity, and less distinct cytoplasmic borders. In contrast, dysgerminoma contains a variable amount of fibrous stroma with striking lymphocytic and granulomatous infiltrate, features typically absent in embryonal carcinoma. Cytokeratin is strongly and diffusely positive in embryonal carcinoma whereas it is negative or only shows weak and focal positivity in dysgerminoma. Embryonal carcinoma lacks the distinctive patterns of yolk sac tumor displaying a more prominent necrotic background as well as cellular pleomorphism and often show more amphophilic cytoplasm. Helpful immunohistochemical stains include CD30 and OCT4, typically positive in embryonal carcinoma but negative in yolk sac tumor. Lastly, these tumors can be confused with surface epithelial carcinomas, either large cell carcinomas or poorly differentiated adenocarcinomas. The latter generally occur in an older age group and generally show neither AFP nor β-hCG production. In contrast to embryonal carcinoma, they are positive for EMA.
Is a yolk sac tumor a mixed germ cell tumor?
Embryonal carcinoma also affects young patients but is far less common than yolk sac tumor in the ovary and, when encountered, is always a component of a mixed germ cell tumor. Embryonal carcinoma lacks many characteristics observed in yolk sac tumor, such as reticular and microcystic patterns, Schiller-Duval bodies, and hyaline bodies, but shares the solid, papillary, and glandular growths. Embryonal carcinoma cells tend to be larger, with a more granular (rather than clear) cytoplasm and nuclei that are even more pleomorphic. However, some yolk sac tumors show more nuclear atypia than usual; therefore, cytologic features cannot be completely relied on. Immunostains are very helpful in the identification of embryonal carcinoma foci in mixed germ cell tumors and in the distinction from yolk sac tumor. OCT4 is negative in yolk sac tumor and positive in embryonal carcinoma and is the best discriminatory stain. GPC3 is positive in yolk sac tumor but can also be positive in foci of yolk sac differentiation of embryonal carcinoma; therefore, it should be used in conjunction with OCT4, which if positive should lead to the diagnosis of embryonal carcinoma.220 Contrary to yolk sac tumor, embryonal carcinoma is positive for CD30, which is yet another helpful immunostain in this context. Immunohistochemical expression of SOX2 is only observed in 50% of ovarian embryonal carcinomas and therefore is not recommended for the detection of embryonal carcinoma foci in mixed germ cell tumors of the ovary. 220 Like yolk sac tumor, embryonal carcinoma is positive for keratins and SALL4.
Does embryonal carcinoma have necrosis?
In some cases, embryonal carcinoma may not show areas of necrosis but rather an inflammatory reaction composed mainly of lymphocytes and plasma cells . Sign in to download full-size image. Extensive Necrosis. A common feature of embryonal carcinoma is the presence of extensive areas of necrosis .
How good is the prognosis for Embryonal Carcinoma of the Testis?
The prognosis of Embryonal Carcinoma of the Testis is generally excellent. The cure rates with multi-modal therapy are around 95%.
What type of cancer is a neoplastic cell?
Neoplastic cells that grow aggressively and spread to other areas are cancerous. There are two types of testicular cancer: Seminoma: It is a slow-growing cancer affecting men in their 30s and 40s, which is usually confined to the testis. These are of 2 types - classical and spermatocytic seminoma.
How do pluripotent stem cells become other cell types?
The process of pluripotent stem cells becoming other cell types is mediated by chemical signaling. Chemicals that act as signals include growth factors, nutrients, and hormones. Stem cells that do not respond to normal signals may grow uncontrollably and cause tumors.
Is Embryonal Carcinoma of the Testis a cure?
The prognosis of Embryonal Carcinoma of the Testis is generally excellent. The cure rates with multi-modal therapy are around 95%. In about 60% of the cases, the tumor is found to have metastasized outside the testis. However, despite such frequent incidences of metastasis at the time of diagnosis, the prognosis is still excellent.
What is the cause of testicular carcinoma?
The cause for Embryonal Carcinoma of the Testis is unknown. It appears under the microscope as a tumor resembling early developing fertilized eggs or embryos, hence the term “embryonal”
What are the two types of seminoma?
These are of 2 types - classical and spermatocytic seminoma. Nonseminoma: It is a fast-growing cancer affecting males in their late teens through 30s, which aggressively metastasizes, or spreads. These are of 4 types - embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma. The cause for Embryonal Carcinoma of the Testis is unknown.
What is the cancer of the testis?
Embryonal Carcinoma of the Testis is a type of testicular cancer affecting the germ cells. Germ cells are precursors to sperm cells that will eventually transform into sperms
Where is embryonal cell carcinoma found?
Embryonal cell carcinoma is a form of testicular cancer that occurs most commonly in the male testes, which are located inside the scrotum. Rarely, embryonal carcinomas are seen in females, in the ovaries. Compared with other types of cancer, embryonal cell carcinoma is rare.
Can testicular cancer be treated?
Depending on the type and stage of testicular cancer, patients may receive one of several treatments, or a combination. Regular testicular self-examinations can help identify growths early, when the chance for successful treatment of testicular cancer is highest.
Where does embryonal carcinoma occur?
Embryonal carcinoma is a relatively uncommon type of germ cell tumour that occurs in the ovaries and testes .
How rare is embryonal carcinoma?
In the ovary, embryonal carcinoma is quite rare, amounting to approximately three percent of ovarian germ cell tumours. The median age at diagnosis is 15 years. Symptoms and signs are varied, and may include sexual precocity and abnormal (increased, reduced or absent) uterine bleeding.
What percentage of testicular cancer is pure embryonal carcinoma?
Testicular. In the testis pure embryonal carcinoma is also uncommon, and accounts for approximately ten percent of testicular germ cell tumours. However, it is present as a component of almost ninety percent of mixed nonseminomatous germ cell tumours.
Does embryonal carcinoma have a protein?
Males with pure embryonal carcinoma tend to have a normal amount of the protein alpha-fetoprotein in the fluid component of their blood. The finding of elevated amounts of alpha-fetoprotein is more suggestive of a mixed germ cell tumour, with the alpha-fetoprotein being released by the yolk sac tumour component.
What are the clinical features of metastasis of embryonal carcinoma?
The clinical features associated with metastasising embryonal carcinoma may include low back pain, dyspnoea, cough, haemoptysis, haematemesis and neurologic abnormalities. Males with pure embryonal carcinoma tend to have a normal amount of the protein alpha-fetoprotein in the fluid component of their blood. The finding of elevated amounts of ...
Is testicular embryonal carcinoma pure?
Testicular embryonal carcinoma occurs mostly (84%) as a component of a mixed germ cell tumor, but 16% are pure. Occasionally, embryonal carcinoma develops predominantly in the context of polyembryoma -like (6%) and diffuse embryoma -like ("necklace" pattern) (3%) proliferations.
What is embryonal tumor?
Embryonal tumors are a collection of biologically heterogeneous lesions that share the tendency to disseminate throughout the nervous system via cerebrospinal fluid (CSF) pathways. Although there is significant variability, histologically these tumors are grouped together because they are at least partially composed of hyperchromatic cells (blue cell tumors on standard staining) with little cytoplasm, which are densely packed and demonstrate a high degree of mitotic activity. Other histologic and immunohistochemical features, such as the degree of apparent cellular transformation along identifiable cell lineages (ependymal, glial, etc.), can be used to separate these tumors to some degree. However, a convention, which has been accepted by the WHO, also separates these tumors on the basis of presumed location of origin within the central nervous system (CNS). Molecular studies have substantiated the differences between tumors arising in different areas of the brain and give partial credence to this classification approach. [ 1]
What is the first step in the management of newly diagnosed nonmedulloblastoma embryonal tumors
Attempting aggressive surgical resection is the first step in the management of newly diagnosed nonmedulloblastoma embryonal tumors. Although previous studies did not demonstrate that the extent of resection is predictive of outcome, [ 25 - 27] one study demonstrated an improved survival when the tumor was completely resected. [ 28 ] [ Level of evidence: 2A] A published study ( COG-ACNS0332 [NCT00392327]) of molecularly classified nonmedulloblastoma embryonal tumors revealed improved overall survival (OS) for patients who had less than 1.5 cm 2 of residual disease compared with patients who had more than 1.5 cm 2 of residual disease. [ 14 ] [ Level of evidence: 1iiA]
Is medulloepithelioma an ETMR?
Medulloepithelioma with the classic C19MC amplification is considered an ETMR, C19MC -altered (refer to the ETMR information above). However, when a tumor has the histological features of medulloepithelioma, but without a C19MC amplification, it is identified as a histologically discrete tumor within the WHO classification system and called medulloepithelioma . [ 15, 16] Medulloepithelioma tumors are rare and tend to arise most commonly in infants and young children. Medulloepitheliomas, which histologically recapitulate the embryonal neural tube, tend to arise supratentorially, primarily intraventricularly, but may arise infratentorially, in the cauda, and even extraneurally, along nerve roots. [ 15, 16]
What is the classification of CNS tumors?
The WHO Classification of Tumors of the CNS classifies nonmedulloblastoma embryonal tumors primarily by histologic and immunohistologic features, with the exception of ETMR and atypical teratoid tumor with rhabdoid features. [ 1] By definition, these tumors arise in the cerebral hemisphere, brain stem, or spinal cord and are composed of undifferentiated or poorly differentiated neuroepithelial cells that may display divergent differentiation. This classification, based on the histopathological characteristics and location of the tumor, is as follows:
What is a nonmedulloblastoma tumor?
In the most recent World Health Organization (WHO) classification of primary central nervous system (CNS) tumors, all nonmedulloblastoma tumors of neuroectodermal origin that lack the specific histopathological features or molecular alterations that define other CNS tumors are classified as CNS em bryonal tumors.
Is surgery considered a standard part of treatment for histologic confirmation of tumor type?
Surgery is considered a standard part of treatment for histologic confirmation of tumor type and as a means to improve outcome. Total or near-total resections are considered optimal, if they can be performed safely. [ 73, 74]
What is a WNT tumor?
WNT tumors are medulloblastomas with aberrations in the WNT signaling pathway and represent approximately 10% of all medulloblastomas. [ 46] WNT medulloblastomas show a WNT signaling gene expression signature and beta-catenin nuclear staining by immunohistochemistry. [ 48] They are usually histologically classified as classic medulloblastoma tumors and rarely have a large cell/anaplastic appearance. WNT medulloblastomas generally occur in older patients (median age, 10 years) and are infrequently metastasized at diagnosis.
What is the treatment for a tumor in the brain?
Surgery to remove as much of the tumor as possible. This is followed by radiation therapy to the brain and spinal cord. Chemotherapy may also be given during and after radiation therapy.
How to treat pineoblastoma in children?
Standard treatment of newly diagnosed pineoblastoma in children aged 3 years and younger includes the following: Biopsy to diagnose pineoblastoma followed by chemotherapy. If the tumor responds to chemotherapy, radiation therapy is given when the child is older. High-dose chemotherapy with stem cell rescue.
What test is used to diagnose medulloblastoma?
Tests that examine the brain and spinal cord are used to diagnose childhood medulloblastoma and other CNS embryonal tumors. A biopsy may be done to be sure of the diagnosis of medulloblastoma and other CNS embryonal tumors. Certain factors affect prognosis (chance of recovery) and treatment options.
Where do medulloblastoma tumors begin?
Medulloblastoma and other central nervous system (CNS) embryonal tumors may begin in embryonic (fetal) cells that remain in the brain after birth.
Can a tumor be removed?
Surgery to remove the tumor. The tumor usually cannot be completely removed because of where it is in the brain. Surgery is often followed by radiation therapy to the brain and spinal cord and chemotherapy.
How does chemo work?
When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body ( systemic chemotherapy ). Although most cannot, some chemotherapy drugs can cross the blood-brain barrier and reach tumor cells in the brain. When chemotherapy is placed directly into the cerebrospinal fluid, it is called intrathecal chemotherapy. Intraventricular chemotherapy is a treatment in which anticancer drugs are placed into the ventricles (fluid-filled cavities) of the brain. Combination chemotherapy is treatment using more than one anticancer drug. The way the chemotherapy is given depends on the type of cancer being treated.
How to get medulloblastoma removed from brain?
For brain tumors, the biopsy is done by removing part of the skull and using a needle to remove a sample of tissue. Sometimes, a computer-guided needle is used to remove the tissue sample. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are found, the doctor may remove as much tumor as safely possible during the same surgery. The piece of skull is usually put back in place after the procedure.
How many cycles of BEP for cancer?
This can help reduce the risk that the cancer will come back. If cancer was found in the lymph nodes after surgery, 2 to 4 cycles of BEP or EP (etoposide and cisplatin) may be given, depending on how many nodes had cancer in them. This has a high cure rate, but it can have side effects (which are mostly short-term).
What is the procedure to remove lymph nodes?
If tumor marker levels are normal, there are 2 main options: Retroperitoneal lymph node dissection (RPLND): This is surgery to remove the lymph nodes at the back of the abdomen. If the lymph nodes that were removed contain cancer, chemo (typically for 2 cycles) might be given.
How long does it take for testicular cancer to recur?
If this happens, it’s usually within the first 2 years after treatment. In general, if the cancer recurs, it’s probably best to get a second opinion from a center with extensive experience in treating relapsed testicular cancer before starting treatment.
What happens after chemo?
Once chemo is complete, the doctor looks for any cancer that's left. If scans and tumor marker levels are normal, no further treatment may be needed.
Can chemo be done without a biopsy?
If there's a high suspicion that the cancer might be a testicular chorio carcinoma, chemo may be started without a biopsy or surgery to remove the testi cle. If the cancer has spread to the brain, surgery (if there are only 1 or 2 tumors in the brain), radiation therapy aimed at the brain, or both may also be used.
Can stage 3 cancer be cured?
Even though stage III cancers have spread by the time they are found, most of them can still be cured.
How many cycles of chemo for lymph nodes?
Chemotherapy: This is typically the preferred treatment. It is usually either 4 cycles of EP (etoposide and cisplatin) or 3 cycles of BEP (bleomycin, etoposide, and cisplatin). Radiation: This may be an option instead of chemo if the lymph nodes aren't enlarged from cancer spread.