Procedures
Women typically recover from the cystocele repair in about 4-6 weeks. Women typically recover from the cystocele repair in about 4-6 weeks. They may resume their daily activities, including sexual intercourse, in about 4 weeks after the procedure.
Self-care
Cystocele and rectocele recovery time. 45 minutes to 2 or more hours will take to repair. You can expect to feel better and stronger each day, although you may get tired quickly and need pain medicine for a week or two. You may need about 4 to 6 weeks to fully recover from open surgery and 1 to 2 weeks to recover from laparoscopic surgery or ...
Nutrition
- Rectocele repair (posterior repair)
- Perineorrhaphy (vaginal opening repair)
- Vaginal Vault suspension
- Sacrocolpopexy
- Hysteropexy
How long does it take to recover from cystocele repair?
What to expect in cystocele repair?
- Before the procedure: Inform the physician about your current medications. Eat light meals the evening before the surgery.
- During the procedure: You might be given antibiotics before the start of the surgery. ...
- After the procedure: You may experience discomfort in the vagina for 1-2 weeks following the surgery. ...
What is recovery time after a cystocele?
What are the alternatives to cystocele repair?
How to fix a cystocele?

What is the best treatment for cystocele?
How is a cystocele treated?Activity changes. Avoiding certain activities, such as heavy lifting or straining during bowel movements, that could cause the cystocele to worsen.Kegel exercises. Regular, daily exercises of the pelvic muscles to make them stronger.Pessary. ... Surgery. ... Hormone replacement therapy.
Can a cystocele be corrected without surgery?
In mild cases, non-surgical treatments may be all that is needed to successfully deal with a cystocele. When surgery is performed for more serious cases, some women will eventually need another surgery because the first surgery failed, the cystocele returned or another pelvic floor problem developed.
Can cystocele go away?
Anterior prolapse is treatable. For a mild or moderate prolapse, nonsurgical treatment is often effective. In more severe cases, surgery may be necessary to keep the vagina and other pelvic organs in their proper positions.
How long does it take to recover from cystocele surgery?
Women typically recover from the cystocele repair in about 4-6 weeks. They may resume their daily activities, including sexual intercourse, in about 4 weeks after the procedure.
Is a pessary better than surgery?
Conclusions. In women with POP of stage II or higher undergoing surgery, prolapse symptoms were less severe than in those who were treated with a pessary, but 72% of women who were treated with a pessary did not opt for surgery.
Can you leave a prolapsed bladder untreated?
If prolapse is left untreated, over time it may stay the same or slowly get worse. In rare cases, severe prolapse can cause obstruction of the kidneys or urinary retention (inability to pass urine). This may lead to kidney damage or infection.
Can you live with a cystocele?
Many women contend with pelvic floor problems, including urinary incontinence and pelvic organ prolapse -- when pelvic organs drop due to weakened muscles and tissues.
What does a cystocele feel like to touch?
a dragging discomfort inside your vagina. feeling like there's something coming down into your vagina – it may feel like sitting on a small ball. feeling or seeing a bulge or lump in or coming out of your vagina.
Does Stage 2 cystocele require surgery?
Grade 2 Cystocele This type of cystocele causes major discomfort and severe urinary incontinence. The treatment for this type of cystocele is usually some form of cystocele repair surgery but the cystocele may also be treated with a pessary device.
Is it worth having prolapse surgery?
Consider surgery if the prolapse is causing pain, if you are having problems with your bladder and bowels, or if the prolapse is making it hard for you to do activities you enjoy. An organ can prolapse again after surgery. Surgery in one part of your pelvis can make a prolapse in another part worse.
What kind of doctor does cystocele repair?
A urogynecologist treats these symptoms and conditions and can help you increase your quality of life.
What pessary is used for cystocele?
In patients with a mild cystocele, treatment using a ring with support, a dish with support, a Hodge with support or a donut pessary will suffice. To manage a large prolapse of the anterior vaginal wall, the Gellhorn pessary may be the best choice, although insertion and removal can be difficult.
Treatment for Cystoceles
Specific treatment for cystoceles will be determined by your physician based on:
Clinical Trials
Clinical trials are research studies that evaluate a new medical approach, device, drug, or other treatment. As a Stanford Health Care patient, you may have access to the latest, advanced clinical trials.
What is cystocele in a woman?
What is cystocele? Cystocele is the prolapse of the bladder. Cystocele, or bladder prolapse, is a condition in which the bladder sags down into the vagina due to the weakening of the supporting structure between the bladder and the vagina. Pelvic organ prolapse is a condition in which the structures that support the pelvic organs (the pelvic floor) ...
How to tell if cystocele is a cyst?
The most common symptom is a bulge through the vagina that may be felt or seen. Other symptoms of cystocele may include. Frequent urge to urinate. Inability to empty the bladder. Loss of bladder control or urinary incontinence. Feeling pressure or fullness in the vagina. Discomfort or pain while passing urine.
What is it called when the rectum bulges?
Rectocele: When the rectum (the last part of the large bowel) bulges into the vagina, it is called rectocele. Enterocele: This refers to the bulging of the small bowel against the vaginal wall. This can occur along with vaginal vault prolapse. Depending on the severity, cystocele may be. Grade 1: This is also called mild cystocele.
What is the grade of a cystocele?
Grade 1: This is also called mild cystocele. In this condition, the bladder sags only a short way into the vagina. Grade 2: This is a more severe condition in which the bladder slips down further to reach the opening of the vagina. Grade 3: This is the most severe condition in which the bladder sags so low that it comes out of the vagina.
What are the treatment options for a syphilis?
Treatment options include. Watchful waiting: In the absence of symptoms, the doctor may suggest no treatment. They may keep the patient under observation for the development of any symptoms or complications. Conservative (nonsurgical) therapy: This may include.
What happens after a hysterectomy?
Following hysterectomy, the top of the vagina is repaired to form a vaginal vault. During vault prolapse, the vaginal vault drops down into the vaginal canal. Cystocele: In this condition, the bladder bulges into the vagina.
What is a cystocele in the pelvis?
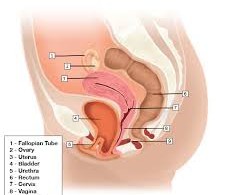
Pelvis with a cystocele (fallen bladder) A cystocele ― also known as a prolapsed, herniated, dropped or fallen bladder ( where your urine or “water” is stored) ― occurs when ligaments that hold your bladder up and the muscle between a woman’s vagina and bladder stretches or weakens, allowing the bladder to sag into the vagina.
What are the grades of cystocele?
There are three grades of cystocele: Grade 1 (mild): The bladder drops only a short way into the vagina. Grade 2 (moderate): The bladder drops to the opening of the vagina. Grade 3 (severe): The bladder bulges through the opening of the vagina. Cleveland Clinic is a non-profit academic medical center.
What is a fallen bladder?
Cystocele (Fallen Bladder) A cystocele occurs when ligaments that hold the bladder up and the muscle between a woman’s vagina and bladder stretches or weakens. Appointments & Access. Contact Us. Overview. Symptoms and Causes. Diagnosis and Tests. Management and Treatment. Prevention.
Why do women need another hysterectomy?
When surgery is performed for more serious cases, some women will eventually need another surgery because the first surgery failed, the cystocele returned or another pelvic floor problem developed. Women who are older, who smoke, are diabetic, or who have had a hysterectomy, may be at higher risk for complications.
Why do you need a pessary in your vagina?
If symptoms are modest, a device called a pessary may be placed in the vagina to hold the bladder in place. Pessaries are available in a number of shapes and sizes to ensure a proper fit. A pessary has to be removed and cleaned on a regular basis in order to avoid infection or ulcers.
What tests are performed to determine bladder function?
The doctor may also perform certain tests, including the following: Urodynamics: Measures the bladder’s ability to hold and release urine. Cystoscopy (cystourethroscopy): A long tube-like instrument is passed through the urethra to examine the bladder and urinary tract for malformations, blockages, tumors, or stones.
Can cystocele cause kidney damage?
If it is not treated at all, the condition can continue to get worse. In the worst cases, the woman may be unable to urinate, which can cause kidney damage or infection.
How to make cystocele worse?
Avoiding certain activities, such as heavy lifting or straining during bowel movements, that could cause the cystocele to worsen. Kegel exercises. Regular, daily exercises of the pelvic muscles to make them stronger. Pessary. This is a device placed in the vagina to hold the bladder in place. Surgery.
What tests are done for cystocele?
Tests for a cystocele may include a pelvic exam and urodynamics, a group of tests to evaluate bladder function. Women with moderate to advanced symptoms may opt for a vaginal pessary, a support device that is inserted into the vagina, or cystocele repair surgery.
What is the test for bladder prolapse?
Other tests may include: Cystourethrogram (also called a voiding cystogram). This is an X-ray of the bladder taken while the woman is urinating and with the bladder and urethra filled with contrast dye. It shows the shape of the bladder and any blockages. MRI can be used to determine the extent of bladder prolapse.
What is it called when the bladder sags?
When the wall between the bladder and the vagina weakens, the bladder may drop or sag into the vagina. This disorder in women is called a cystocele. Cystoceles are grouped into grades:
How to tell if you have cystocele?
Symptoms of cystocele include: Feeling of pelvic heaviness or fullness. Bulge in the vagina that you can feel. Aching or a feeling of pressure in the lower belly or pelvis. Lower back pain. Frequent urinary tract infections. Need to urinate often or urgently. Leakage of urine. Incomplete emptying of the bladder.
What is the best way to move the bladder back into a normal position?
May be used to move the bladder back into a more normal position. Hormone replacement therapy . This may help to strengthen the muscles around the vagina and bladder. If you are thinking about hormone replacement therapy , talk to your healthcare provider about the risks and benefits first.
What are the factors that increase the risk of cystocele?
Factors that increase your risk of a cystocele are childbirth, age, obesity, chronic constipation and heavy lifting. Signs and symptoms can include the feeling that something has dropped out of your vagina, leaking urine or a feeling of incomplete emptying of your bladder. In more advanced cases, the vaginal wall that supports ...
What is a cystocele?
Cystocele is an example of when the tissues between the bladder and vaginal wall weaken causing it to apply pressure on the front vaginal wall and in some cases, drop into the vagina causing pressure on other organs. This can happen when the various muscles and ligaments surrounding the bladder weaken or stretch from childbirth, ...
What is cystocele in isolation?
For the benefit of explanation we will consider cystocele in isolation. A cystocele is a defect of the support of the anterior vaginal wall and is a type of Vaginal Prolapse.
What is a dropped bladder?
It is also referred to as an anterior prolapse as the front (or anterior) vaginal wall has collapsed allowing the bladder to bulge downward into the vagina.
Is a cystocele a defect?
For the benefit of explanation we will consider Cystocele in isolation. A Cystocele is a defect of the support of the anterior vaginal wall and is part of Utero-Vaginal Prolapse.
Understanding Your Treatment Options for a Cystocele
Some degree of pelvic organ prolapse occurs in up to one-third of women in the United States, a quarter of whom experience symptoms . If you find yourself among this group due to a condition called cystocele (a prolapsed bladder) you can take some comfort in knowing you’re in good company.
Cystocele 101
Before we look at our treatment options for a prolapsed bladder, let’s review what cystocele is and how the condition develops. The female pelvic region houses a number of important reproductive, gastrointestinal, and urinary tract organs, all of which are primarily supported by the pelvic floor.
Treating cystocele in its early stages
If you’re just beginning to notice signs of cystocele, the good news is that we can help you strengthen your pelvic floor through targeted exercises, like Kegels. Because your pelvic floor is primarily made up of muscles, exercise is the best way to shore up the support system inside your pelvis.
Treating moderate to severe cystocele
If your cystocele symptoms are affecting your quality of life, our first order of business is to determine the degree to which your bladder has prolapsed. First, we review your symptoms, then we use advanced imaging and specialized testing, including urodynamics, which measures nerve and muscle function , to establish the stage of your cystocele.
Urinary Tract Infection (UTI) Symptoms, Diagnosis, Medication
Bladder infections can be painful and often require medical treatment. Get the latest information on urinary tract infections...
Urinary Incontinence in Women: Types, Causes, and Treatments for Bladder Control
Urinary incontinence in women is a common problem. Overactive bladder (OAB), stress incontinence, and urge incontinence can be...
Why Do I Pee So Often? Incontinence & Overactive Bladder
You went to the bathroom to pee just a few minutes ago. Now you need to go again. What's going on? Here are some possible reasons.
Urinary Incontinence Quiz: Test Your Medical IQ
What is urinary incontinence and why do people develop it? Learn all you need to know with this quiz.
Urinary Incontinence: Foods and Drinks That Cause Overactive Bladder
What causes overactive bladder (OAB)? A natural remedy is to avoid caffeine, alcohol, and these foods. Learn the foods and...
What is it called when the bladder is held in place?
What is Bladder Prolapse? Under normal conditions in women, the bladder is held in place by a "hammock" of supportive pelvic floor muscles and tissue. When these tissues are stretched and/or become weak, the bladder can drop and bulge through this layer and into the vagina. This results in bladder prolapse, also called cystocele.
How to find prolapse?
Prolapse can be found with a clinical history and a pelvic exam. The exam may be done while you are lying down, straining or pushing, or standing. Your health care provider may measure how serious the prolapse is and what parts of the vagina are falling.
Where is surgery done?
Surgery can be performed through the vagina or the abdomen. There are several ways the surgery can be done, they include: Open surgery - when an incision (cut) is made through the abdomen. Minimally invasive surgery - uses small incisions (cuts) in the abdomen.
Can a prolapsed bladder be a cystocele?
This results in bladder prolapse, also called cystocele. In severe cases, the prolapsed bladder can appear at the opening of the vagina. Sometimes it can even protrude (drop) through the vaginal opening. Bladder prolapse is common in women. The symptoms of bladder prolapse can be bothersome but it can be treated.
What is the procedure to repair a cystocele?
The most common surgical procedure to repair a cystocele is anterior vaginal repair, also called anterior colporrhaphy.
How does a cystocele surgery work?
During this procedure, a surgeon puts the bladder back in its normal position and tightens the muscles and tissues that hold the bladder in place using stiches. Your health care professional may perform a procedure to treat or prevent urinary incontinence at the same time as the surgery to repair the cystocele.
What causes cystocele in the vagina?
Weakened or damaged muscles and connective tissues that support the bladder and vaginal walls cause a cystocele. Multiple factors may contribute to the stretching or weakening of these muscles and tissues, including. pregnancy and childbirth, particularly vaginal childbirth.
What is cystocele in a woman?
A cystocele is a condition in which supportive tissues around the bladder and vaginal wall weaken and stretch, allowing the bladder and vaginal wall to fall into the vaginal canal. Usually, the muscles and connective tissues that support the vaginal wall hold the bladder in place. With a cystocele, the muscles and tissues supporting ...
Why do you need to remove a pessary?
Pessaries must be removed and cleaned regularly to prevent vaginal irritation. Your health care professional will show you how to clean and reinsert the pessary on your own. Your health care professional may suggest you use a pessary to help hold your bladder in place and ease your symptoms.
How common is cystocele?
How common is a cystocele? A cystocele is common. Experts estimate that nearly half of women who have given birth have some degree of pelvic organ prolapse. 1 However, many other women with the condition do not have symptoms or do not seek care from a health care professional.
Why do women have a higher risk of having a cystocele?
A cystocele can affect women of any age, but your chances of developing a cystocele increase with age because muscles and tissues often become weaker over time. Other factors that increase your risk of having a cystocele include. giving birth vaginally. having a history of pelvic surgery such as a hysterectomy.
