Healthline.com
1. Flavonoids...
2. Deglycyrrhizinated licorice...
3. Probiotics...
4. Honey...
5. Garlic...
6. Cranberry...
7. Mastic...
Learn More...Medicalnewstoday.com
1. Probiotics...
2. Ginger...
3. Colorful fruits...
4. Plantain bananas...
5. Honey...
6. Turmeric...
7. Chamomile...
8. Garlic...
Learn More...Allremedies.com
1. Cabbage - Carrots...
2. Coconut...
3. Bananas...
4. Honey...
5. Garlic...
6. Cayenne Pepper...
7. Licorice Root...
8. Fenugreek Honey...
Learn More...Trueremedies.com
1. Honey...
2. Garlic...
3. Apple Cider Vinegar...
4. Broccoli...
5. Cabbage...
6. Ginger...
7. Licorice...
8. Mastic...
Learn More...Effectiveremedies.com
1. Cabbage And Carrot...
2. Cayenne Pepper And Warm Water...
3. Bananas With Honey And Milk...
4. Coconut...
5. Fenugreek, Water, Honey, And Milk...
6. Licorice, Water, And Cooked Broken Rice...
7. Raw Honey...
Learn More...Why is decubitus ulcer a serious condition?
Decubitus ulcers often occur on the skin covering bony areas. The most common places for a decubitus ulcer are your: This condition is common among people who are older and people who have decreased mobility. Left untreated, infections can spread to the blood, heart, and bones and become life threatening.
What is the proper treatment for an ulcer?
You may be asked to:
- Clean the wound regularly
- Apply a dressing to the ulcer
- Avoid products that cause skin sensitivity
- Wear compression stockings to prevent blood from pooling in the legs and to speed healing
- Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
- Take oral antibiotic medicines to prevent or treat an infection
What are the stages of an ulcer?
- The depth of a Stage IV pressure ulcer varies by anatomical location. ...
- Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon, or joint capsule), making osteomyelitis likely to occur.
- Exposed bone/tendon is visible or directly palpable.
How to treat a stage 3 pressure ulcer?
Treatment of Stage 3 and Stage 4 Pressure Ulcers . The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies.

What antibiotics treat decubitus ulcers?
Amoxicillin-potassium clavulanate is a naturally occurring beta-lactam structurally similar to the penicillin nucleus. This antibiotic group of beta-lactam/beta-lactamase combination has demonstrated a broad-spectrum activity; therefore, it is frequently used for the treatment of infected pressure ulcers.
What is the #1 treatment of pressure ulcers?
If you believe that you have a stage 1 pressure ulcer, you should remove all pressure from the area. Keep the area as dry and clean as possible to prevent bacterial infections. To speed up the healing process, you should eat adequate calories and have a diet high in minerals, proteins, and vitamins.
Which ointment is best for bed sores?
Options that are antimicrobial or hydrocolloid, or that contain alginic acid, may be best. Dressings are available for purchase online. Use topical creams: Antibacterial creams can help combat an infection, while barrier creams can protect damaged or vulnerable skin.
What is the best treatment for a Stage 2 pressure ulcer?
Stage II pressure sores should be cleaned with a salt water (saline) rinse to remove loose, dead tissue. Or, your provider may recommend a specific cleanser. Do not use hydrogen peroxide or iodine cleansers. They can damage the skin.
What dressing is used for stage 1 pressure ulcer?
Thin hydrocolloid dressings (eg DuoDERM® SignalTM and DuoDERM® Extra Thin) are increasingly used in the management of Category/Stage I pressure ulcers. The slippery outer surface assists in reducing friction or shear to the underlying skin to protect it against further damage7.
Is Betadine good for ulcers?
Results: Compression increases the ulcer healing rate compared with no compression. Using the same local povidone-iodine (Betadine) treatment with compression bandages is more effective (82%) for ulcus healing than without compression therapy (62%).
Is Vaseline good for bed sores?
Clean open sores on the skin with salt water (saline, which can be made by boiling 1 quart of water with 1 teaspoon of salt for 5 minutes and kept cooled in a sterile container). Apply a thin layer of petroleum jelly (Vaseline®) and then cover with a soft gauze dressing.
What does a Stage 2 pressure sore look like?
At stage 2, the skin breaks open, wears away, or forms an ulcer, which is usually tender and painful. The sore expands into deeper layers of the skin. It can look like a scrape (abrasion), blister, or a shallow crater in the skin. Sometimes this stage looks like a blister filled with clear fluid.
When should you not use silver dressing?
Silver dressings should not be used in the absence of localised (overt or covert), spreading or systemic infection, unless there are clear indicators that the wound is at high risk of infection or re-infection. Box 5 summarises the situations where silver dressings should not be used.
What is a decubitus ulcer?
Decubitus ulcers are simply damaged skin, usually over bony areas, that result from lack of blood flow to the area because of a person staying in one position for too long.
How long does it take for a decubitus ulcer to heal?
Most stage I and stage II decubitus ulcers will heal on their own within a couple of weeks with conventional methods. However, stage III and stage IV ulcers will probably not heal without special treatment and possible surgery.
How many people die from decubitus ulcers?
Decubitus ulcers can be life threatening if left untreated, and are the primary cause of death in 7 to 8 percent of all patients that are paralyzed. Investigations have determined that one-third of the patients hospitalized that have pressure ulcers die while they are hospitalized.
How often should you change position for decubitus ulcer?
If the patient can move themselves, they need to change position every ten minutes. If they cannot do it themselves, a caregiver needs to reposition the patient every two hours even if they are utilizing a specialty bed or surface. If a patient receives an ulcer by sitting too long, the patient should be put on bed rest and repositioned frequently. There are many pressure reduction devices that can aid the patient in keeping pressure off of the decubitus ulcer.
What is the procedure to remove dead tissue from a wound?
Many times these types of wounds require surgery and dressings for this kind of ulcer should be applied by a professional. A surgery called debridement is utilized to remove all dead tissue so that the wound will not become infected.
Can a decubitus ulcer be treated without surgery?
If medical management of the decubitus ulcer is complete and meticulous, most ulcers can be treated and healed without the intervention of a surgeon. However, treating decubitus ulcers is demanding, and it is much easier to prevent the ulcer rather than having to treat it.
Can you cover decubitus ulcers?
Usually Stage I decubitus ulcers will not need to be covered. For Stage II and III ulcers, use saline solution to clean the wound and dry it carefully. Apply either gauze dampened with saline, a hydrocolloid dressing (for example DuoDerm), or a thin foam dressing such as Allevyn.
What is a decubitus ulcer?
A decubitus ulcer is also known as a pressure ulcer, pressure sore, or bedsore. It’s an open wound on your skin. Decubitus ulcers often occur on the skin covering bony areas. The most common places for a decubitus ulcer are your: This condition is common among people who:
How to treat ulcers?
Treatment can include: medications. local wound care, including specific dressing recommendations. lifestyle changes, such as repositioning frequently and using special off-loading cushions, as well as making healthy eating choices.
How to remove dead tissue from decubitus?
A process to remove dead or infected tissue called debridement may be recommended by your doctor. Keeping the site clean, dry, and free of irritants is important to promote healing. Off-loading the pressure as well as frequent repositioning is very important when treating a decubitus ulcer.
What is the dark plaque inside a sore called?
A dark, hard plaque called eschar may be inside the sore, which makes full evaluation and staging difficult. Sometimes your doctor requires further imaging or surgical evaluation of the area to determine the full extent of the ulcer. The ulcer may also have discolored debris known as slough (yellow, tan, green, or brown), which makes full evaluation difficult.
Can you move a person with deep ulcers?
This condition is common among people who: are older. have decreased mobility. spend long periods in bed or a wheelchair. can’t move certain body parts without help. have fragile skin. The condition is treatable, but chronic deep ulcers can be difficult to treat.
Decubitus meaning and definition
Decubitus is the Latin name for pressure ulcers. Decubitus refers to skin tissue damaged by permanent pressure, shear force, friction, or a combination of these effects. If it’s not prevented and treated normally, skin cells and even bone cells can die during this disease.
What is the cause of decubitus ulcers?
The primary cause of decubitus ulcers is the time that the patient spends in bed. Unfortunately, bedridden patients easily develop decubitus ulcers, especially when they have limited mobility. Elderly and paralyzed patients with pathological weaknesses or the ones with multiple sclerosis or stroke are at particular risk.
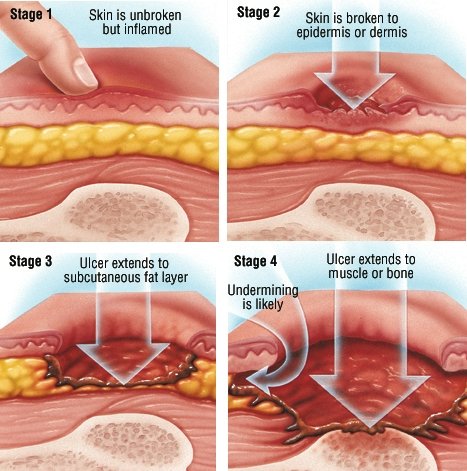
Pressure ulcers stages
The development of pressure ulcers has four distinct stages, according to the depth of the wound. The later the treatment begins, the harder it gets to heal bedsores.
Pressure ulcers treatment: how to treat bedsores?
Prevention is the most important, but if it’s already in one of the above-mentioned stages, proper treatment is inevitable for the patient. The spreading of pressure ulcers has to be prevented.
Decubitus ulcers prevention with dermolex
How to prevent pressure ulcers? Herbs can play a complementary role in the prevention and treatment of bedsores. Our dermolex gel includes herbs like aloe vera, echinacea purpurea, or menthol.
How to treat decubitus ulcers?
Treatment for decubitus ulcers depends on the stage of the ulcer: Stage 1 & 2: Keep the area clean and dry. If the skin is broken, apply antibiotic cream then cover the wound with a bandage. Stage 3 & 4: Clean the wound and remove any dirt and necrotic tissue. Apply antibiotic cream, pack the wound completely with gauze, ...
What is a stage 4 decubitus ulcer?
This is an example of a stage 4 decubitus ulcer because the wound goes all the way to the bone. Stages 1 & 2 are considered partial thickness wounds, and stages 3 & 4 are considered full thickness wounds.
What are the stages of sacral decubitus?
These are the 4 different stages of ulcers: Stage 1: The skin appears red but remains intact. There is no open wound present, but the area may still be painful.
How to treat a stage 2 ulcer?
It's very important to dry the area completely after cleaning. If a stage 2 ulcer forms, you can apply a topical antibiotic ointment to the wound, then cover the wound with a clean, dry bandage.
How to get rid of necrotic tissue?
This necrotic tissue can be removed with scissors or a scalpel, washing the dead tissue away with a gentle stream of water, or using a special chemical agent to dissolve the dead tissue. Apply a topical antibiotic cream to the wound.
Where is the sacral region of a stage 3 ulcer?
The sacral region is near the lower back at the bottom of the spine.
Can you move your body when you have ulcers?
Ulcers often form in people who are bedridden and are not able to move their bodies. The weight of their bodies on bony areas such as their sacrum and heels can damage the skin and reduce blood flow, eventually leading to ulcers. Decubitus ulcers are staged based on the depth of the wound: Stage 1: Skin is intact.
How to care for pressure ulcers?
Generally, cleaning and dressing a wound includes the following: Cleaning. If the affected skin isn't broken, wash it with a gentle cleanser and pat dry.
What can a social worker do for a child with pressure ulcers?
Parents or caregivers of children with pressure ulcers can talk with a child life specialist for help in coping with stressful health situations.
What to do if a bedsore doesn't heal?
One method of surgical repair is to use a pad of your muscle, skin or other tissue to cover the wound and cushion the affected bone (flap surgery).
What is the best way to heal a wound?
A bandage speeds healing by keeping the wound moist. It also creates a barrier against infection and keeps skin around it dry. Bandage choices include films, gauzes, gels, foams and treated coverings. You might need a combination of dressings.
How to treat bedsore?
The first step in treating a bedsore is reducing the pressure and friction that caused it. Strategies include: Repositioning. If you have a bedsore, turn and change your position often. How often you reposition depends on your condition and the quality of the surface you are on. Using support surfaces.
How to heal a wound?
To heal properly, wounds need to be free of damaged, dead or infected tissue. The doctor or nurse may remove damaged tissue (debride) by gently flushing the wound with water or cutting out damaged tissue.
How do pressure ulcers heal?
The healing process varies depending on the stage of the pressure ulcer. Stage I & II pressure ulcers and partial thickness wounds heal by tissue regeneration. Stage III & IV pressure ulcers and full thickness wounds heal by scar formation and contraction.
What is pressure ulcer?
Previously called decubitus or bed sore, a pressure ulcer is the result of damage caused by pressure over time causing an ischemia of underlying structures. Bony prominences are the most common sites and causes. There are many risk factors that contribute to the development of pressure ulcers.
How many stages are there in pressure ulcers?
Pressure ulcers are classified by stages as defined by the National Pressure Ulcer Advisory Panel (NPUAP). Originally there were four stages (I-IV) but in February 2007 these stages were revised and two more categories were added, deep tissue injury and unstageable. Pressure Ulcer Staging.
What is pressure ulcer dressing?
Background. Pressure ulcers, also known as bedsores, decubitus ulcers and pressure injuries, are localised areas of injury to the skin or the underlying tissue, or both. Dressings are widely used to treat pressure ulcers and promote healing, and there are many options to choose from including alginate, hydrocolloid and protease‐modulating dressings.
What is the NMA for pressure ulcers?
A network meta‐analysis (NMA) of data from 39 studies (evaluating 21 dressings and topical agents for pressure ulcers) is sparse and the evidence is of low or very low certainty (due mainly to risk of bias and imprecision). Consequently we are unable to determine which dressings or topical agents are the most likely to heal pressure ulcers, and it is generally unclear whether the treatments examined are more effective than saline gauze.
What is RCT in wound care?
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
How much did pressure ulcers cost in 2006?
Figures from the USA suggest that for half a million hospital stays in 2006, 'pressure ulcer' was noted as a diagnosis; for adults, the total hospital cost for these stays was USD 11 billion ( Russo 2008 ).
Can topical agents be used for pressure ulcers?
Topical agents have also been used as alternatives to dressings in order to promote healing. A clear and current overview of all the evidence is required to facilitate decision‐making regarding the use of dressings or topical agents for the treatment of pressure ulcers.