
How do you fix colonic inertia?
Several procedures have been attempted to treat colonic inertia. These include segmental colectomy, subtotal colectomy with ileosigmoid or cecorectal anastomosis, and total abdominal colectomy with ileorectal anastomosis (TAC IRA).
What is colonic inertia constipation?
Treatment of colonic inertia Fortunately, most problems with motility in the lower gut can be resolved with changes in diet and exercise. Such dietary changes could include: eating foods high in fiber drinking plenty of water avoiding dairy products avoiding fatty foods
What are the treatment options for constipation of colonic Interia?
Nov 15, 2017 · Some people do notice relief of colonic inertia symptoms following a change in their eating habits. A lot of fruits and vegetables, as well as plenty of water, can be helpful. Consuming foods that...
When is surgery indicated for colonic inertia?
For treating the acute constipation of colonic interia, dietary measures and regular exercise can help to control the symptoms by softening the stool, strengthening the internal system and improving activity of abdominal muscles. Dietary measures include: Adequate fluid intake Intake of 10-12 glasses of water Consumption of Dietary fibres
How do you treat a colonic distention?
Although infrequent, colonic distention can recur following successful treatment with neostigmine. Some individuals with Ogilvie syndrome may be treated with colonic decompression, a procedure that reduces pressure within the colon.
What is colonic inertia?
What is colonic inertia? Colonic inertia is referred to as a motility disorder; that is, it is an abnormal passage of waste through the digestive system. Motility disorders are very common, especially problems associated with constipation and diarrhea.
How can I get my colon to work again?
Eat high-fiber foods such as whole-wheat grains, fresh vegetables, and beans. Use products containing psyllium, such as Metamucil, to add bulk to the stools. Try to drink 2 to 3 liters of fluid a day (unless you have a medical condition that requires you to restrict your fluid intake).Jul 16, 2020
How do you treat slow gut motility?
Some potential treatments for slowed digestion and STC include the following:Evaluating fiber intake. Significantly increasing the amount of fiber in the diet may make STC worse. ... Reducing the use of stimulant laxatives. ... Enemas. ... Bowel retraining. ... Surgery. ... Interferential electrical stimulation.
How long after a colonic do you poop?
What happens after your colonic? Afterwards you might get slight stomach cramping, because you've just put your gut through a workout and you might find that your stools for the next day or so are slightly looser than normal. But everything should be back to normal within 24 hours.Apr 10, 2019
Can I take a laxative with Motegrity?
Motegrity is likely safe to take with over-the-counter (OTC) constipation medications, such as stool softeners and laxatives. But be sure to talk with your doctor before using Motegrity with other medications, whether they're OTC or prescription drugs.
What are the signs of a blocked bowel?
Symptoms of intestinal obstruction are:Severe pain in your belly.Severe cramping sensations in your belly.Throwing up.Feelings of fullness or swelling in your belly.Loud sounds from your belly.Feeling gassy, but being unable to pass gas.Constipation (being unable to pass stool)
How do you know if you have a blockage in your bowels?
Symptoms of an intestinal blockage include severe belly pain or cramping, vomiting, not being able to pass stool or gas, and other signs of belly distress.
What food clears your bowels?
5 colon-cleansing foodsBroccoli. There are so many different ways to add broccoli to your diet. ... Dark, leafy greens. Eating dark, leafy greens like spinach, kale, and chard is a great way to cleanse your colon. ... Milk. You can use milk for more than just your morning cereal. ... Raspberries. ... Oatmeal.
What causes poor peristalsis?
Common Causes Gastrointestinal motility can be impaired due to: A problem within the muscles that control peristalsis. A problem with the nerves or hormones that govern the muscles' contractions.Aug 9, 2021
Can motility disorders be fixed?
These occur as a result of another condition such as diabetes, alcohol consumption, or scleroderma. Treatment will usually be aimed at the disease causing the motility disorder, but sometimes specific treatment including surgery may be required to help with swallowing difficulties.
How can I increase my gut motility naturally?
A diet that emphasizes natural, unprocessed fruit and vegetables can kick-start digestion and help make you more regular unless you have IBS, gastroparesis or other chronic gastrointestinal condition. Good sources of fiber include: almonds and almond milk. prunes, figs, apples, and bananas.
What is colonic inertia?
Colonic inertia is referred to as a motility disorder; that is, it is an abnormal passage of waste through the digestive system. Motility disorders are very common, especially problems associated with constipation and diarrhea.
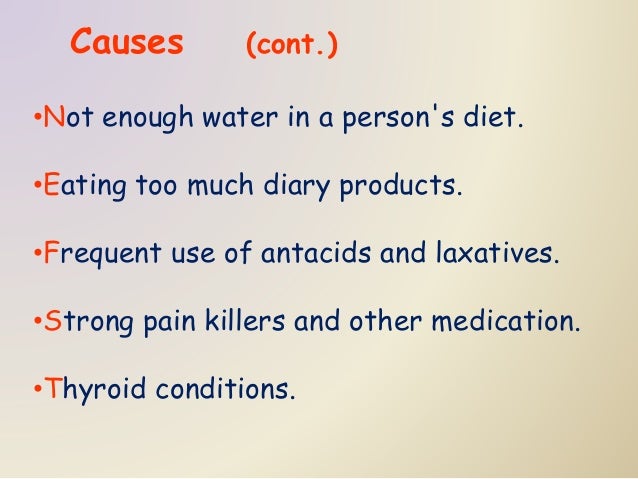
What causes inertia in the colon?
Colonic inertia may be caused by one or more of the following: nerve or muscle damage. not enough water in a person's diet. eating too much dairy products. frequent use of antacids and laxatives. strong pain killers and other medication. thyroid conditions.
Does shortening the colon require a colostomy?
Most of the colon is removed, and the small intestine is attached directly to the rectum. This procedure does not require a colostomy.
Is a total abdominal colectomy dangerous?
It is not quite as dangerous as open heart surgery, chest or brain surgery, but it is major surgery. It is a bigger operation than a hysterectomy. It involves removing about eighty percent of the large intestine. The technical name for the operation is total abdominal colectomy and ileorectal anastomosis.
What are the symptoms of colonic inertia?
Just what are the signs and symptoms of colonic inertia? Actually, there are a number of colonic inertia symptoms that a person could experience. Some of the most common are listed below: 1 Abdominal bloating 2 Pain 3 Difficulty defecating 4 Haemorrhage 5 Constipation 6 Nausea and/or vomiting 7 Excessive gas
What causes inertia in the colon?
There are other factors that could lead to colonic inertia, including certain health conditions such as multiple sclerosis, Parkinson’s disease, irritable bowel syndrome, hypothyroidism, and depression. People who suffer from colon cancer, are sedentary, take antidepressants and pain drugs, are pregnant or are stressed out, ...
How long does it take to pass stool?
People who suffer from colonic inertia usually do not pass stool for anywhere from 7 to 10 days or in some cases even longer. There are situations where this disorder also involves abnormalities in movement ...
What is the best way to get stool out of your body?
Fiber. Insoluble fiber can add bulk to the volume of the stool, which can be helpful to people who suffer from constipation. It can make it easier for stool to move through the colon and out of the body, but can be problematic for those who suffer from colonic inertia.
How do you know if you have colonic inertia?
Some of the most common are listed below: Abdominal bloating. Pain. Difficulty defecating. Haemorrhage. Constipation. Nausea and/or vomiting. Excessive gas.
How long does it take for a colon xray to show a ring?
Usually rings appear in the colon after about 12 hours.
What is the purpose of a barium enema?
A barium enema, which is a study using x-rays and a liquid barium to get a clear picture of the colon and rectum , can also be used. A defecography, which is similar to a barium enema, is another testing option.
How to treat colonic interia?
For treating the acute constipation of colonic interia, dietary measures and regular exercise can help to control the symptoms by softening the stool, strengthening the internal system and improving activity of abdominal muscles. Dietary measures include: Adequate fluid intake. Intake of 10-12 glasses of water.
Why is colonic inertia a defecation disorder?
Colonic inertia is a defecation disorder occurs due to abnormality in the neuromuscular control of GI tract. In colonic inertia gastric motility is hampered due to malfunctioning of muscles and nerves present in the GI tract. The waste materials do not pass smoothly within the colon which delays the empting of faeces from the GI tract.
How long does colonic interia last?
For 7- 10 days the passage of stool is ceased in case of chronic colonic inertia. It is found that in colonic interia, nerves and muscles present in colon gets affected ...
What is the prime symptom of colonic inertia?
The prime symptom of colonic inertia is severe constipation. In such cases, individual do not pass stool for several days and he/she takes much time in washroom and has to give much more strain to rectal emptying. Some may feel incomplete defecation due to partial rectal emptying.
How to know if you have incomplete defecation?
Some may feel incomplete defecation due to partial rectal emptying. Strain in the colonic and pelvic muscles and incomplete rectal emptying also results in the following symptoms: Hard stool. Irregular (less than 3 times a week) stool pass. Bloody stool . Blood discharged during defecation . Painful defecation.
What causes colon inertia?
Other than this, inadequate balanced diet which has insufficient dietary fibres also causes constipation. Water and fluid insufficiency also causes hard stool and constipation.
What is the surgical process of removing the colon?
Surgical process involves complete removal of the colon and reconnects the small intestine to the rectum. This intervention is rare as there are debates and controversies about the benefit from this surgery. This surgical process is not useful if the patient has upper GI tract obstruction, so careful diagnosis is very important to get the optimum result.
What is colonic inertia?
Sometimes colonic inertia is accompanied by abnormalities in motility of the upper intestine including delayed emptying of the stomach and small intestinal pseudo-obstruction (a disorder that causes symptoms of blockage, but no actual blockage).
When do you start using stimulants for colonic inertia?
It often begins at a young age (between ages 20–30). This condition can result in severe and stubborn constipation. It is not uncommon for individuals with colonic inertia to begin to use stimulant laxatives as a treatment.
How many rings are in a colonic transit?
The time required to excrete these substances is called colonic transit. To perform a marker test, a capsule containing a number of tiny rings (usually 24) is ingested by mouth. These rings have been specially treated so that they are clearly visible on an abdominal x-ray.
What to do if colonic transit time is normal?
If colonic transit time is normal, and medications or other medical disorders ruled out, treatment may include: Increasing water and fiber intake. Following a bowel retraining program (regular and unhurried routine for having bowel movements) Getting adequate exercise.
What is delayed colonic action?
People with delayed colonic action (medically termed colonic inertia) have difficulty with moving stool through the colon.
How long does it take for a colon to pass a stool?
Individuals with colonic inertia often do not pass a stool for 7–10 days at a time.
Why is it important to see a doctor for constipation?
This is especially important if constipation is accompanied by pain, bleeding, or a recent change in bowel habits. Discuss the use of any medications with your physician to see if they may be contributing to your symptoms.
How to assess colonic tone and sensitivity?
To assess colonic tone and sensitivity, one can connect a barostat in the manometer. This procedure is useful because studies show that, in addition to motor dysfunction, a sensory dysfunction – or even an isolated sensory neuropathy – may also be present. However, this may also be only an effect, not a cause.
How often does a colon move from the cecum to the rectosigmoid?
Severe/intractable colic inertia or slow transit constipation is the inability that the colon has to modify stool consistency, so as to make them move from the cecum to rectosigmoid at least once every three days. There is a significant delay in colonic transit, not attributable to any other cause. 1, 2, 3, 4.
What changes are associated with slow transit constipation?
However, a decrease in fatty acid amide hydrolase (FAAH) activity would lead to an increase of two endocannabinoids: anandamide and 2-araquidonilglicerol (2-AG) which, through their action on cannabinoid receptor type 1 (CB1), would lead to a reduction of intestinal motility.25 The brain-derived neurotrophic factor (BDNF) appears to influence the maintenance and survival of the enteric nervous system, accelerating the colonic emptying and increasing the frequency of bowel movements. Studies in mice have suggested that a change of BDNF would lead to a change in the neural structure of the intestinal innervation, with denervation, causing atrophy and secondary smooth muscle degeneration [with a decrease in smooth muscle α-actin (α-AML) expression] through the kinase tropomyosin B receptor-phospholipase C/inositol triphosphate (TrkB-PLC-IP3) pathway. A decrease of this factor in human patients has been demonstrated.26 An increase in the number of intact (not degranulated) mast cells in the colon of these patients was also observed, but it was suggested that this would be a potential compensatory mechanism, in order to repair any damaged neuroenteric circuits, taking into account that they constitute a source of nerve growth factors. 27 Furthermore, a study with mice suggested that mast cell deficiency could lead to an inflammatory condition that would decrease muscle contractility by reducing the reactivity to acetylcholine (Ach), regardless of the decrease in the number of the interstitial cells of Cajal.28 Apparently, the peptide YY (PYY) is increased in the ascending colon in some patients, constituting a possible etiological factor, by leading to an increased absorption and to a decreased secretion of water and electrolytes, and resulting in an increase of the ileal brake force and in the inhibition of intestinal motility.29 The downregulation of microRNA128 in the colon of these patients appears to lead to increased numbers of macrophages, which could lead to loss or dysfunction of the interstitial cells of Cajal. 9 A decrease in the expression of esmotelin, that supposedly plays a role in muscle contractile activity by interacting with α-MLA in the outer layer of the muscularis propria, may have implications in the pathogenesis of colic inertia in some patients. 30
What is the role of interstitial cells in Cajal?
Interstitial cells of Cajal are considered as intestinal pacemakers, playing a critical role in the regulation of spontaneous electrical activity (“ slow waves and enteric transmission”). These cells can be found particularly at the level of mucosa and myenteric plexus.
What is the purpose of colonoscopy?
Colonoscopy allows a structural evaluation of the colon and excludes anatomical/mechanical causes of constipation. This test should be done particularly if the patient has warning symptoms, shows a sudden onset of constipation, or if is aged over 50 and have never done a colorectal cancer screening.
Which phase of the menstrual cycle is the colonic transit?
Role of progesterone. There is evidence that colonic transit is more intense during the luteal phase of the menstrual cycle, and that the speed of propagation of phase III of the migrating motor complex is slowed in women.
Do laxatives cause abdominal pain?
While laxatives have a significant impact on the frequency and form of the stool, these drugs have little effect on abdominal pain, sense of abdominal distension, the feeling of complete evacuation, and efforts made to defecate (which may suggest the presence of a concurrent defecatory obstruction).
Is total colonic inertia a constipation?
Total colonic inertia is manifested as constipation and is difficult to treat. The results of medical and surgical treatment are not satisfactory, and the need for other therapeutic modalities is warranted. The current study may shed some light on the treatment of colonic inertia with colonic pacing.
Is colonic motility a function of electric activity?
Colonic motility is a function of electric activity. Previous studies8-10have associated constipation with impaired colonic motility and abnormal myoelectric activity. In colonic inertia, the absence of electric waves is presumably responsible for the loss of colonic motility and for constipation.
