Medication
People with ARDS usually are given medication to:
- Prevent and treat infections
- Relieve pain and discomfort
- Prevent blood clots in the legs and lungs
- Minimize gastric reflux
- Sedate
Therapy
What's Next After ARDS: Long-Term Outcomes
- Abstract. ARDS is a life-threatening organ failure due to several pulmonary and extrapulmonary injuries with an incidence between 5 and 60 cases/100,000 persons/y.
- Introduction. ...
- Long-Term Mortality. ...
- Neuropsychological Disability
- Radiological Findings. ...
- Pulmonary Dysfunction. ...
- Summary. ...
- Footnotes. ...
- References. ...
Nutrition
You can take steps to recover from ARDS and improve your quality of life. Ask your family and friends to help with everyday activities. Don't smoke and avoid secondhand smoke and other lung irritants, such as harmful fumes. Go to pulmonary rehabilitation if your doctor recommends it. Join a support group for ARDS.
See more
There is no cure for ARDS at this time. Treatment focuses on supporting the patient while the lungs heal. The goal of supportive care is getting enough oxygen into the blood and delivered to your body to prevent damage and removing the injury that caused ARDS to develop. All patients with ARDS will require extra oxygen.
How Ards should be treated?
How to recover from ARDS?
Can You recover from ARDS?
Can Ards be cured?

How do doctors treat ARDS?
No specific therapy for ARDS exists. Treatment is primarily supportive using a mechanical respirator and supplemental oxygen. Intravenous fluids are given to provide nutrition and prevent dehydration and are carefully monitored to prevent fluid from accumulating in the lungs (pulmonary edema).
What medications are used to treat a patient with ARDS?
Statins and aspirin are the two kinds of most studied medicine to prevent patients at high risk from turning into ARDS. Statins are proved to have the effects of immunomodulatory and anti-inflammatory which can be used against ARDS. Shyamsundar et al.
What are the chances of surviving ARDS?
Prognosis. The survival rate for patients with COVID-19 with ARDS is approximately 25%. Factors associated with increased mortality in patients with COVID-19 pneumonia included age ≥65 years, presence of cardiovascular or cerebrovascular disease, lymphopenia, and elevation in troponin I levels.
What is ARDS and how is it treated?
Acute respiratory distress syndrome (ARDS) is a serious lung condition that causes low blood oxygen. People who develop ARDS are usually ill due to another disease or a major injury. In ARDS, fluid builds up inside the tiny air sacs of the lungs, and surfactant breaks down.
Can a person recover from ARDS?
It is important to note that most people survive ARDS. They will not require oxygen on a long-term basis and will regain most of their lung function. Others will struggle with muscle weakness and may require re-hospitalization or pulmonary rehabilitation to regain their strength.
How long does it take to recover from Covid ARDS?
Lasting effects can include: Difficulty breathing. It can take up to two years for people recovering from ARDS to regain lung function. A physical therapist can help patients maximize their lung capacity.
What are the 4 phases of ARDS?
In ARDS, the injured lung is believed to go through three phases: exudative, proliferative, and fibrotic, but the course of each phase and the overall disease progression is variable.
How long can a person be on a ventilator in an ICU?
Some people may need to be on a ventilator for a few hours, while others may require one, two, or three weeks. If a person needs to be on a ventilator for a longer period of time, a tracheostomy may be required.
How long can a person survive on a ventilator?
Results: On average, patients had a hospital stay of almost 6 weeks and required mechanical ventilation for approximately 4 weeks; 43.9% of the patients died in the hospital.
What is the difference between pneumonia and ARDS?
The diagnoses of ARDS and pneumonia both require radiographic infiltrates; severe pneumonia is frequently of acute onset and shows bilateral infiltrates on chest radiography and severe acute respiratory failure not due to cardiac failure.
What is the most common cause of ARDS?
Sepsis may be the most common cause of ARDS that develops several days or more after severe trauma or burns. Massive traumatic tissue injury may directly precipitate or predispose a patient to ARDS [65,68].
How do you remove fluid from the lungs?
Thoracentesis is a procedure to remove fluid or air from around the lungs. A needle is put through the chest wall into the pleural space. The pleural space is the thin gap between the pleura of the lung and of the inner chest wall.
What to do if you have ARDS?
If you have symptoms of depression, such as hopelessness and loss of interest in your usual activities, tell your doctor or contact a mental health professional. Depression is common in people who have had ARDS, and treatment can help. By Mayo Clinic Staff. Symptoms & causes Doctors & departments. June 13, 2020.
How to diagnose ARDS?
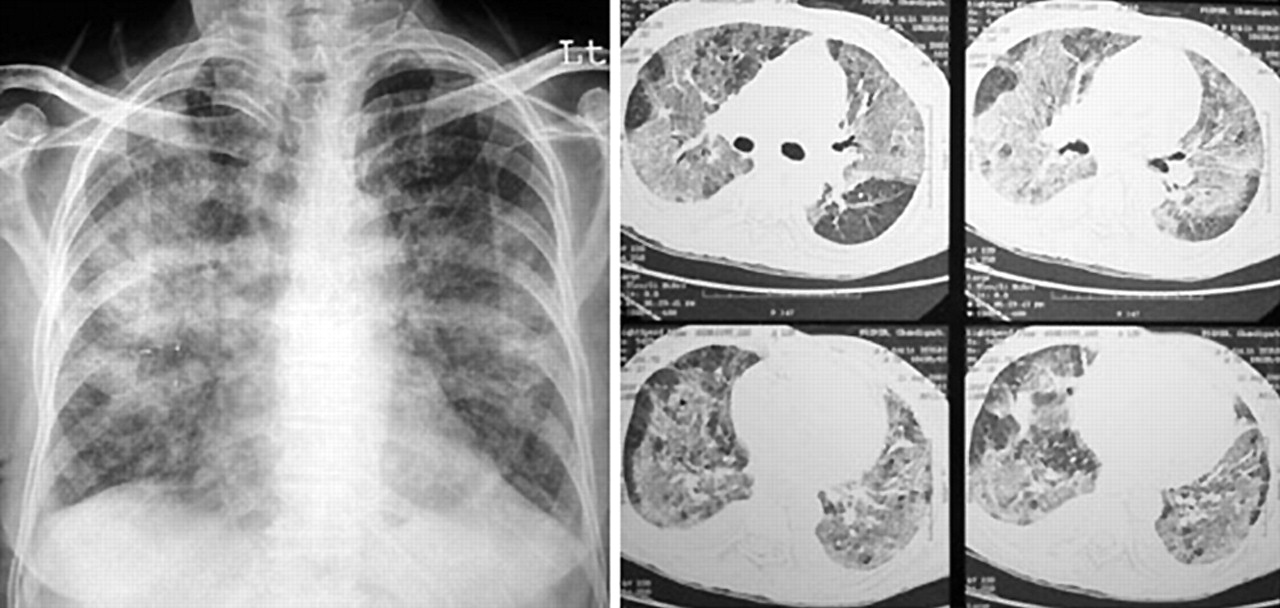
There's no specific test to identify ARDS. The diagnosis is based on the physical exam, chest X-ray and oxygen levels. It's also important to rule out other diseases and conditions — for example, certain heart problems — that can produce similar symptoms.
What is the first goal of ARDS?
The first goal in treating ARDS is to improve the levels of oxygen in your blood. Without oxygen, your organs can't function properly.
What is the best test for ARDS?
Because the signs and symptoms of ARDS are similar to those of certain heart problems, your doctor may recommend heart tests such as: Electrocardiogram. This painless test tracks the electrical activity in your heart. It involves attaching several wired sensors to your body. Echocardiogram.
How to protect your lungs from ARDS?
If you're recovering from ARDS, the following suggestions can help protect your lungs: Quit smoking. If you smoke, seek help to quit, and avoid secondhand smoke whenever possible. Get vaccinated. The yearly flu (influenza) shot, as well as the pneumonia vaccine every five years, can reduce your risk of lung infections.
How to help someone with lung problems?
Join a support group. There are support groups for people with chronic lung problems. Discover what's available in your community or online and consider joining others with similar experiences.
Can you recover from ARDS?
Recovery from ARDS can be a long road, and you'll need plenty of support. Although everyone's recovery is different, being aware of common challenges encountered by others with the disorder can help. Consider these tips:
How is ARDS treated?
ARDS is usually treated in the intensive care unit (ICU) along with treatment of the underlying cause. Mechanical ventilation (a ventilator) is often used in caring for patients with ARDS. For milder cases of ARDS, oxygen may be given through a fitted face mask or a cannula fitted over the nose.
What is ARDS in medical terms?
Acute Respiratory Distress Syndrome (ARDS) Acute respiratory distress syndrome (ARDS) is a life-threatening lung injury caused by sepsis, pneumonia, the coronavirus (COVID-19) and other conditions. ARDS tends to develop within few hours to few days of the event that caused it, and can worsen rapidly. ARDS patients may have to be put in an intensive ...
What causes ARDS in the lungs?
ARDS is caused when fluids leak from small lung vessels into lung air sacs (alveoli). When the protective membrane between blood vessels and air sacs is compromised, levels of oxygen in the blood decrease. Causes of ARDS include: Sepsis: The most common cause of ARDS, a serious infection in the lungs ...
What is the most common cause of ARDS?
Sepsis: The most common cause of ARDS, a serious infection in the lungs (pneumonia) or other organs with widespread inflammation. Aspiration pneumonia: Aspiration of stomach contents into the lungs may cause severe lung damage and ARDS. The coronavirus (COVID-19): The infection COVID-19 may develop into severe ARDS.
What is the name of the virus that can cause severe ARDS?
The coronavirus (COVID-19): The infection COVID-19 may develop into severe ARDS.
Where does ARDS happen?
ARDS typically happens in hospital settings while the patient is being treated for infection or trauma. If you’re not hospitalized and experience symptoms of ARDS, get medical attention immediately.
When do complications develop from ARDS?
Complications and problems from ARDS may develop while a patient is in the hospital or after discharge.
What is the best treatment for ARDS?
Supplemental oxygen – ensures the body is getting enough oxygen in the lungs and the blood. Mechanical ventilator – supports the work it takes to breath with ARDS. Sedation— intravenous medications are used to induce sedation or coma, if needed, to help the patient breath.
How long does it take to recover from ARDS?
Recovery after being treated for ARDS in an ICU can be weeks to months. Acute Respiratory Distress Syndrome (ARDS): Diagnosis.
How is acute respiratory distress syndrome treated?
How is of acute respiratory distress syndrome (ARDS) treated? Treating acute respiratory distress syndrome includes addressing any lung damage or other injury, and helping the patient breathe consistently while the lungs heal and the body fights the infection.
What is the best treatment for ARDS?
Antibiotics to treat infection. Anti-inflammatory drugs, such as cortico steroids, to reduce inflammation in the lungs in the late phase of ARDS or sometimes if the person is in septic shock. Diuretics to eliminate fluid from the lungs. Drugs to counteract low blood pressure that may be caused by shock.
What is ARDS in medical terms?
Acute respiratory distress syndrome (ARDS) is characterized by the development of sudden breathlessness within hours to days of an inciting event. Inciting events include: trauma, sepsis (microorganisms growing in a person's blood), drug overdose, massive transfusion of blood products, acute pancreatitis, or.
What is AP in X-rays?
This anteroposterior (AP) portable chest X-ray film shows an endotracheal tube, left subclavian central venous catheter into the superior vena cava, and bilateral patchy opacities in mostly the middle and lower lung zones. The person had been in respiratory failure for 1 week with the diagnosis of ARDS
What is ARDS in lungs?
ARDS is associated with severe and diffuse injury to the alveolar-capillary membrane (the air sacs and small blood vessels) of the lungs. Fluid accumulates in some alveoli of the lungs, while some other alveoli collapse.
How long does it take for ARDS to develop?
ARDS typically develops within 12-48 hours after the inciting event, although, in rare instances, it may take up to a few days. Persons developing ARDS are critically ill, often with multisystem organ failure. It is a life-threatening condition; therefore, hospitalization is required for prompt management.
How long has the outlook for ARDS been good?
Outlook of persons with ARDS has improved over the last 20 years and a majority of people survive. Persons with a poor outlook include those older than 65 years and those with sepsis as the underlying cause. The adverse effect of age may be related to the underlying health status.
Why do you need a pulmonary artery catheter?
Monitoring with a pulmonary artery catheter may be done to exclude a cardiac cause for the difficulty in breathing.
Why do doctors check for ARDS?
Because ARDS is a disease of the lungs, the physical exam centers on evaluating lung function. A doctor will listen to the lungs , using a stethoscope to check for characteristic crackling sounds produced by fluid-filled lungs.
What is ARDS in medical terms?
Though it has become part of a vocabulary around COVID-19, the term Acute Respiratory Distress Syndrome , or ARDS for short, refers to a type of lung damage that can result from a variety of causes, including illness, trauma, or even as a complication that occurs following certain medical procedures. ARDS is a dangerous, potentially fatal respiratory condition in which the lungs sustain a serious, widespread injury that diminishes their ability to provide the body’s organs with enough oxygen. The condition causes fluid to accumulate in the lungs, which in turn reduces blood oxygen to dangerously low levels. ARDS is a medical emergency.
Why is ARDS called acute?
The term “acute” appears in the name of ARDS, because the condition arises from a recent injury to the lungs. It is characterized by the accumulation of fluid in the lungs and below-normal levels of oxygen in the blood (the medical term for this is hypoxemia). While a variety of medical conditions may lead to ARDS, ...
How long does it take for ARDS to develop?
The first symptoms of ARDS usually develop within a few hours to a week after lung injury. People typically experience extreme difficulty breathing and shortness of breath. This is often accompanied by rapid, shallow breathing.
How many people get ARDS each year?
ARDS is always caused by an injury to the lungs, whether from illness or injury, but it can affect people of any age. In fact, in the United States, about 190,000 Americans are diagnosed with ARDS each year.
What are the lungs that are affected by ARDS?
While a variety of medical conditions may lead to ARDS, at a microscopic level they all result in damage to air sacs in the lungs (called alveoli) and the tiny neighboring blood vessels (called capillaries).
Does ARDS cause immune system problems?
What’s more, ARDS also triggers an immune response.
What is ARDS ventilation?
ARDS is a heterogeneous process within the lungs in which some alveoli will never inflate, some will open and close cyclically while others will be continuously distended and damaged.13Ther efore , the effective lung being ventilated is much smaller than usual and is termed ‘baby lung’. The primary mechanism of VILI is tidal hyperinflation of the ‘baby lung’ and cyclic atelectasis of already injured lung units.14Low tidal volume ventilation to prevent tidal hyperinflation and application of positive end expiratory pressure (PEEP) to improve hypoxemia and limit cyclic atelectasis are the key aspects of lung protective ventilation in ARDS.15Multiple other aspects of mechanical ventilation such as modes of ventilation,16, 17, 18, 19recruitment maneuvers,20,21higher versus lower PEEP22have all been studied and described below. The current recommendations for mechanical ventilation in ARDS are represented in Table 2.
What is ARDS in medical terms?
Acute respiratory distress syndrome (ARDS) is a clinically and biologically heterogeneous disorder associated with a variety of disease processes that lead to acute lung injury with increased non-hydrostatic extravascular lung water, reduced compliance, and severe hypoxemia. Despite significant advances, mortality associated with this syndrome remains high. Mechanical ventilation remains the most important aspect of managing patients with ARDS. An in-depth knowledge of lung protective ventilation, optimal PEEP strategies, modes of ventilation and recruitment maneuvers are essential for ventilatory management of ARDS. Although, the management of ARDS is constantly evolving as new studies are published and guidelines being updated; we present a detailed review of the literature including the most up-to-date studies and guidelines in the management of ARDS. We believe this review is particularly helpful in the current times where more than half of the acute care hospitals lack in-house intensivists and the burden of ARDS is at large.
What is lung protective ventilation?
Lung protective ventilation is the cornerstone of ARDS management. The ARDSnet study published in 2000 was the most influential trial to demonstrate the clinical value of low tidal volume ventilation.23This randomized control trial involving 861 patients showed significantly reduced mortality (31% vs. 39.8%, p = 0.007) in patients treated with lower tidal volumes (mean tidal volumes of 6.2 ± 0.8 mL per Kg of predicted body weight) compared to patients treated with traditionally high volumes (11.8 ± 0.8 mL per Kg of predicted body weight). The mean plateau pressures were 25 ± 6 and 33 ± 8 cmH2O (p < 0.001), respectively. Subsequently, a meta-analysis of six randomized control studies comparing ventilation using tidal volume of 7 mL/Kg or less versus ventilation that used tidal volume of 10–15 mL/Kg showed that in 1297 patients with ARDS, the 28-day mortality was significantly lower in low tidal volume group compared to high tidal volume group (27.3% vs 36.9%).24Furthermore, the mortality rate in the control group was not significantly different if a plateau pressure of 31 cmH2O or less was maintained.
How long does it take for corticosteroids to be administered?
In conclusion, early administration of corticosteroids within 14 days of onset of moderate to severe ARDS can reduce the duration of mechanical ventilation and overall mortality and should be considered in such patients provided no contraindications.
What are the mechanisms of ARDS?
The proposed mechanism of these agents includes either decreasing the inflammatory cascade, fastening the recovery of injured alveoli or reducing ventilator dyssynchrony, thus reducing VILI.12Neuromuscular blockers and systemic corticosteroids are the most extensively studied agents in this aspect.
When was acute respiratory distress syndrome first recognized?
Acute respiratory distress syndrome (ARDS) was first recognized as a distinct clinical entity in the 1960s. Ashbaugh presented a case series of twelve patients in respiratory failure with hypoxia and loss of compliance after a variety of clinical insults. These patients did not respond to usual methods of respiratory therapy and positive end-expiratory pressure (PEEP) was most helpful in combating atelectasis and hypoxemia. The clinical and pathological features closely resembled those seen in infants with respiratory distress and hence these patients were described as having acute respiratory distress in adults.1Since then we have made remarkable advances in terms of understanding the disease pathology and more importantly management of patients with ARDS. ARDS affects approximately 200,000 individuals and results in 74,500 deaths per year in the United States and globally about 3 million cases each year. Patients with ARDS represent about 10% of ICU admissions, 25% of patients require mechanical ventilation and mortality ranges from 35% to 46%.2,3
Is PEEP recommended for ARDS?
In summary, while PEEP is recommended in all patients with ARDS, high PEEP may be considered on a case-by-case basis (conditional recommendation) in patients with moderate to severe ARDS.
What is the purpose of the ARDS guidelines?
The purpose of this guideline is to provide an evidence-based framework for the management of adult patients with acute respiratory distress syndrome (ARDS) that will inform both key decisions in the care of individual patients and broader policy. Our recommendations are neither dictates nor standards of care. We cannot take into account all of the features of individual patients and complex local factors; all we can do is to synthesise relevant evidence and to put it into the context of current critical care medicine. Similarly, our recommendations are not comprehensive: these guidelines have relevance to a fraction of the total number of decisions that are required of carers for these complex patients. Indeed, the current state of the art for the management of ARDS has been recently reviewed1–4and comparable guidelines have been produced by national and international stakeholders.5 6
What is the recommended ventilation for ARDS?
The Faculty of Intensive Care Medicine and Intensive Care Society Guideline Development Group have used GRADE methodology to make the following recommendations for the management of adult patients with acute respiratory distress syndrome (ARDS). The British Thoracic Society supports the recommendations in this guideline. Where mechanical ventilation is required, the use of low tidal volumes (<6 ml/kg ideal body weight) and airway pressures (plateau pressure <30 cmH2O) was recommended. For patients with moderate/severe ARDS (PF ratio<20 kPa), prone positioning was recommended for at least 12 hours per day. By contrast, high frequency oscillation was not recommended and it was suggested that inhaled nitric oxide is not used. The use of a conservative fluid management strategy was suggested for all patients, whereas mechanical ventilation with high positive end-expiratory pressure and the use of the neuromuscular blocking agent cisatracurium for 48 hours was suggested for patients with ARDS with ratio of arterial oxygen partial pressure to fractional inspired oxygen (PF) ratios less than or equal to 27 and 20 kPa, respectively. Extracorporeal membrane oxygenation was suggested as an adjunct to protective mechanical ventilation for patients with very severe ARDS. In the absence of adequate evidence, research recommendations were made for the use of corticosteroids and extracorporeal carbon dioxide removal.
What is ARDS in medical terms?
ARDS was first reported in a case series from Denver in 1967.7The American European Consensus Conference (AECC) 1994 defined ARDS as ‘an acute inflammatory syndrome manifesting as diffuse pulmonary oedema and respiratory failure that cannot be explained by, but may co-exist with, left-sided heart failure’.8In 2012, the AECC definition was re-evaluated and minor alterations were proposed by the European Society of Intensive Care Medicine ARDS Definition Task Force. This iteration recognised 3 grades of severity depending on the degree of hypoxaemia and stipulated the application of at least 5 cmH2O of positive end-expiratory pressure (PEEP) or continuous positive airway pressure. This so-called Berlin definition was validated using retrospective cohorts and captures patients with a mortality of 24% in patients with mild ARDS, rising to 48% in the group of patients with the most severe respiratory failure.9
How many people die from ARDS annually?
Using the AECC definition, several population-based studies of ARDS showed a fairly consistent picture of the age, mortality and severity of illness; however, there was almost a fourfold difference in incidence, probably contributed to by differences in study design and ICU utilisation.10In the USA, there are estimated to be 190 000 cases and 74 000 deaths annually from ARDS.11Whereas in a third world setting, from 1046 patients admitted to a Rwandan hospital over 6 weeks, 4% (median age 37 years) met modified ARDS criteria. Only 30.9% of patients with ARDS were admitted to an ICU, and hospital mortality was 50.0%. This study used the Kigali modification of the Berlin definition: without a requirement for PEEP, hypoxia threshold of SpO2/FiO2less than or equal to 315, and bilateral opacities on lung ultrasound or chest radiograph.12
Why is ARDS important?
Therefore, ARDS is important both clinically and financially, because it is a not uncommon contributor to the deaths of critically ill patients of all ages and because survivors carry on suffering from the sequelae of critical illness long after they leave hospital.16
What is the pathophysiology of ARDS?
The pathophysiology of ARDS results from acute inflammation affecting the lung’s gas exchange surface, the alveolar-capillary membrane.1Inc reased permeability of the membrane associated with the recruitment of neutrophils and other mediators of acute inflammation into the airspace manifests as high permeability pulmonary oedema. The resulting acute inflammatory exudate inactivates surfactant leading to collapse and consolidation of distal airspaces with progressive loss of the lung’s gas exchange surface area. This would be compensated for by hypoxic pulmonary vasoconstriction, if the inflammatory process did not also effectively paralyse the lung’s means of controlling vascular tone, thereby allowing deoxygenated blood to cross unventilated lung units on its way to the left heart. The combination of these two processes causes profound hypoxaemia and eventually type 2 respiratory failure as hyperventilation fails to keep pace with carbon dioxide production.
Who created the guidelines for adult patients with ARDS?
The guidelines for the management of adult patients with ARDS were created by a multidisciplinary writing group constituted by the Joint Standards Committee of the Faculty of Intensive Care Medicine and the ICS. All group members, including lay members, are coauthors of the guideline. The group first met in 2013 and completed the guidelines in 2018. The guidelines have undergone both independent external peer review and input from stakeholder organisations.

Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Coping and Support