What is DIC and how is it treated?
There is no specific treatment for DIC. The goal is to determine and treat the underlying cause of DIC. Supportive treatments may include: Plasma transfusions to replace blood clotting factors if a large amount of bleeding is occurring.Sep 24, 2019
Can a patient survive DIC?
The long-term outlook for people who have DIC depends on how much damage the clots may have caused to the body's tissues. About half of those with DIC survive, but some may live with organ dysfunction or the results of amputations.
What medication begins with DIC?
Prescription diclofenac topical solution (Pennsaid) is used to relieve osteoarthritis pain in the knees. Diclofenac is in a class of medications called nonsteroidal anti-inflammatory drugs (NSAIDs). It works by stopping the body's production of a substance that causes pain.Apr 15, 2021
Can DIC go away?
Treatment for DIC depends on its severity and symptoms. The main goals of treatment for DIC are to control clotting and bleeding and to treat the underlying cause. DIC may go away once the underlying cause is treated.Oct 8, 2019
What is the survival rate of DIC?
Mortality in ED patients with DIC Mortality rates range from 40 to 78% in hospitalized patients experiencing DIC 3,19. The presence of DIC in ED patients results in roughly comparable overall 30-day mortality rates (52%).
What bacteria causes DIC?
DIC is classically associated with Gram negative bacterial infections but it can occur with a similar incidence in Gram positive sepsis. Moreover, systemic infections with other micro-organisms, such as viruses, Rickettsiae and even parasites (e.g. Plasmodium falciparum) may also result in DIC.
Why do doctors not prescribe diclofenac?
12, 2013 study in PLoS Medicine (2013;10:e1001388) indicates that diclofenac use can increase the risk of heart attack or stroke in patients with pre-existing conditions such as diabetes, high cholesterol or other high risk factors for cardiovascular problems.
Can I take Tylenol with diclofenac sodium?
It's safe to take diclofenac with paracetamol or codeine. Do not take diclofenac with similar painkillers, like aspirin, ibuprofen or naproxen, without talking to a doctor.
Why is heparin given in DIC?
Heparin, as an anticoagulant, which, not only inhibits the activation of the coagulation system, but is also an anti-inflammatory and immunomodulatory agent, has been widely used during DIC treatment and in the prevention and treatment of thrombotic diseases.Dec 31, 2013
How does DIC lead to bleeding?
Disseminated intravascular coagulation is a condition in which small blood clots develop throughout the bloodstream, blocking small blood vessels. The increased clotting depletes the platelets and clotting factors needed to control bleeding, causing excessive bleeding.
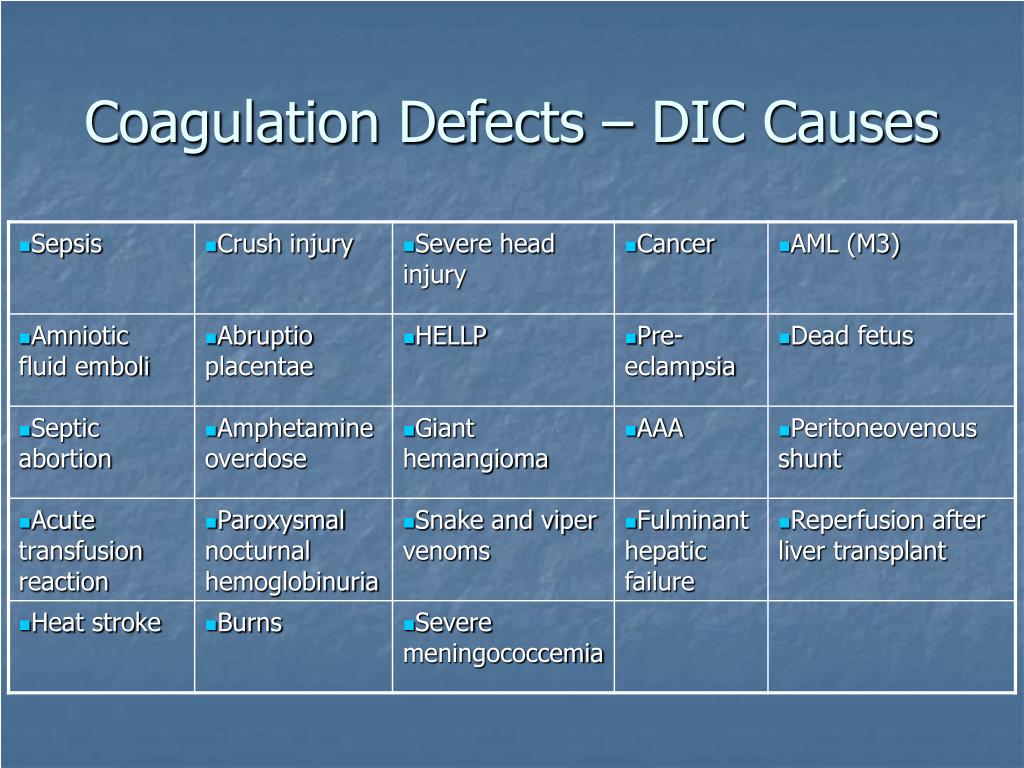
Which client is most at risk for developing disseminated intravascular coagulation DIC?
People who have one or more of the following conditions are most likely to develop DIC: Sepsis (an infection in the bloodstream) Surgery and trauma. Cancer.
What happens when you have a DIC?
In some cases of DIC, small blood clots form in the blood vessels. Some of these clots can clog the vessels and cut off the normal blood supply to organs such as the liver, brain, or kidneys. Lack of blood flow can damage and cause major injury to the organs. In other cases of DIC, the clotting proteins in your blood are consumed.
What are the risks of DIC?
Risk factors for DIC include: 1 Blood transfusion reaction 2 Cancer, especially certain types of leukemia 3 Inflammation of the pancreas (pancreatitis) 4 Infection in the blood, especially by bacteria or fungus 5 Liver disease 6 Pregnancy complications (such as placenta that is left behind after delivery) 7 Recent surgery or anesthesia 8 Severe tissue injury (as in burns and head injury) 9 Large hemangioma (a blood vessel that is not formed properly)
What are the reactions of blood transfusion?
Blood transfusion reaction. Cancer, especially certain types of leukemia. Inflammation of the pancreas (pancreatitis) Infection in the blood, especially by bacteria or fungus. Liver disease. Pregnancy complications (such as placenta that is left behind after delivery) Recent surgery or anesthesia.
Is there a treatment for DIC?
There is no specific treatment for DIC. The goal is to determine and treat the underlying cause of DIC. Supportive treatments may include: Plasma transfusions to replace blood clotting factors if a large amount of bleeding is occurring.
What is the keystone of DIC management?
If the condition causing the DIC is properly dealt with (in the example of the case with bile duct drainage and antibiotics), the coagulopathy will spontaneously resolve. However, in some situations, adjunctive supportive treatment aimed at the coagulation system will be required, because the coagulopathy may proceed for a while even after adequate treatment of the underlying condition has been initiated ( Figure 2 ). 42, 58, 59
What are the mechanisms of coagulation in DIC?
The initiation and propagation of procoagulant pathways with simultaneous impairment of natural anticoagulant systems and suppression of endogenous fibrinolysis as a result of systemic inflammatory activation are leading to platelet activation and fibrin deposition. 15, 29 Important mediators that regulate these processes are cytokines, such as interleukin-1 (IL-1) and IL-6 and tumor necrosis factor-α (TNF-α). In addition, recent studies point to a prominent role of intravascular webs (neutrophil extracellular traps) consisting of denatured DNA from damaged cells and entangling neutrophils, platelets, fibrin, and cationic proteins, such as histones, in the development of thrombus deposition. 30
What are the causes of coagulation activation?
A variety of disorders, including severe sepsis, systemic inflammatory conditions, trauma, and malignant disease, will lead to activation of the coagulation system. In many cases, this coagulation will not result in clinical complications and will not even be identified by routine laboratory tests, but can only be detected when sensitive molecular markers for activation of coagulation pathways are used. 1 However, if the activation of coagulation is sufficiently strong, consumption of platelets and coagulation proteins may become visible through prolongation of routine clotting tests and increasing thrombocytopenia. Systemic activation of coagulation in its most extreme form is known as disseminated intravascular coagulation (DIC). DIC is classically characterized by the simultaneous occurrence of widespread vascular clot deposition, compromising an adequate blood supply to various organs, and thereby contributing to organ failure. 2-5 Due to ongoing activation of the coagulation system and other factors, such as impaired synthesis and increased degradation of coagulation proteins and protease inhibitors, exhaustion of factors and platelets may occur, potentially resulting in profuse bleeding from various sites. In addition, high levels of fibrin degradation products may affect platelet function and fibrin cross-linking and thereby further contribute to the bleeding tendency. 6, 7
What is DIC in coagulopathy?
Disseminated intravascular coagulation (DIC) is a condition characterized by systemic activation of coagulation, potentially leading to thrombotic obstruction of small and midsize vessels, thereby contributing to organ dysfunction. At the same time, ongoing consumption of platelets and coagulation proteins results in thrombocytopenia and low concentrations of clotting factors, which may cause profuse hemorrhagic complications. DIC is always secondary to an underlying condition, such as severe infections, solid or hematologic malignancies, trauma, or obstetric calamities. A reliable diagnosis of DIC can be made through simple scoring algorithms based on readily available routine hemostatic parameters. The cornerstone of supportive treatment of this coagulopathy is management of the underlying condition. Additionally, administration of heparin may be useful, and restoration of physiological anticoagulants has been suggested, but has not been proven successful in improving clinically relevant outcomes so far. In patients with major bleeding or at risk for hemorrhagic complications, administration of platelet concentrates, plasma, or coagulation factor concentrates should be considered.
What are the symptoms of liver cirrhosis?
At physical examination, the most prominent signs were hepatic encephalopathy, jaundice, splenomegaly, and ascites. Laboratory test results showed a hemoglobin concentration of 7.0 mmol/L (11.3 g/dL), a leukocyte count of 7.9.2 × 10 9 /L, a platelet count of 88 × 10 9 /L (1 week before admission, 84 × 10 9 /L), a bilirubin concentration of 84 μmol/L (1.2 mg/dL), and an albumin concentration of 28 g/L. Coagulation tests reveal a PT of 17 seconds (normal, <12 seconds), an aPTT of 52 seconds (normal, <28 seconds), a D-dimer concentration of 1.0 μg/mL (normal, <0.5 μg/mL), and a fibrinogen concentration of 2.1 g/L (normal, 1-3 g/L). The question is whether these coagulation abnormalities are due to liver failure-related coagulopathy or DIC, secondary to an infection.
What is the use of plasma to restore coagulation factors?
The use of large volumes of plasma may be required to restore normal levels of coagulation factors. Coagulation factor concentrates, such as prothrombin complex concentrate, may overcome this impediment, but these agents may lack important factors (eg, factor V).
What was the blood pressure after hemicolectomy?
A 68-year-old man was admitted to the intensive care unit because of respiratory failure 3 days after a hemicolectomy. His blood pressure was 100/60 mm Hg, heart rate was 120 beats per minute (regular), respiratory rate was 28 breaths per minute, and temperature was 38.1°C. Arterial blood gas analysis showed a Pa o2 of 8.4 kPa (63 mmHg) and oxygen saturation of 84% while on 5 L supplemental oxygen. Laboratory analysis showed a hemoglobin concentration of 6.8 mmol/L (11.0 g/dL), a leukocyte count of 9.2 × 10 9 /L with 7.7 × 10 9 /L neutrophils, a remarkable left shift and some schistocytes in the blood smear, a creatinine concentration of 212 μmol/L (2.4 mg/dL), a bilirubin concentration of 18 μmol/L (1.2 mg/dL), a lactic acid concentration of 3.3 mmol/L (30 mg/dL), and a bicarbonate concentration of 18 mmol/L. The patient was intubated and ventilated, achieving an oxygen saturation of 98%, and hemodynamically stabilized with crystalloids and IV administration of dopamine. He was further treated with broad spectrum antibiotics and continues subcutaneous heparin prophylaxis.
Overview
Disseminated intravascular coagulation is a rare and serious condition that can disrupt your blood flow. It is a blood clotting disorder that can turn into uncontrollable bleeding.
Symptoms and Causes
One classic symptom is uncontrolled bleeding from several areas of your body. Other symptoms are:
Management and Treatment
Your healthcare provider’s first step is treating the underlying condition that caused you to develop DIC. They might use supportive treatments to improve blood flow if you have blood clots or to slow your blood loss. Those treatments are:
Prevention
DIC is linked to medical conditions such as cancer, pancreatitis and liver disorders. Unfortunately, that means there’s very little you can do to prevent DIC. What you can do is to talk to your healthcare provider about DIC so you know what changes in your body might be a sign of it.
Living With
Most people who have DIC are already coping with illness or a medical condition. Being diagnosed with disseminated intravascular coagulation means you have another medical concern to manage as you continue the treatment and testing for the medical condition that caused your DIC. Here are some suggestions that might help:
Can DIC be corrected?
The outlook of your treatment depends on what caused you to develop DIC. If the initial problem can be corrected, then DIC will resolve. If not, your doctor may prescribe blood thinners to prevent blood clots .
Can DIC cause complications?
DIC can cause complications, especially when it isn’t treated properly. Complications can occur from both the excessive clotting that happens in the early stages of the condition and the absence of clotting factors in the later stages. Complications include:
What is DIC in a patient?
Disseminated intravascular coagulation (DIC) involves abnormal, excessive generation of thrombin and fibrin in the circulating blood. During the process, increased platelet aggregation and coagulation factor consumption occur. DIC that evolves slowly (over weeks or months) causes primarily venous thrombotic and embolic manifestations; DIC that evolves rapidly (over hours or days) causes primarily bleeding. Severe, rapidly evolving DIC is diagnosed by demonstrating thrombocytopenia, an elevated partial thromboplastin time and prothrombin time, increased levels of plasma D-dimers (or serum fibrin degradation products), and a decreasing plasma fibrinogen level. Treatment includes correction of the cause and replacement of platelets, coagulation factors (in fresh frozen plasma), and fibrinogen (in cryoprecipitate) to control severe bleeding. Heparin is used as therapy (or prophylaxis) in patients with slowly evolving DIC who have (or are at risk of) venous thromboembolism.
What is heparin used for?
Heparin is used as therapy ( or prophylaxis) in patients with slowly evolving DIC who have (or are at risk of) venous thromboembolism. (See also Overview of Coagulation Disorders .)
What is DIC in a blood test?
In association with coagulation, the fibrinolytic pathway is also activated. DIC usually begins rapidly and causes bleeding and microvascular occlusion, leading to organ failure.
What are the enzymes in snake venom?
Enzymes in certain snake venoms that enter the circulation, activate one or several coagulation factors, and either generate thrombin or directly convert fibrinogen to fibrin. Aortic aneurysms or cavernous hemangiomas (Kasabach-Merritt syndrome) associated with vessel wall damage and areas of blood stasis.
What are the complications of obstetrics?
Complications of obstetrics (eg, abruptio placentae , saline-induced therapeutic abortion, retained dead fetus or products of conception, amniotic fluid embolism ): Placental tissue with tissue factor activity enters or is exposed to the maternal circulation.
What is the term for a vessel wall damage caused by a hemangioma?
Aortic aneurysms or cavernous hemangiomas (Kasabach-Merritt syndrome) associated with vessel wall damage and areas of blood stasis. Slowly-evolving disseminated intravascular coagulation typically results mainly from cancer, aneurysms, or cavernous hemangiomas.
What are the complications of prostate surgery?
Complications of prostate surgery that allow prostatic material with tissue factor activity (along with plasminogen activators) to enter the circulation.
What is DIC in septic shock?
Disseminated intravascular coagulation, or DIC, is a complicated condition that can occur when someone has severe sepsis or septic shock. Both blood clotting and difficulty with clotting may occur, causing a vicious cycle.
What is the primary task of DIC?
When someone has DIC caused by sepsis, the primary task is to treat the sepsis and the infection that caused it. In addition to treating sepsis, the clots may have to be dissolved and new clots prevented. This may be done with heparin, an anticoagulant, often called a blood thinner.
How many people die from sepsis?
Worldwide, one-third of people who develop sepsis die. Many who do survive are left with life-changing effects, such as post-traumatic stress disorder (PTSD), chronic pain and fatigue, organ dysfunction (organs don’t work properly), and/or amputations.
What causes DIC?
There are several medical conditions that can cause DIC, including sepsis. DIC affects about 35% of patients who have sepsis. Sometimes incorrectly called blood poisoning, sepsis is the body’s often deadly response to infection.
What happens if blood clots are not circulating properly?
For example, if clots prevent blood from circulating properly to the hands or feet, the tissue may start to turn splotchy, then bluish in color (cyanotic), and then black (gangrenous) if the skin dies.
What does it mean when you have a small patch of skin?
For some people, this may be a small patch of skin or a few fingers or toes, but for others, it could mean amputation of one or more limbs . If blood isn’t effectively reaching vital organs like your kidneys, liver, or lungs, they may have trouble functioning.
Does DIC cause bleeding?
On the reverse side of the cycle, DIC can cause increased bleeding because the body is using up so many of the blood clotting proteins for the multiple blood clots in the blood vessels that there are not enough of them left to clot the blood elsewhere.
Why do blood clots run out?
The clumps can block small blood vessels and slow blood flow to organs. When your blood clots too often, substances that help with clotting can run out. If that happens, they won’t be there when your body truly needs them. That can cause severe bleeding anywhere from just beneath the skin to deep inside the body.
What are the complications of disseminated intravascular coagulation?
Either overactive clotting or the bleeding that follows can cause complications that can threaten your life. These may include: Acute respiratory distress syndrome, a severe lung condition that leads to low levels of oxygen in your blood.
What is DIC in medical terms?
Disseminated intravascular coagulation (DIC) is a blood clotting disorder. You cut your finger or nick your leg and your body gets to work to stop the bleeding. You don’t give it a second thought. But what if this normal blood clotting process went into overdrive?
How do you know if you have DIC?
Other signs and symptoms of DIC depend on what’s causing it. You may have these types of bleeding: Where you have cuts or wounds. Where you had surgery, an IV needle, or a catheter. In a bruise or in small red dots on the skin. From your nose, gums, or mouth, including bleeding when you brush your teeth.
What type of treatment is needed for clotting?
When you get treatment for the underlying problem, the clotting should improve. But you may need other treatment as well, such as: Platelet or plasma transfusion (these are blood components) to stop or prevent bleeding.
What are the complications of childbirth?
Complications of childbirth. Cancer. Certain cancers or problems during pregnancy may trigger proteins needed for clotting. The proteins may spring into action during pregnancy, for example, if the placenta separates from the uterus or if amniotic fluid enters the mother’s bloodstream.
How to treat DIC?
If you have DIC, follow your doctor’s treatment plan and get regular follow-up care. Be sure to: Take all medicine exactly as your doctor prescribes. Follow through on treatment for the underlying condition. Know when to return for office visits and blood tests. Tell all your doctors if you are on blood thinners.