
What are the treatments for popliteal vein thrombosis?
When patients get proper treatment, the condition will eventually vanish with no long-term consequences. Mostly, the first treatment for popliteal vein thrombosis will be anticoagulant therapy. Anticoagulants, also known as blood thinners, refer to medications that prevent clotting.
How is popliteal artery occlusion (Pao) treated?
Surgical therapy for popliteal artery occlusion involves bypass of the occlusion, which can be achieved with grafts, including great saphenous vein (GSV) or prosthetic (eg, polytetrafluoroethylene [PTFE]) grafts.
What is a blood clot in the popliteal vein?
Sometimes the blood flowing through those veins can form a clot -- a thick clump that can keep blood from getting through smoothly. The medical term for a blood clot is “thrombosis,” and it can be dangerous if it happens in a blood vessel like the popliteal vein.
What is the treatment for blood clots?
Treatment for blood clots depends on where the clot is in the body, and the severity of the condition. Blood-thinning medications are commonly used to prevent blood clots from forming or getting bigger. Thrombolytic medications can break up existing clots.
What would happen if there was a blood clot in the popliteal artery?
It can restrict circulation in your legs. This can cause damage to your blood vessels and the surrounding tissue. A clot can also break loose from the popliteal vein. It can then travel to the right side of the heart and then to the lungs, where it can cause numerous circulation and respiratory problems.
Is popliteal vein thrombosis serious?
Popliteal vein thrombosis happens when a blood clot blocks one of the blood vessels behind your knees. It's a serious condition, but it can sometimes be mistaken for a less-dangerous condition called a Baker's cyst.
How do you treat a blood clot under the knee?
Distal DVT can either be treated with anticoagulation (medicines that help prevent blood clots), with or without additional use of compression stockings, or no medications can be given, and monitoring with repeat ultrasounds can be performed to see if the clots grow, which requires anticoagulation.
How long does it take for a blood clot in the leg to resolve?
Living with DVT It takes about 3 to 6 months for a blood clot to go away. During this time, there are things you can do to relieve symptoms. Elevate your leg to reduce swelling. Talk to your doctor about using compression stockings.
Do you treat popliteal DVT?
Treatment with anticoagulation is the accepted standard of care for DVT involving the proximal leg veins, specifically, the popliteal, femoral, and iliac veins.
What happens if a blood clot does not dissolve?
In addition, when a clot in the deep veins is very extensive or does not dissolve, it can result in a chronic or long-lasting condition called post-thrombotic syndrome (PTS), which causes chronic swelling and pain, discoloration of the affected arm or leg, skin ulcers, and other long-term complications.
How do you dissolve a blood clot in your leg?
Thrombolytics. Thrombolytics are drugs that dissolve blood clots. A doctor may give a thrombolytic intravenously, or they may use a catheter in the vein, which will allow them to deliver the drug directly to the site of the clot. Thrombolytics can increase the risk of bleeding, however.
How do you get rid of a blood clot in your leg?
Anticoagulants: The most common treatment for a blood clot is anticoagulants or blood thinners. They work by reducing the body's ability to form new clots and preventing existing clots from growing larger. Anticoagulants can be given in the form of pills or intravenous injections.
Can a blood clot go away on its own?
Blood clots do go away on their own, as the body naturally breaks down and absorbs the clot over weeks to months. Depending on the location of the blood clot, it can be dangerous and you may need treatment.
What dissolves blood clots fast?
Anticoagulants. Anticoagulants, such as heparin, warfarin, dabigatran, apixaban, and rivaroxaban, are medications that thin the blood and help to dissolve blood clots.
Does a blood clot require hospitalization?
Will you be admitted to the hospital or sent home? If a DVT is confirmed, you may be discharged and sent home with injectable or oral anticoagulant medication (sometimes called a blood thinner). That said, every patient is different, and you may be admitted to the hospital if the ER doctor believes it's necessary.
Can you walk with a blood clot in your leg?
Following a DVT, your leg may be swollen, tender, red, or hot to the touch. These symptoms should improve over time, and exercise often helps. Walking and exercise are safe to do, but be sure to listen to your body to avoid overexertion.
How to prevent popliteal vein thrombosis?
The best way to prevent and recover from popliteal vein thrombosis is to get moving and active. When patients keep their legs still for long periods, the blood flow in the legs becomes sluggish. There is a tendency of blood to pool behind the valves leading to the formation of a clot.
How to prevent blood clots?
Smoking can damage the wall of blood vessels, thus triggering the formation of blood clots. Therefore, one of the solid ways to prevent blood clots is to quit smoking . However, stopping the smoking habit is easier said than done. If someone wants to quit smoking, they can seek professional help for specific advice.
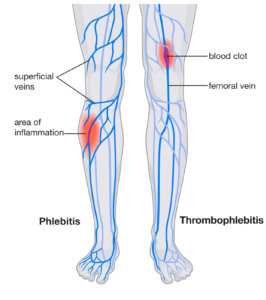
What is the name of the condition where blood carries from the legs to the heart?
Popliteal vein thrombosis is a silent condition that might occur without the patient's knowledge. It is a condition defined by the formation of a clot also known as a thrombus in the popliteal vein . The popliteal vein is a major vein in the lower body that empties blood from the legs and carries it to the heart. The vein is located behind the knee, and it is found deep into the skin. Popliteal vein thrombosis is a form of deep vein thrombosis since it occurs deep into the leg tissue.
How long does blood thinner last?
Blood thinners can either be taken as a pill or an injection under the skin. Anticoagulant therapy usually lasts for six months, and it carries various side effects. The most common side effect of using blood thinners is excessive bleeding. It occurs when the anticoagulants cause excessive thinning of the blood.
Why do you need blood tests for blood thinners?
If a patient is on blood thinners, it is wise for them to have regular blood tests to measure their blood’s clotting ability . The tests will help their doctor to change the dosage for the anticoagulants if need be.
What is the best medication for thrombosis?
Anticoagulants, also known as blood thinners, refer to medications that prevent clotting. Heparin and warfarin are the first two anticoagulants approved for treating thrombosis, though newer anticoagulants such as apixaban, rivaroxaban, and dabigatran have also been approved. A combination of anticoagulants and the natural body’s mechanism will ...
Can you put anticoagulants on popliteal vein thrombosis?
As highlighted earlier, the primary treatment option for popliteal vein thrombosis is anticoagulant therapy. But, remember not everyone can be put on anticoagulants. For instance, if a patient had a major operation or cases of active bleeding, their doctor may recommend the use of a mechanical filter instead of blood thinners. The mechanical filters are used to remove the clots from the blood before they move to the heart and lungs.
Why does popliteal vein thrombosis occur?
Popliteal vein thrombosis can occur due to poor blood flow, damage to a blood vessel, or an external injury. In this article, we explain what popliteal vein thrombosis is and discuss its causes, risk factors, and symptoms. We also cover diagnosis, treatment, complications, and prevention.
What is a blot clot?
The blot clot closes the wound and stops the bleeding, preventing further blood loss and starting the healing process. When a blood clot forms inside a vein or artery, doctors refer to it as a thrombus. A thrombus can develop due to poor blood flow, damage to a blood vessel, or external injury.
What is a blood clot behind the knee?
A blood clot behind the knee is a type of venous thromboembolism. It is a serious condition that can lead to life-threatening complications, such as a pulmonary embolism. The popliteal vein runs behind the knee and transports blood back up to the heart. When a blood clot forms in this vein, doctors refer to it as popliteal vein thrombosis.
When is thrombolytic therapy necessary?
Thrombolytic therapy may be necessary if a person has a very large blood clot or if anticoagulant medications are not working effectively.
What does it feel like to have a blood clot?
a warm area behind the knee or in the leg. pain in the knee or leg, which may feel similar to a cramp. Anyone who suspects that they have a blood clot should see a doctor right away. It is essential to seek immediate medical attention if the following symptoms occur alongside a potential clot: shortness of breath.
How long does it take to take anticoagulant?
A person will initially take an oral anticoagulant once or twice daily for between 5 and 21 days. Doctors may also recommend that a person takes these medications in the long term to prevent future blood clots. Treatment can last for 6 months or longer.
What are the conditions that affect blood clotting?
genetic conditions that affect blood clotting, such as thrombophilia, antiphospholipid syndrome, and sickle cell anemia
What is the best treatment for a clot in the leg?
For patients who are at high risk of developing clots in the deep veins of the legs—also known as deep vein thrombosis (DVT)—preventive measures should be considered. In addition to or instead of blood thinners, intermittent pneumatic compression (IPC) devices can be very effective. A cuff is placed around the leg, where it periodically fills with air and squeezes, helping move blood toward the heart.
How to treat blood clots?
Treatment for blood clots depends on where the clot is in the body, and the severity of the condition. Blood-thinning medications are commonly used to prevent blood clots from forming or getting bigger. Thrombolytic medications can break up existing clots.
Where is a thrombectomy tube used?
Surgical thrombectomy, in which the clot is surgically removed from the vein or artery, is often used in arms or legs, but can be used elsewhere in the body.
Can blood clots cause shortness of breath?
Blood clots can be very serious, so symptoms of blood clots should be evaluated by a doctor immediately. If not treated, a clot can break free and cause a pulmonary embolism—where the clot gets stuck in a blood vessel in the lung, causing severe shortness of breath and even sudden death.
What is the ultrasound used to look for blood clots?
The kind of ultrasound used to look for signs of deep vein blood clots is called venous duplex scanning.
What is the condition called when a blood clot blocks one of the blood vessels behind your knees?
Articles On Popliteal Vein Thrombosis. Popliteal vein thrombosis happens when a blood clot blocks one of the blood vessels behind your knees. It’s a serious condition, but it can sometimes be mistaken for a less-dangerous condition called a Baker’s cyst.
How to treat Baker's cyst?
For a Baker’s cyst, most of your symptoms can be treated with ice and over-the-counter painkillers. If you have popliteal vein thrombosis, you may need medicine to treat the clot before it can cause bigger problems. Share on Facebook Share on Twitter Share on Pinterest Email Print. Pagination.
Is a blood clot dangerous?
The medical term for a blood clot is “thrombosis,” and it can be dangerous if it happens in a blood vessel like the popliteal vein. That’s because blood clots in deep veins can travel to your lungs and block a blood vessel there. That's called a pulmonary embolism, and it can be deadly.
Can a popliteal cyst be a blood clot?
A blood clot in the popliteal vein and a Baker’s cyst have many common symptoms. That can make it hard for your doctor to know which one you have , especially if the cyst has broken open.
What is PTA in a popliteal artery?
Percutaneous transluminal angioplasty (PTA) is a less invasive intervention in the treatment of popliteal artery occlusive disease. PTA is indicated for short (< 2 cm) lesions in patients who have claudication and good runoff. Initial enthusiasm for the possibility that stents could improve long-term results of PTA was not supported by subsequent studies. The primary patency rate at 1 year is 65%. However, PTA may be a reasonable alternative to open surgery for limb salvage in patients with prohibitive surgical risks.
Why is clot lysis not routinely initiated?
Because of the high rate of complications from popliteal artery aneurysms (PAAs), medical therapies such as clot lysis are not routinely initiated except to identify an artery for distal anastomosis or when the patient is critically ill and cannot withstand an operation.
What is a stent graft?
Percutaneous endovascular procedures are increasingly being used to treat peripheral artery disease (PAD). Bare-metal, drug-eluting, biodegradable, and covered stents (stent-grafts) are intended to provide enhanced treatment with a reduced risk of the perioperative complications associated with open surgical treatment.
How many stent occlusions were identified at 1-month follow-up?
Five stent occlusions were identified at 1-month follow-up. [ 24] Four occlusions (80%) occurred in the elective group. One stent fracture was noted in an asymptomatic patient. Type I endoleak and type II endoleak were documented in 1 (3.2%) and 3 (10%) cases, respectively. All type II endoleaks occurred in the elective group. Most of the major adverse events, leading to death, occlusion, or reoperation, were documented it the emergency group. The 2-year survival was 93% for the elective group and 73% for the emergency group.
What is the purpose of performing a lower extremity angiography?
In nonemergency cases, performing lower-extremity angiography is important for identifying the site of occlusion, any collateral circulation, and possible target vessels for bypass, as well as for visualizing runoff vessels. If the use of a vein is anticipated, duplex ultrasonography (US) should be performed to assess the caliber and patency of the veins.
What is cilostazol used for?
The advent of cilostazol and its subsequent approval by the US Food and Drug Administration (FDA) represented a significant advance in pharmacologic treatment of patients with intermittent claudication. Cilostazol is a phosphodiesterase III inhibitor with several mechanisms of action.
Is Cilostazol safe to take?
Starting with low doses and then gradually increasing to the recommended dose (100 mg q12hr) may alleviate some of these side effects. Cilostazol is absolutely contraindicated in patients with chronic heart failure of any severity.
What is the best treatment for popliteal cysts?
Your doctor may recommend a corticosteroid medication, such as cortisone. Your doctor will inject this drug into the joint, and the medication will flow back into the cyst. Though it may help relieve the pain, it doesn’t always prevent a popliteal cyst from recurring.
What to do if you have a cyst in your knee?
If the cyst is small, they may compare the affected knee to the healthy one and check your range of motion. Your doctor may recommend noninvasive imaging tests if the cyst rapidly increases in size or causes severe pain or fever. These tests include an MRI or ultrasound.
Why does my knee pop?
Sometimes the knee produces too much of this fluid. The increasing pressure forces the fluid to the back of the knee via a one-way valve, where it creates a bulge . This severe swelling of the knee causes a popliteal cyst to form.
How to prevent a cyst from returning?
Treating the cause of the cyst is very important to prevent the cyst from returning. As a general rule, if the cyst is left alone, it’ll go away once the underlying cause is treated. Should your doctor determine that you have damage to the cartilage, they may recommend surgery to repair or remove it.
How to draw fluid from knee?
Your doctor will insert a needle into the knee joint and may use an ultrasound to help guide the needle to the correct place. They’ll then draw the fluid from the joint.
Can a popliteal cyst be long term?
A pop liteal cyst won’t cause any long-term damage, but it can be uncomfortable and annoying. The symptoms may come and go. In most cases, the condition will improve over time or with surgery. Long-term disability due to a popliteal cyst is very rare.
Can a cyst be removed with arthritis?
If you have arthritis, the cyst may persist even after your doctor treats the underlying cause. If the cyst causes you pain and limits your range of motion, your doctor might recommend surgery to remove it.
How to prevent blood clots in knees?
Compression stockings. These special knee socks reduce the chances that your blood will pool and clot. To help prevent swelling associated with deep vein thrombosis, wear them on your legs from your feet to about the level of your knees. You should wear these stockings during the day for at least two years, if possible.
How to treat DVT?
DVT is most commonly treated with anticoagulants, also called blood thinners. These drugs don't break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots. Blood thinners may be taken by mouth or given by IV or an injection under the skin.
What blood thinners are used for DVT?
The most commonly used injectable blood thinners for DVT are enoxaparin (Lovenox) and fondaparinux (Arixtra). After taking an injectable blood thinner for a few days, your doctor may switch you to a pill. Examples of blood thinners that you swallow include warfarin (Jantoven) and dabigatran (Pradaxa).
What is a clot buster?
Clot busters. Also called thrombolytics, these drugs might be prescribed if you have a more serious type of DVT or PE, or if other medications aren't working.
What blood test is used to diagnose a blood clot?
Tests used to diagnose or rule out a blood clot include: D-dimer blood test. D dimer is a type of protein produced by blood clots. Almost all people with severe DVT have increased blood levels of D dimer. A normal result on a D-dimer test often can help rule out PE. Duplex ultrasound.
How many goals are there for DVT?
There are three main goals to DVT treatment.
What to do if you can't take medicine to thin your blood?
If you can't take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs. Compression stockings. These special knee socks reduce the chances that your blood will pool and clot.
