What is the success rate of maze procedure for atrial fibrillation?
The maze procedure is appropriate for patients with highly symptomatic atrial fibrillation, patients in whom catheter ablation has failed, and patients who have a history of stroke or other blood clots. The success rate is approximately 80% to 90%, varying with patient characteristics.
What is the success rate of atrial fibrillation (AFIB) surgery?
In early studies, the majority of centers reported single procedure success rates of 60% or more for paroxysmal atrial fibrillation and 30% or less for persistent atrial fibrillation.
What is heart surgery for atrial fibrillation (maze)?
Heart Surgery for Atrial Fibrillation (MAZE) 1 Treatment for Atrial Fibrillation. The goals of treatment for atrial fibrillation include regaining... 2 Medical Management of Atrial Fibrillation. 3 Surgical Treatment for Atrial Fibrillation. 4 Evaluation. After the evaluation, the surgeon will discuss your treatment options and together,...
Does the Cox-maze IV procedure improve survival in patients with atrial fibrillation?
Musharbash FN, Schill MR, Sinn LA. et al. Performance of the Cox-maze IV procedure is associated with improved long-term survival in patients with atrial fibrillation undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2018; 155 (1):159–170.
How long does it take for maze procedure to work?
How Long Does It Take for Maze Surgery to Correct an Irregular Heartbeat? Most patients see reduced symptoms within six to eight weeks and a fully corrected heartbeat within three to six months.
How successful is ablation for AFib 2021?
Results from the multicentre investigator-initiated trial found that cryoablation was superior in maintaining freedom from AF, atrial tachycardia and atrial flutter, with 57.1% of patients in the catheter ablation group versus 32.2% in the antiarrhythmic drug group achieving treatment success at 12 months.
What is the most successful treatment for AFib?
Blood thinners (Aspirin and Heparin) can thin the blood and lower the risk of serious complications. Heart rate controlling medicines, such as beta-blockers that include Coreg (Carvedilol) and Lopressor and Toprol (Metoprolol), is the best way to treat AFib.
How successful is AFib 2020 ablation?
“The success rate of a single procedure for recent onset atrial fibrillation is 70-75%. Compare that to the success rate of 30% with drugs. Even if the patient needs a second ablation, it rises to 80-85%, which is much better.”
Is cardiac ablation worth the risk?
Ablation can relieve symptoms and improve the quality of life in people with atrial fibrillation. But it doesn't work for everyone. If atrial fibrillation happens again after the first ablation, you may need to have it done a second time. Repeated ablations have a higher chance of success.
What is the life expectancy after an ablation?
After a single ablation procedure, arrhythmia-free survival rates were 40%, 37%, and 29% at one, two, and five years.
Is a pacemaker better than ablation?
Conclusions: In patients with paroxysmal AF-related tachycardia-bradycardia syndrome, AF ablation seems to be superior to a strategy of pacing plus AAD. Pacemaker implantation can be waived in the majority of patients after a successful ablation.
What is the first drug of choice for atrial fibrillation?
Amiodarone as a first-choice drug for restoring sinus rhythm in patients with atrial fibrillation: a randomized, controlled study. Chest.
What happens if AFib can't be controlled?
AFib can lead to blood clots, which will stop the blood flow through that area. This can cause serious issues like a stroke. A left atrial appendage closure will close off your LAA to keep clots from escaping. This will lower your risk of stroke.
Can an ablation help permanent AFib?
Conclusion: Catheter ablation can be used to cure longstanding permanent AF; however, there is a significant complication rate. Whether this is offset by a mortality benefit associated with sinus rhythm is unknown. Many patients will need more than one procedure to achieve success.
How often does AFib return after ablation?
Although most arrhythmia recurrences typically occur in the first 6 months to 1 year after ablation,5–7 AF recurrences, after initially achieving long-term success, have been reported.
How serious is heart ablation surgery?
In general, cardiac (heart) catheter ablation is a minimally invasive procedure and risks and complications are rare. Catheter ablation may require an overnight stay in the hospital though most patients can return home the same day as the procedure.
How effective is the maze procedure?
Success rates for the maze procedure. The maze procedure as a treatment for AFib is highly effective. The Mayo Clinic estimates that the specialized surgery restores normal function in 75 to 95 percent of those with AFib.
How long does it take to recover from open heart maze surgery?
Most who undergo an open-heart maze can return to work, school, and everyday activities between 8 and 10 weeks after surgery. Mini-maze and cryomaze procedures are minimally invasive, calling for a three- to-four-day hospital stay.
What is the maze procedure?
The maze procedure is a surgical intervention used to treat AFib when medications and other nonsurgical interventions can’t adequately control frequent arrhythmias.
What is the most invasive type of surgery for AFIB?
The open-chest maze procedure is the most invasive type of surgery for AFib. Your doctor makes an incision in your sternum — the bony area that connects the right and left sides of your ribs —to access your heart.
How long before maze surgery can you take blood work?
Preparing for surgery. Preparation for a maze procedure begins a couple of weeks before your surgery date. At this time, you may be asked to stop taking certain medications, such as aspirin and other blood thinners. You may also be asked to stop smoking. You’ll also get blood work to confirm that you’re infection-free.
How does maze surgery work?
Maze surgery destroys tissues that erroneously conduct the electric signals that control the rhythm of the heart. There are three types of maze surgery: This surgery gets its name from a children’s puzzle. The path through which electrical impulses can move in your heart after maze surgery looks like this puzzle.
What is a mini maze?
Mini-maze procedure. Mini-maze is a minimally invasive procedure that accomplishes the same end goal as open-chest surgery. Instead of opening the chest to destroy the tissues that cause episodes of AFib, your doctor makes keyhole incisions on your right side, underneath your armpit.
How many patients underwent the Maze procedure?
The largest study of Maze procedures was conducted on 282 patients who underwent the traditional Maze procedure. In the study, 78% of the patients were in normal sinus rhythm without any anti-arrhythmic medications at 12 months after surgery.
How long does it take to recover from a mini maze?
Because of the minimally invasive nature of the procedure, recovery from a Mini Maze is much less extensive. The average hospital stay after the procedure is 3-4 days, and most patients can return to regular activities with 2-4 weeks.
What is the maze procedure?
The Maze Procedure. Created by Dr. James Cox in 1987, the Maze procedure quickly became the gold standard surgical treatment to eliminate atrial fibrillation. It is also commonly called the “traditional maze,” or the “cut and sew maze” procedure. The Maze procedure is an open-heart surgery.
What are the risks of a maze?
Complications and Recovery for a Maze Surgery. Like all surgeries, the Maze procedure comes with the expected risks. Anesthesia complications, surgical site infections, and post-operative blood clots are all possible complications of this procedure.
How many incisions are made in a mini maze?
The Mini Maze is a minimally invasive or laparoscopic procedure. Instead of opening the chest, three or four small incisions are created in the chest. Long surgical tools are inserted, and the surgery is done via a live video recording. Unfortunately, not everyone is a good candidate for this procedure.
What is the complication rate of convergent surgery?
A recent study reports the complication rate of a convergent procedure is 10%.
How many patients are in sinus rhythm at 12 months?
In a recent article, it was found that of 340 patients who underwent a convergent procedure, at 12 months, 81.9% of patients were in sinus rhythm, while 54.1% of patients were in sinus rhythm while not taking AADs.
What is the Maze procedure?
The Maze procedure is a type of heart surgery used to treat atrial fibrillation. The heart has 4 chambers. There are 2 upper chambers called atria and 2 lower chambers called ventricles. Normally, a specialized group of cells called the sinoatrial (SA) node in the upper right chamber of your heart, or the right atrium, ...
How does a maze procedure work?
In a traditional Maze procedure, the surgeon makes a number of small cuts in the atrium and then sews them back together. The heart’s electrical signal is not able to cross these cuts. The cut area now stops conducting the abnormal signals that caused the atrial fibrillation.
Why do you sleep during a heart maze?
Because the Maze procedure is commonly done in people needing heart surgery for another reason, the surgical process will vary. During a typical open-heart Maze procedure: A doctor will give you anesthesia before the surgery starts. This will cause you to sleep deeply and painlessly during the operation.
How long after maze surgery do you wake up?
After your Maze procedure: When you wake up, you might feel confused at first. You might wake up a couple of hours after the surgery, or a little later. The team will carefully monitor your vital signs, such as your heart rate. They will hook you up to several machines so that you are continuously monitored.
Where does the heartbeat start in atrial fibrillation?
With atrial fibrillation, the signal to start the heartbeat doesn’t begin in the sinoatrial node the way it should. Instead, the signal begins somewhere else in the atria. This causes the atria to quiver or “fibrillate.”. The atria can’t contract normally to move blood to the ventricles.
Does atrial fibrillation cause shortness of breath?
Some people have unpleasant symptoms from atrial fibrillation, like shortness of breath. Atrial fibrillation also greatly increases the risk of stroke. Blood thinners used for preventing stroke pose their own risks, and some medicines require extra blood tests for monitoring.
Can a maze procedure stop fibrillation?
The heart rhythm can therefore return to normal, and the heart can stop fibrillating. Traditionally, the Maze procedure is done as part of an open-heart surgery assisted with a heart-lung machine (cardiopulmonary bypass). Instead of making cuts, doctors can use radiofrequency energy or freeze the tissue to disrupt the abnormal signals.

Definition
Risks
- At one time, atrial fibrillation was thought to be a harmless annoyance. However, atrial fibrillation is now recognized as a dangerous condition. Atrial fibrillation doubles the risk of death. It also increases the risk of stroke five to seven times compared to a person without atrial fibrillation. In addition, atrial fibrillation may cause congestive heart failure and uncomfortable symptoms relat…
Prognosis
- Advances in ablation (both minimal invasive surgical and catheter) offer the possibility of cure to a large number of patients. Patients with untreated preoperative AF (blue lines) have reduced survival. Now, all AF is ablated at the time of heart surgery.
Treatment
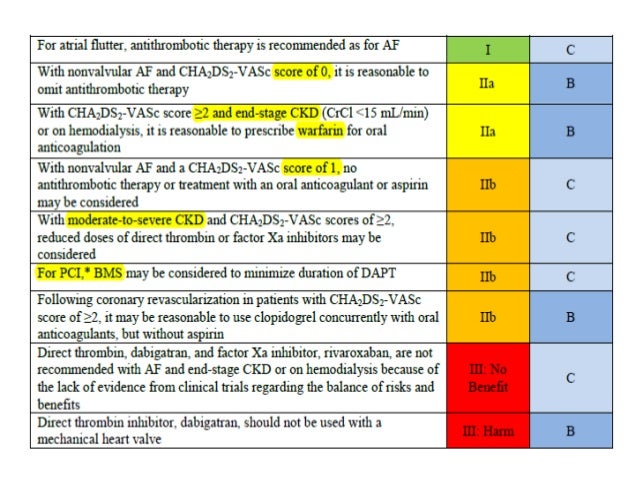
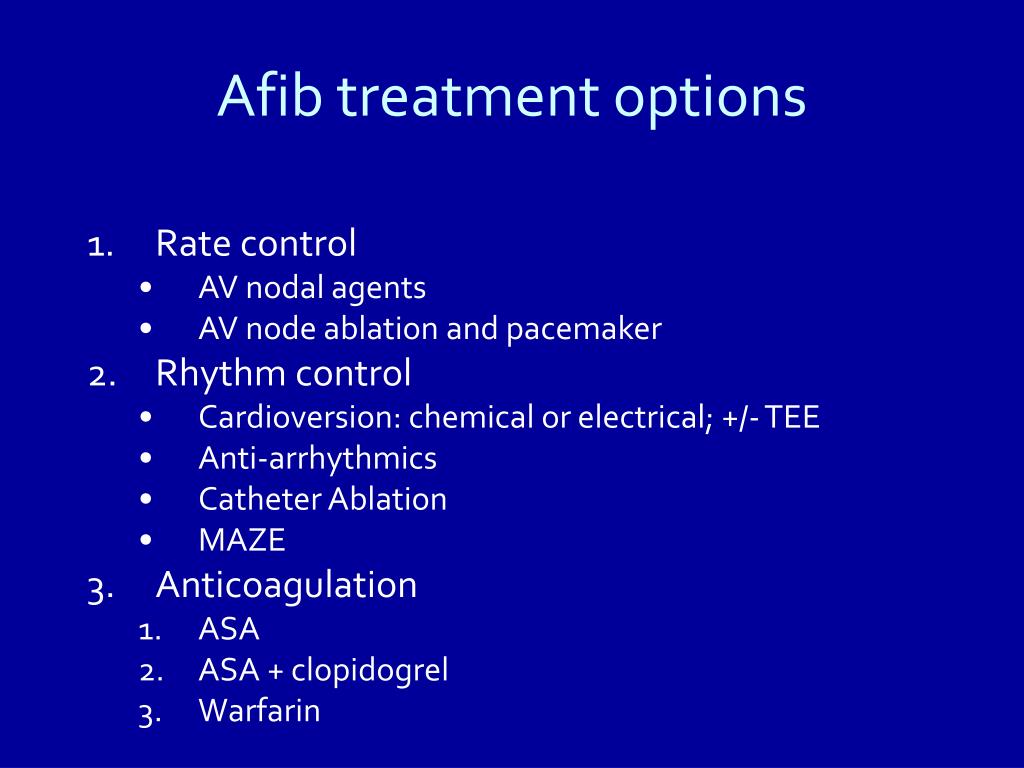
- The goals of treatment for atrial fibrillation include regaining a normal heart rhythm (sinus rhythm), controlling the heart rate, preventing blood clots and reducing the risk of stroke. Initially, medications are used to treat atrial fibrillation. Atrial fibrillation medications may include: Surgical treatment for atrial fibrillation is considered when: Minimally invasive surgery is an option for ma…
Results
- After the evaluation, the surgeon will discuss your treatment options and together, you will determine if you are a candidate for surgery.
Clinical significance
- When patients with AF have valve or bypass surgery, surgeons create a classic Maze lesion set on the heart using either radiofrequency energy or cryothermy. This generally adds 15 minutes to the operative procedure and does not increase operative risk. Sinus rhythm is restored in 75% to 85% of patients, depending upon patient characteristics.