Healthline.com
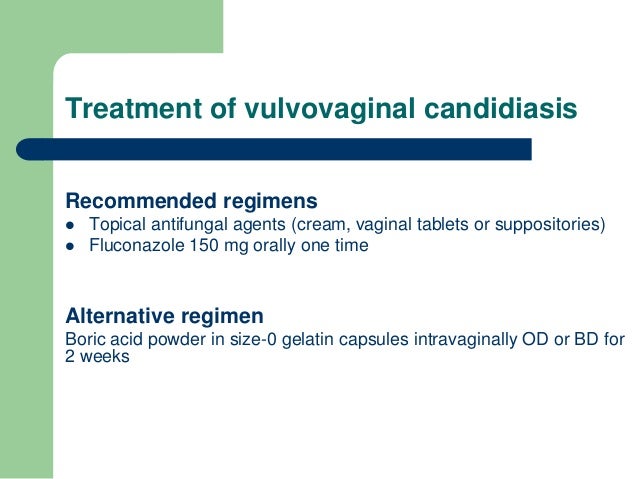
Treatment with azoles results in relief of symptoms and negative cultures in 80%–90% of patients who complete therapy. Recommended Regimens for Vulvovaginal Candidiasis Over-the-Counter Intravaginal Agents Clotrimazole 1% cream 5 g intravaginally daily for 7–14 days OR Clotrimazole 2% cream 5 g intravaginally daily for 3 days OR
Medicalnewstoday.com
It is treated with oral or topical metronidazole or clindamycin. Patients with trichomoniasis usually complain of profuse, yellow-green discharge and vaginal or vulvar irritation. The standard treatment is a single 2 gram dose of oral metronidazole for both the …
Top10homeremedies.com
Jul 21, 2021 · Acute candidal vulvovaginitis is treated with antifungal agents. Since most cases of candidal vulvovaginitis are secondary to C. albicans species, and since C. albicansdoes not have significant resistance to azole antifungals, these are the agents of choice for this disease.
Tinyqualityhomes.org
Treatment of Candidal Vaginitis Antifungal drugs (oral fluconazole in a single dose preferred) Avoidance of excess moisture accumulation Keeping the vulva clean and wearing loose, absorbent cotton clothing that allows air to circulate can …
How can I treat vaginitis at home?
Vaginal imidazole should be applied at night for candidal vulvovaginitis treatment. Other preparations are also effective on candidiasis. Recurrent candidiasis treatment. If candidiasis reoccurs after treatment before 6 months are over, vaginal swabs should be taken; a laboratory test confirmation to manage the suspected infection is also vital.
What is the best treatment for recurent vaginal candidiasis?
Dec 22, 2021 · For this type of vaginitis, your health care provider might prescribe metronidazole tablets (Flagyl) that you take by mouth or metronidazole gel (MetroGel) that you apply to the affected area. Other treatments include clindamycin (Cleocin) cream that you apply to your vagina, clindamycin tablets you take by mouth or capsules you put in your vagina.
Are over-the-counter medications available for vulvovaginitis?
Mar 01, 2018 · Bacterial vaginosis is treated with oral metronidazole, intravaginal metronidazole, or intravaginal clindamycin. The diagnosis of vulvovaginal candidiasis is made using a combination of clinical...
Is treatment required to heal bacterial vaginosis?
Jan 20, 2021 · Antifungals available for intravaginal treatment of vaginal candidiasis include: Butoconazole (Femstat, Gynazole-1) Clotrimazole (Gyne-Lotrimin, Mycelex) Miconazole (Monistat) Terconazole (Terazol) Tioconazole (Vagistat-1) An oral antifungal drug, fluconazole (Diflucan), can also be used to treat vaginal candidiasis.

Which antibiotic is best for vaginal candidiasis?
Treatment of vaginal candidiasis usually involves topical or oral antifungals, such as butoconazole, clotrimazole or fluconazole. Symptoms usually resolve quickly, although in more severe cases treatment may be needed for up to two weeks.
Can Candida vaginitis resolve itself?
Can vaginitis go away untreated? It isn't a good idea to wait for vaginitis to disappear unless you know what's causing it. For instance, some mild yeast infections go away on their own, but not all cases do. Bacterial vaginosis usually clears up on its own, but left untreated, it can put you more at risk for STIs.Nov 30, 2021
How long does it take to get rid of candida?
How long does candida die off last? Candida die off symptoms usually clear up in three to 10 days. After symptoms have started, within just a few weeks, you should notice an increase in energy and focus, as well as relief from other symptoms, as endotoxins are cleared from the body.Jan 11, 2022
How long does it take for a yeast infection to go away with fluconazole?
If you have vaginal thrush, balanitis or oral thrush, your symptoms should be better within 7 days of taking fluconazole. If you have a serious fungal infection, ask your doctor how long it will take for fluconazole to start to work. It may be 1 to 2 weeks before it reaches its full effect.Mar 23, 2020
What is the best medicine for vaginal infections?
These treatments include more doses of fluconazole taken by mouth or other medicines applied inside the vagina, such as boric acid , nystatin, or flucytosine.
How common is vaginal candidiasis?
Vaginal candidiasis is common. In the United States, it is the second most common type of vaginal infection after bacterial vaginal infections. 2 An estimated 1.4 million outpatient visits for vaginal candidiasis occur annually in the United States. 4 The number of vaginal candidiasis cases in the United States is unknown.
What is the name of the yeast infection that causes a person to have a swollen mouth and throat
Candidiasis is an infection caused by a yeast (a type of fungus) called Candida. Candida normally lives inside the body (in places such as the mouth, throat, gut, and vagina) and on skin without causing any problems.
How do you know if you have candida?
Although most vaginal candidiasis is mild, some women can develop severe infections involving redness, swelling, and cracks in the wall of the vagina. Contact your healthcare provider if you have any of these symptoms.
What is the name of the yeast infection in the vagina?
Candidiasis in the vagina is commonly called a “vaginal yeast infection.”. Other names for this infection are “vaginal candidiasis,” “vulvovaginal candidiasis,” or “candidal vaginitis.”.
What are some examples of weakened immune systems?
Have a weakened immune system (for example, due to HIV infection or medicines that weaken the immune system, such as steroids and chemotherapy ) Are taking or have recently taken antibiotics.
Can cotton underwear cause yeast infection?
Wearing cotton underwear might help reduce the chances of getting a yeast infection. 2 Because taking antibiotics can lead to vaginal candidiasis, take these medicines only when prescribed and exactly as your healthcare provider tells you. Learn more about when antibiotics work and when they should be avoided.
What is recurrent candida?
Patients with recurrent candidal vulvovaginitis (defined as four or more episodes of culture-proven candidal vulvovaginitis) have predisposing genetic factors that cause them to be susceptible to recurrent fungal infections. These factors may also predispose to a hypersensitivity to Candida. Pathophysiology.
What is vulvovaginitis?
Vulvovaginitis, or inflammation of the vulva and vagina, most commonly occurs in reproductive-aged women and is usually secondary to infection. Candidal vulvovaginitis is responsible for about one-third of cases. This activity reviews the evaluation and management of candidal vulvovaginitis and highlights the role of interprofessional team members ...
How long does fluconazole last?
Patients with recurrent candidal vulvovaginitis may benefit from suppressive therapy with weekly oral fluconazole for 6 months. Pregnant patients should not be given oral antifungals. In these patients, a 7-day course of intravaginal therapy is appropriate. Fluconazole is considered safe in breastfeeding women.
What is the cause of Candida albicans?
[1][2][3][4] Etiology. Candidal vulvovaginitis is caused by inflammatory changes in the vaginal and vulvar epithelium secondary to infection with Candidaspecies, most commonly Candida albicans.
Is vulvovaginitis common in women?
Candidal vulvovaginitis is common. It is responsible for a third of all cases of vulvovaginitis in reproductive-aged women, and 70% of women report having had candidal vulvovaginitis at some point in their lifetimes. About 8% of women suffer recurrent candidal vulvovaginitis.
What is the most common pathogen in the world?
The most common responsible pathogen is C. albicans (in about 90% of cases), with most of the remaining cases caused by Candida glabrata. It is important to recognize that detailed epidemiological data is not available for this disease process.
Is C. albicans resistant to azole?
Since most cases of candidal vulvovaginitis are secondary to C. albicans species, and since C. albicansdoes not have significant resistance to azole antifungals, these are the agents of choice for this disease.
What is candida vaginal infection?
Candidal vaginitis is vaginal infection with Candida species, usually C. albicans. (See also Overview of Vaginitis .) Most fungal vaginitis is caused by C. albicans ( candidiasis ), which colonizes 15 to 20% of nonpregnant and 20 to 40% of pregnant women. Risk factors for candidal vaginitis include the following: Diabetes.
What are the symptoms of a vaginal discharge?
Symptoms and signs increase the week before menses. Erythema, edema, and excoriation are common.
Is fluconazole over the counter?
Topical butoconazole, clotrimazole, miconazole, and tioconazole are available over the counter.
How long does clotrimazole last?
Clotrimazole. 1% cream 5 g once a day for 7 to 14 days or 2% cream 5 g for 3 days. Miconazole. 2% cream 5 g once a day for 7 days or 4% cream 5 g for 3 days. Vaginal suppository 100 mg once a day for 7 days or 200 mg once a day for 3 days or 1200 mg, only once. Terconazole.
When was the Merck Manual first published?
The Merck Manual was first published in 1899 as a service to the community. The legacy of this great resource continues as the Merck Manual in the US and Canada and the MSD Manual outside of North America. Learn more about our commitment to Global Medical Knowledge.
What is Merck and Co?
Merck & Co., Inc., Kenilworth, NJ, USA is a global healthcare leader working to help the world be well. From developing new therapies that treat and prevent disease to helping people in need, we are committed to improving health and well-being around the world. The Merck Manual was first published in 1899 as a service to the community.
What is the cause of vulvovaginal candidiasis?
Vulvovaginal candidiasis is caused by a pathogen called Candida albicans. Other pathogens include Candida glabrata and Candida tropicalis. Candida species cause yeast vaginitis more than C. albicans. Recurrent infections can be brought about by resistance of the non-C. albicans to anti-fungal treatment.
How many episodes of vulvovaginal candidiasis are there in one year?
If 4 specific episodes of vulvovaginal candidiasis occur within one year, it is considered to be recurrent. If 3 episodes that are not associated with antibiotics happen in one year, it might also be considered to be recurrent. More than 50% of women above 25 years contract vulvovaginal candidiasis. Less than 5% of the women get an infection again. Testing of vulvovaginal candidiasis is, however, vital. Women who self-diagnose are likely to skip concurrent infections or other causes.
How long does it take for candida to reoccur?
If candidiasis reoccurs after treatment before 6 months are over, vaginal swabs should be taken; a laboratory test confirmation to manage the suspected infection is also vital. However, the treatment recommended is seven days of vaginal imidazole.
How to treat swollen epithelium?
Special care and hygiene has to be practiced by using normal saline. Avoid soap, over-the-counter preparations, and home remedies. Use cotton to apply saline, then pat dry using a soft cloth.
What is the best medicine for bacterial vaginosis?
Bacterial vaginosis. For this type of vaginitis, your doctor may prescribe metronidazole (Flagyl) tablets that you take by mouth or metronidazole (MetroGel) gel or clindamycin (Cleocin) cream that you apply to your vagina. You'll need to get tested and be given a prescription for these medications. Yeast infections.
What is the best medicine for yeast infections?
Yeast infections. Yeast infections usually are treated with an over-the-counter antifungal cream or suppository, such as miconazole (Monistat 1), clotrimazole, butoconazole or tioconazole (Vagistat-1). Yeast infections may also be treated with a prescription oral antifungal medication, such as fluconazole (Diflucan).
How to diagnose vaginal infection?
This includes your history of vaginal or sexually transmitted infections. Perform a pelvic exam. During the pelvic exam, your doctor may use an instrument (speculum) to look inside your vagina for inflammation and abnormal discharge. Collect a sample for lab testing.
Can you take fluconazole for yeast infection?
Yeast infections may also be treated with a prescription oral antifungal medication, such as fluconazole (Diflucan). The advantages of over-the-counter treatment are convenience, cost and not waiting to see your doctor. However, you might have something other than a yeast infection.
Can estrogen be used for menopause?
Genitourinary syndrome of menopause (vaginal atrophy). Estrogen — in the form of vaginal creams, tablets or rings — can effectively treat this condition. This treatment is available by prescription from your doctor, after other risk factors and possible complications are reviewed. Noninfectious vaginitis.
What is the treatment for bacterial vaginosis?
Treatment of bacterial vaginosis is recommended for resolving symptoms, as well as reducing the risk of Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, human immunodeficiency virus (HIV), and herpes simplex virus type 2 infections. 37 Shifts in vaginal flora have been associated with increased risk of these infections, leading researchers to conclude that treatment of bacterial vaginosis may decrease susceptibility to these infections. 38, 39
What causes vaginal candidiasis?
The most common causes of vaginitis are bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis. Bacterial vaginosis is the cause in 40% to 50% of cases in which a cause is identified, with vulvovaginal candidiasis accounting for 20% to 25% and trichomoniasis for 15% to 20% of cases.
What are the symptoms of vaginal symtoms?
Vaginitis is characterized by vaginal symptoms, including discharge, odor, itching, irritation, or burning. 1 Most women have at least one episode of vaginitis during their lives, 2 making it the most common gynecologic diagnosis in primary care. Studies have shown a negative effect on quality of life in women with vaginitis, ...
What are office based tests for vaginal fluid?
Office-based tests include microscopy, measurement of vaginal pH, and whiff test. A speculum is not required for collecting vaginal fluid samples for these tests. 17 Several studies have demonstrated a strong correlation between samples from patient self-collected swabs and those collected by clinicians for the diagnosis of bacterial vaginosis, with sensitivities of 70% to 100% and specificities of 97% to 100%. 18 – 22 It is reasonable to conclude that samples for office-based microscopy and laboratory testing for other causes of vaginitis can be collected by patients as well. Patients should be instructed to insert the swab at least one inch into the vagina.
What is the best treatment for trichomoniasis?
Trichomoniasis is treated with oral metronidazole or tinidazole, and patients' sex partners should be treated as well.
Does antibiotic treatment prevent preterm birth?
A 2013 meta-analysis showed that oral or topical antibiotic treatment of bacterial vaginosis in pregnancy does not prevent preterm birth, even in women with a history of preterm labor in previous pregnancies.
What is nucleic acid amplification test?
Nucleic acid amplification testing is recommended for the diagnosis of trichomoniasis in symptomatic or high-risk women. C. 9. Treatment of bacterial vaginosis during pregnancy improves symptoms but does not reduce the risk of preterm birth.
What is the best treatment for candida?
Vaginal candidiasis is treated with antifungal medications. Several are available in the form of creams, suppositories and tablets that can be placed directly in the vagina. Some are available over-the-counter, while others require a prescription.
What causes candida in the vagina?
Vaginal candidiasis is most commonly caused by Candida albicans, a type of yeast, or fungus, that is normally present in the mouth, gut and vagina. It can occasionally be caused by other species of Candida. Our bodies are normally colonized with a variety of organisms, including different bacteria and yeast. These organisms exist in ...
What is the infection of the vagina?
Vaginal candidiasis is an infection of the vagina involving overgrowth of a yeast, or fungus, known as Candida. This yeast is normally present in the mouth, gut and vagina, as are a number of other organisms. If the balance of microorganisms is disrupted, as can occur with taking broad spectrum antibiotics, hormonal fluctuations, ...
How do you know if you have candidiasis?
Common symptoms of vaginal candidiasis include: Itchy feeling in the vagina and the tissue around it (vulva) Pain during sexual intercourse. Pain or burning with urination. Redness and swelling of the vulva. Thick, white vaginal discharge that has a texture similar to cottage cheese.
What is yeast infection?
Vaginal candidiasis, often referred to as a "yeast infection," is a common problem, affecting nearly 75% of adult women in their lifetime (Source: CDC ). Itching and a thick, white discharge are the most common symptoms of vaginal candidiasis. It can also make sexual intercourse and urination painful.
How to reduce candida?
Reducing your risk of vaginal candidiasis. You may be able to lower your risk of vaginal candidiasis by: Avoiding douching. Avoiding products that can irritate the vaginal tissues, such as feminine hygiene sprays, perfumes, powders and soaps.
Can candidiasis be recurrent?
If you have symptoms of vaginal candidiasis, but have never had it before, or if you have a fever or have persistent or recurrent symptoms despite treatment, seek prompt medical care .Women who have symptoms of vaginal candidiasis and are pregnant or are worried about sexually transmitted infections should also seek prompt medical care.
Symptoms of candidal vaginitis
Typical symptoms and manifestations are vaginal or Bulbar pruritus, burning, irritation (which can intensify after sexual intercourse) and abundant, curdled discharge, adhering tightly to the walls of the vagina. Symptoms and signs of the disease are worse in the week before menstruation.
Diagnosis of candidal vaginitis
The diagnostic criteria for candidal vaginitis are: the pH of the vaginal secretion is less than 4.5; detection of yeast, pseudomycelia or mycelium during the test with KOH.
Treatment of candidal vaginitis
Vaginal or oral drugs are highly effective. Improves the condition of a single application of fluconazole at a dose of 150 mg orally. Effective use of pharmaceutical preparations of butoconazole, clotrimazole, miconazole and thioconazole for topical use.

About
Symptoms
Risk & Prevention
- Who gets vaginal candidiasis?
Vaginal candidiasis is common, though more research is needed to understand how many women are affected. Women who are more likely to get vaginal candidiasis include those who: 1. Are pregnant 2. Use hormonal contraceptives (for example, birth control pills) 3. Have diabetes 4. Ha… - How can I prevent vaginal candidiasis?
Wearing cotton underwear might help reduce the chances of getting a yeast infection.2 Because taking antibiotics can lead to vaginal candidiasis, take these medicines only when prescribed and exactly as your healthcare provider tells you. Learn more about when antibiotics workand when t…
Sources
- Scientists estimate that about 20% of women normally have Candida in the vagina without having any symptoms.2 Sometimes, Candidacan multiply and cause an infection if the environment inside the vagina changes in a way that encourages its growth. This can happen because of hormones, medicines, or changes in the immune system.
Diagnosis & Testing
- Healthcare providers usually diagnose vaginal candidiasis by taking a small sample of vaginal discharge to be examined under a microscope in the medical office or sent to a laboratory for a fungal culture. However, a positive fungal culture does not always mean that Candida is causing symptoms because some women can have Candidain the vagina without having any symptoms.
Treatment
- Vaginal candidiasis is usually treated with antifungal medicine.3For most infections, the treatment is an antifungal medicine applied inside the vagina or a single dose of fluconazole taken by mouth. Other treatments may be needed for infections that are more severe, that don’t get better, or that keep coming back after getting better. These treatm...
Statistics
- Vaginal candidiasis is common. In the United States, it is the second most common type of vaginal infection after bacterial vaginal infections.2 An estimated 1.4 million outpatient visits for vaginal candidiasis occur annually in the United States.4 The number of vaginal candidiasis cases in the United States is unknown.