If other systems get impaired, renal dialysis, liver dialysis, and artificial nutrition and hydration (including total or partial parenteral nutrition) can also be used. The effects of a circulatory collapse vary based on the type of collapse it is.
What is a circulatory collapse?
A circulatory collapse is defined as a general or specific failure of the circulation, either cardiac or peripheral in nature.
How can I reduce my chances of a collapsed lung?
Anyone can take steps to reduce your chances of collapsed lung: 1 Stop smoking. 2 Avoid or limit activities with drastic changes in air pressure (scuba diving and flying). Follow your provider’s... 3 See your provider regularly to monitor any lung conditions. More ...
Should I go to the ER for a collapsed lung?
A collapsed lung can have many signs and symptoms. If you have symptoms of a collapsed lung, go to the emergency room. You may need immediate care. Signs of a collapsed lung include: Chest pain on one side especially when taking breaths. Cough.
What are the treatment options for atelectasis of the lungs?
Compression of lung caused by pneumothorax, hydrothorax, or hemothorax. Bronchial hygiene, postural drainage, and percussion are used to assist in mucus removal for those patients with atelectasis due to mucus plugging. Bronchoscopy may also be useful in these patients.
What causes a circulatory collapse?
Peripheral collapses usually involve abnormally low blood pressure and result in collapsed arteries and/or veins, leading to oxygen deprivation to tissues, organs, and limbs. Acute collapse can result from heart failure causing the primary vessels of the heart to collapse, perhaps combined with cardiac arrest.
How would you manage circulatory collapse in ICU?
Infusion. Intravenous fluids are the first-line agents for the treatment of patients with circulatory collapse. Repletion of the intravascular volume to increase CO is necessary to improve tissue perfusion in most types of shock.
What happens if your circulatory system shuts down?
When the heart stops, the lack of oxygen-rich blood can cause death or permanent brain damage within minutes.
When is dobutamine used?
Dobutamine stimulates heart muscle and improves blood flow by helping the heart pump better. Dobutamine is used short-term to treat cardiac decompensation due to weakened heart muscle. Dobutamine is usually given after other heart medicines have been tried without success.
How is shock treated in hospital?
Doctors may prescribe the following medications to treat shock: Drugs that increase pressure in the arteries and help the heart pump more blood, such as dopamine, dobutamine, and norepinephrine. Medications to either dilate or constrict blood vessels (depending on the cause of shock)
Is there medication for poor circulation?
Pentoxifylline is used to improve blood flow in patients with circulation problems to reduce aching, cramping, and tiredness in the hands and feet. It works by decreasing the thickness (viscosity) of blood.
What are the symptoms of circulatory failure?
Common symptoms include:numbness and tingling in the hands and feet.cold hands and feet.swelling in the feet, ankles, and legs.memory loss and difficulty concentrating.digestive issues.fatigue.joint and muscle cramping.skin color changes.More items...
What are the first signs of your body shutting down?
Signs that the body is actively shutting down are:abnormal breathing and longer space between breaths (Cheyne-Stokes breathing)noisy breathing.glassy eyes.cold extremities.purple, gray, pale, or blotchy skin on knees, feet, and hands.weak pulse.changes in consciousness, sudden outbursts, unresponsiveness.
What is a circulatory collapse?
A circulatory collapse is defined as a general or specific failure of the circulation, either cardiac or peripheral in nature.
What causes a heart to collapse?
Acute collapse can result from heart failure causing the primary vessels of the heart to collapse, perhaps combined with cardiac arrest .
What is the term for a heart failure that affects the arteries and veins?
Cardiac circulatory collapse affects the vessels of the heart such as the aorta and is almost always fatal. It is sometimes referred to as "acute" circulatory failure. Peripheral circulatory collapse involves outlying arteries and veins in the body and can result in gangrene, organ failure or other serious complications.
What is collapse in medical terms?
collapse. 1. a state of extreme prostration and depression, with failure of circulation. 2. abnormal falling in of the walls of a part or organ. circulatory collapse shock (def. 2). Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc.
What is the treatment for atelectasis?
Treatment. Bronchial hygiene, postural drainage, and percussion are used to assist in mucus removal for those patients with atelectasis due to mucus plugging. Bronchoscopy may also be useful in these patients. Chest tubes are inserted to drain air or fluid from the pleural cavity when present.
Why is fluid therapy important for shock?
Fluid Resuscitation. Fluid therapy to improve microvascular blood flow and increase cardiac output is an essential part of the treatment of any form of shock. Even patients with cardiogenic shock may benefit from fluids, since acute edema can result in a decrease in the effective intravascular volume.
How many phases of shock therapy are there?
There are essentially four phases in the treatment of shock, and therapeutic goals and monitoring need to be adapted to each phase ( Figure 3 ). In the first (salvage) phase, the goal of therapy is to achieve a minimum blood pressure and cardiac output compatible with immediate survival.
What is the goal of resuscitation?
The primary goal of resuscitation should be not only to restore blood pressure but also to provide adequate cellular metabolism, for which the correction of arterial hypotension is a prerequisite. Restoring a mean systemic arterial pressure of 65 to 70 mm Hg is a good initial goal, but the level should be adjusted to restore tissue perfusion, assessed on the basis of mental status, skin appearance, and urine output, as described above. In patients with oliguria, in particular, the effects of a further increase in arterial pressure on urine output should be assessed regularly, unless acute renal failure is already established. Conversely, a mean arterial pressure lower than 65 to 70 mm Hg may be acceptable in a patient with acute bleeding who has no major neurologic problems, with the aim of limiting blood loss and associated coagulopathy, until the bleeding is controlled.
What is shock in ICU?
Shock is the clinical expression of circulatory failure that results in inadequate cellular oxygen utilization. Shock is a common condition in critical care, affecting about one third of patients in the intensive care unit (ICU). 1 A diagnosis of shock is based on clinical, hemodynamic, and biochemical signs, which can broadly be summarized ...
Can you use vasopressors while resuscitating?
It is acceptable practice to administer a vasopressor temporarily while fluid resuscitation is ongoing, with the aim of discontinuing it, if possible, after hypovolemia has been corrected.
How to prevent a collapsed lung?
Anyone can take steps to reduce your chances of collapsed lung: Stop smoking. Avoid or limit activities with drastic changes in air pressure ( scuba diving and flying).
How to prevent lung from collapsing again?
Your provider makes an incision and inserts a tube. Then your provider uses chemicals (such as doxycycline or talc) to attach the lung to the chest cavity, eliminating extra space in the chest cavity.
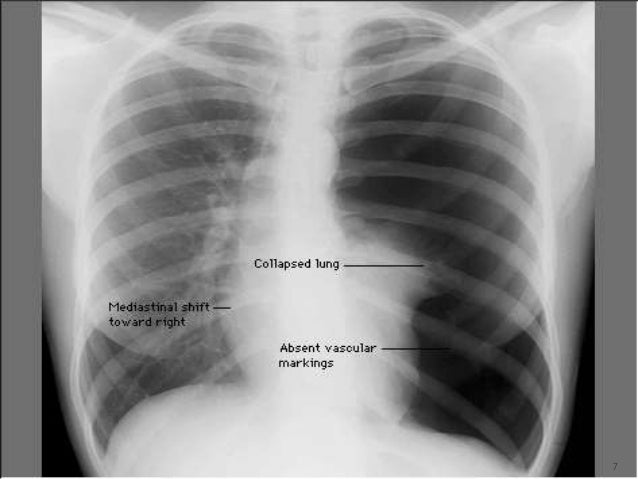
What is a collapsed lung?
A collapsed lung occurs when air enters the pleural space, the area between the chest wall and the lung. Air in the pleural space can build up and press against the lung, causing it to collapse partially or fully. Also called a deflated lung or pneumothorax, a collapsed lung needs immediate medical care.
What is video assisted thoracoscopic surgery?
Surgery: Video-assisted thoracoscopic surgery (VATS) is a minimally invasive procedure that uses a small camera to help the surgeon remove lung tissue. Your surgeon may also perform a chemical pleurodesis or a mechanical pleurodesis using a piece of gauze to attach the lung to the chest cavity.
What is the condition where the lung collapses?
Endometrial tissue lines the uterus. With endometriosis, it grows outside the uterus and attaches to an area inside the chest. The endometrial tissue forms cysts that bleed into the pleural space, causing the lung to collapse.
What are the factors that contribute to a collapsed lung?
Stab wound. Lifestyle factors associated with collapsed lung are: Drug use, especially inhaled drugs. Flying that involves drastic changes in air pressure. Scuba or deep-sea diving. Smoking. People with certain other risk factors may be more likely to have a collapsed lung. These are: Family history of pneumothorax.
Why does my lungs collapse?
It can occur due to abnormal air sacs in the lungs that break apart and release air. Secondary spontaneous pneumothorax: Several lung diseases may cause a collapsed lung. These include chronic obstructive pulmonary disease (COPD), cystic fibrosis and emphysema.